INTRODUCTION
Intraspinal soft tissue lymphangioma is extremely rare. Very few cases of intraspinal lymphangioma have been reported [1-3]. Lymphangioma is pathologically benign harmatomatous proliferation of lymphatic vessels. The causative mechanism remains controversial [4]. The clinical course of the disease is insidious and seldom disappeared spontaneously. To our knowledge, most reported intraspinal lymphangioma cases manifested only pain or minor neurologic sign. We report here one case of intraspinal lymphangioma which caused profound foot drop. Total removal could be achieved by two microscopic surgeries because of initial misdiagnosis as an organized herniated disc fragment.
CASE REPORT
1. Case presentation
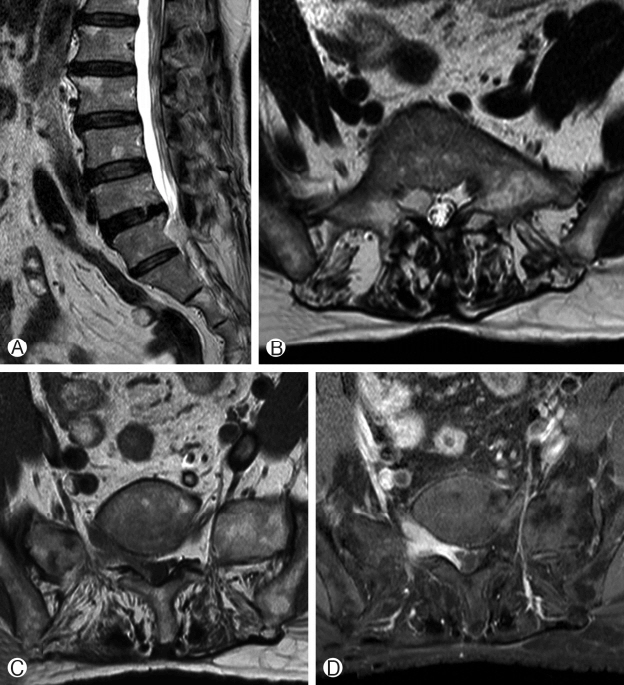
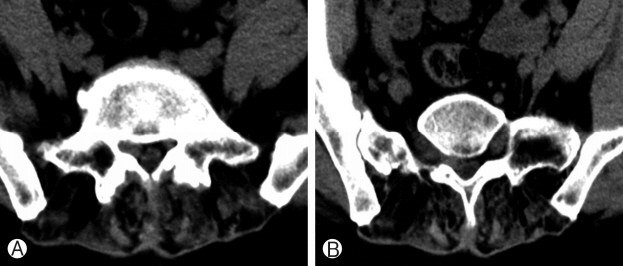
A 62-year-old female patient had been experiencing low back pain and right leg foot drop status since 5 months ago. Physical examination demonstrated mild tenderness of the spinous process of L5. But her neurological status showed a serious painless weakness on the right leg. Ankle dorsiflexion and great toe dorsiflexion motor power was grade 1. Knee jerk was normal, but ankle jerk was trace. Preoperative MRI showed soft tissue mass at the right lumbosacral area (Fig. 1). T1 weighted axial MRI showed soft tissue enhancing mass in L4-5 right lateral recess and epidural space. It was extended to the right L5-S1 foraminal and extraforaminal area with slightly low signal intensity. T2 weighted MRI showed a slightly high-signal intensity mass lesion. It also showed a strong homogeneous gadolinium enhancement on T1 weighted enhanced MRI. CT showed a soft mass without calcified lesion or bony invasion (Fig. 2). The radiological and clinical findings were evaluated by expert radiologists and surgeons. Possible preoperative diagnoses of this epidurally-located, enhancing soft tissue mass by expert radiologist were lymphoma, hemangioma and sequestrated disc material with inflammatory mass.
2. Operation
Although the definite diagnosis was unclear, the patient has a profound neurological deficit and was needed to have decompressive surgery. Therefore, open exploration and thorough decompression was performed. Mass removal was performed through partial hemilaminectomy of L4-5 interlaminar space and foraminotomy of L5-S1 level. The dura mater and the left L5 nerve root had adhered to and were compressed by the mass lesion. It was brown-colored homogenous, gel-like soft tissue mass with thick fibrous capsule. There no vascularity or surrounding neural tissue invasion. The adhesion could be released, and the entire mass was grossly removed. During this procedure, the tumor gradually shrank, although it was tensive at first. The gel-like mass was aspirated in an instant by sucker. Then the fibrotic capsule was removed.
3. Result of Operation and Pathologic Diagnosis
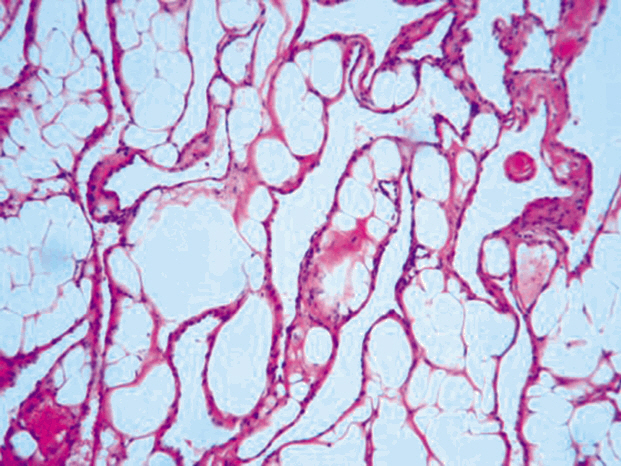
After the surgery, patient’s ankle power was improved from grade 1 to grade 2. However, the histopathologic report revealed lymphangioma. The section contained many thin-walled cavernous structures, whose spaces were mostly empty. These lymphatic channels were lined by normal endothelial cells (Fig. 3). We performed follow-up enhanced MRI after biopsy report. MRI showed remnant mass at the L5-S1 extraforaminal area. Although the L5 root was significantly decompressed, a subsequent paraspinal approach and further removal of tumor mass should be required because of the risk of local recurrence. At the second operation, encapsulated soft tissue remnant mass was found and removed totally. Six months later, the patent still complained mild low back pain, but the motor power of her right ankle and big toe was improved to grade 3. There was no evidence of clinical recurrence or aggravation at the final follow-up visit.
DISCUSSION
Lymphangioma is a benign hamartomatous, proliferation of lymph vessels. The incidence estimated to be around 1 per 10,000 live births. It is composed of fluid filled sacs that result from blockage of the lymphatic system and often associated with karyotype abnormalities such as Turner syndrome. Most common sites are the head and the neck (75%), followed by the proximal extremities, the buttocks, and the trunk. However, they can be found anywhere, including the intestines, the pancreas, the mesentery, and the spine. To the best of our knowledge, this is the first case with spinal lymphangioma causing profound neurologic deficit. Until now, the reported cases showed no definite neurological deficit. The main chief complaints were various pain and sensory change. In our case, tumor growth around the L5 nerve root brought about a profound foot drop. There are no typical clinical features unique to this tumor. It often distributes along the nerves and blood vessels. Therefore, the clinical manifestation depends upon the involved tissue. The radiological findings can offer more important diagnostic information than the clinical features. CT findings demonstrate a low density, poorly-circumscribed cystic mass. Fluid levels may be seen in multiloculated lesion. Usually, it has no distinctive appearance in CT scan. MRI is the most accurate diagnostic tool before histopathological diagnosis. MRI can define the degree of involvement and the entire anatomy of the lesion. It also can help prevent unnecessary extensive, incomplete surgical resection because of the association with a high recurrence rate. In our cases, mass showed low signal intensity on T1-weighted image and high signal intensity on T2-weighted image with homogeneous gadolinium enhancement. However, the definite diagnosis can be made by the pathological findings. On microscopic examination, mass shows thin-wall lumen structures with proliferation of various sized lymphatic vessel lined with endothelial cells (Fig. 3). Due to rarity of the tumor and nonspecific clinical manifestations, it can be misunderstood as other pathological conditions such as disc herniation, arachnoid cyst, hemangioma or inflammation associated fibrous tissue. Therefore, high index of suspicion of tumor is required for adequate diagnosis and treatment. In our case, the first impression was herniated disc fragment with inflammatory change. So, the initial goal of surgery was thorough decompression of the compressed nerve root, not total removal of mass. At the initial surgery, neural decompression was accomplished and the patient’s neurological status was improved. However, the pathologic diagnosis was the lymphangioma which can cause local recurrence later. As for cutaneous lymphangioma, the local recurrences were seen in 12.5% [3]. Therefore, subsequent surgery to remove the remnant mass was required. If we recognized the problem as a tumorous condition, both neural decompression and tumor removal was our goals, and they could have solved at one surgery.
CONCLUSION
Intraspinal soft tissue lymphangioma is very rare. Clinically, it can be confused with other disc fragment or other inflammatory lesion. MRI is the most important diagnostic tool rather than clinical findings. If there is an impression suggesting tumorous lesion, more aggressive evaluation and treatment policy is required.