AbstractObjectiveAlthough the unilateral biportal endoscopy (UBE) technique has remarkable advantages, thoracic laminectomy by UBE is technically difficult and can potentially lead to serious complications. By reviewing previous articles on thoracic laminectomy by UBE, we aimed to identify the complications of thoracic laminectomy by UBE and to establish specific surgical strategies to avoid complications.
MethodsA literature search was performed using the National Center for Biotechnology Information database using the PubMed/MEDLINE search engine. There are 3 published clinical studies in which at least one of these approaches has been performed.
ResultsIn previous articles, several cases of perioperative complications were observed, including spinal cord injury, hyperalgesia, cerebrospinal fluid leakage, headache or neck pain, insufficient decompression, epidural hematoma, subdural hematoma, excessive facet resection, and delayed spinous process fracture.
INTRODUCTIONConventional thoracic laminectomy is the operative treatment for thoracic ossified ligamentum flavum (OLF) or thoracic spinal stenosis [1,2]. However, its clinical outcome is frequently disappointing and often accompanied with complications [3,4]. In a conventional thoracic laminectomy, postoperative complications, including iatrogenic spinal cord injury, dural tear, and postoperative infection, are relatively common [5]. Moreover, it has disadvantages, such as paraspinal muscle atrophy and back pain caused by posterior paraspinal muscle dissection [4,6].
As a result, many alternative surgical techniques were developed, including thoracic decompression with endoscopic guidance [7-13]. Recently, thoracic laminectomy by unilateral biportal endoscopy (UBE) was developed and described by a few studies [7-9]. It demonstrated several advantages as compared to conventional thoracic laminectomy and has been shown to have favorable clinical outcomes [7,9]. Although the UBE technique has remarkable advantages, thoracic laminectomy by UBE is technically difficult and can potentially lead to serious complications.
By reviewing previous articles on thoracic laminectomy by UBE, we aimed to identify the complications of thoracic laminectomy by UBE in patients with thoracic OLF or thoracic spinal stenosis and to establish specific surgical strategies to avoid complications. Furthermore, we sought to demonstrate the indications for thoracic laminectomy by UBE and to discuss the surgical techniques.
MATERIALS AND METHODSEligible studies included in which patients underwent thoracic laminectomy by UBE due to thoracic OLF or thoracic spinal stenosis. Inclusion criteria were studies of human subjects published in the English language. Studies that did not include clinical outcomes or postoperative complications as outcome variables were excluded. Abstracts, case reports, editorials and expert opinions were excluded. Criteria used in this review for article selection were: (1) surgically managed thoracic pathology using UBE techniques, (2) average follow-up period no less than 1 year, (3) pertaining to postoperative complication.
A literature search was performed using the National Center for Biotechnology Information database using the PubMed/MEDLINE search engine. The keywords used in this search were “unilateral biportal endoscopy,” “thoracic,” and “biportal.” The Medline and Scopus databases were used to identify relevant studies published in English. While reviewing the literature, articles on endoscopic thoracic spine surgery were retrieved through the abovementioned search. We emphasize ways to avoid and manage the approach-related morbidity. There are 3 published clinical studies in which at least one of these approaches has been performed (Table 1). Table 2 summarizes the surgery-related complications reported in a series of trials.
The indications and contraindications for thoracic laminectomy by UBE are as follows [7-9]: (1) thoracic OLF and (2) thoracic spinal stenosis. The contraindications of thoracic laminectomy by UBE are as follows: (1) soft or calcified disc herniation, (2) severe ossified posterior longitudinal ligament, (3) spinal column instability, and (4) high-grade deformity.
RESULTSThree articles reported on posterior thoracic decompression by UBE (Table 1) [7-9]. The overall complications associated with thoracic laminectomy by UBE are shown in Table 2. The first article was a previous technical article that described about the OLF’s removal by UBE technique [8]. The other 2 articles presented the surgical techniques and described preliminary clinical outcomes [7,9]. Deng et al. [7] described posterior thoracic decompression by UBE in 14 patients with 1-level thoracic OLF. They presented favorable clinical outcomes in terms of thoracic decompression by UBE with an average follow-up of 15.4 months. Five cases of perioperative complications were noted (1 patient with cerebrospinal fluid leakage [CSF, 7.1%], 2 with headaches and neck pain [14.3%], and 2 with hyperalgesia of lower limbs [14.3%]). One patient with CSF was treated by maintaining a prone position for 5 days. Headache and neck pain happened in 2 patients, which disappeared in 2 days. Hyperalgesia of the lower limbs in 2 patients was relieved after conservative treatment in 1–3 weeks.
Kim et al. [9] described posterior thoracic decompression by UBE in 16 patients with single (11 cases) or 2-level (5 cases) thoracic OLF. Nine cases of perioperative complications were observed, including 2 cases of cord injury, 1 case of insufficient decompression, 1 case of subdural hematoma, 1 case of epidural hematoma, 3 cases of delayed spinous process fracture, and 1 case of facet joint violation. Of the 2 patients with iatrogenic cord injury, 1 patient recovered quickly, whereas the other patient did not improved and required assistance in ambulation at the last follow-up. Two patients had subdural and epidural hematoma, which were managed by conservative treatment. Excessive facet resection in 1 patient and spinous process fracture in 3 patients happened at the T2–3 and T3–4 levels; however, these complications did not cause mechanical back pain and segmental instability during the follow-up duration.
1. Dural TearDural tear is the most common complication of thoracic OLF removal, especially when the case have a dural ossifcation [4,14]. In a series of 14 cases by using the UBE technique, Deng et al. [7] demonstrated one case of CSF leakage (7.1%). Kim et al. [9] also described no case of CSF leakage in their series of patients treated by UBE, which differ from the data reported in previous studies.
2. Postoperative HematomaUncontrolled epidural bleeding might cause symptomatic epidural hematoma, which sometimes requires revision surgery. In a series of 16 cases, Kim et al. [9] reported one case of epidural hematoma, which was managed by conservative treatment.
3. Iatrogenic Cord InjuryIatrogenic cord injury is another seriouis complication of thoracic surgery both in endoscopic and conventional surgeries [15]. The manipulation of the thoracic spinal cord with endoscope or instruments raised the risk of cord injury; therefore, thoracic laminectomy should be performed with caution to avoid mechanical injury. In thoracic laminectomy by UBE, the procedure could be related to cord injury by the use of an endoscope or surgical instruments and thermal injury generated by the overuse of the radiofrequency (RF) probe. In a previous report, 2 patients developed hyperalgesia, which was relieved after conservative treatment for 1–3 weeks [7]. Similarly, Kim et al. [9] reported 2 complications of cord injury in a patient who had undergone thoracic laminectomy by UBE. They mentioned that the “inside-out piecemeal removal of OLF” method could repeatedly cause mechnical injury to the spinal cord, leading to iatrogenic spinal cord injuries.
5. Other ComplicationsThe other complications included postoperative spinous process fracture and excessive facet resection. Kim et al. [9] reported on cases of as spinous process fracture and excessvie facet resection following a thoracic laminectomy by UBE. The upper thoracic vertebrae have relatively smaller lamina, facet joints, and short spinous processes. Therefore, during bilateral decompression from the unilateral side of the upper thoracic level, the preservation of the spinous process and the contralateral lamina may be technically more challenging [9]. Although spinous process fracture do not occur immediately after surgery, delayed spinous process fractures can occur as the thinned bone is subjected to continuous mechanical stress. However, these complications did not cause mechanical back pain and segmental instability during the follow-up period. Given that the posterior musculo-ligamentous complex could be preserved using the UBE technique, complications, such as mechanical pain or postoperative instability, are thought to be mild.
DISCUSSSIONThe thoracic laminectomy by UBE has the following distinct advantages over the conventional surgery for thoracic patholgy: (1) the UBE technique may provide appropriate decompression with minimal musculoligamentous injury or facet joint violation [7,9]; (2) the endoscope and various instruments could be moved independently, which makes the procedure more comfortable and easy as compared to other endoscopic procedures [17]; and (3) surgery can be performed under a highly magnified and clear operative view with saline irrigation [18]. Therefore, UBE technique can achieve exact thoracic decompression while lowering the risk of complications.
Based on the results of 2 previous studies, thoracic laminectomy by UBE may be associated with fewer potential complications [7,9]. Severe water-related complications, including epidural fluid collection and raised intracranial pressure, were not observed. However, these studies have some limitations. Firstly, severe OLF cases, such as tuberous-type OLF or severe dural ossification, might be excluded, that may cause a bias of complications. Second, 2 studies evaluated the clinical outcomes based on the results obtained within the 2-year follow-up.
The management of dural tear is well known, which typically involves a combination of fibrin collagen patch (TachoComb, CSL Behring, Tokyo, Japan) and bedrest of 3–5 days (Figure 1) [18]. Howevere, when the dural tear is too large that the fibrin collagen patch cannot cover it, conventional surgery should be performed to perform dural suturing; subsequently, a lumbar drain could be placed. The severe adhesion of the OLF to the dura sac or dural ossification, which has a high risk of dural tear, is a complication. Preoperative CT combined with MRI should be examined for the presence of dural ossification with the dural matter to prevent this complication. In such cases, it is suggested that a thinned calcified lesion be left against the dural sac.
To prevent postoperative hematoma when performing thoracic laminectomy by UBE, some principles should be pursued. Bleeding from the removed bone surface should apply bone wax to prevent the risk of hematoma (Figure 2A). Prior to Ligamentum flavum (LF) resection, the use of the RF probe and hemostatic agents (Gelfoam [Gelfoam, Pharmacia & Upjohn, Kalamazoo, MI] or Wound Clot [Core scientific creations, Israel]) is effective to control bleeding. Focal epidural bleeding from the epidural vessel can be controlled by using an RF probe (Figure 2B). For epidural bleeding whose bleeding focus is not clear, the use of hemostatic agents (Gelfoam or WoundClot) could be helpful (Figure 2C). To reduce the risk for postoperative hematoma, the use of a Jackson-Pratt surgical drain (100 mL) is recommended to be placed through the working portal for 1 or 2 days.
Since the thoracic cord is vulnerable to mechanical compression, thoracic laminectomy by UBE should be performed carefully to prevent iatrogenic spinal cord injury. The prevention of iagrogenic cord injury is based on several recommendations, which are as follows: (1) when bone working is achieved, care should be taken to protect the thoracic spinal cord while saving the LF; (2) removal of the base of the spinous process should be required to obtain an unobstructed view and to assist in positioning the scope and instruments at the contralateral side; (3) it is recommended to thin the OLF with a diamond burr through the OLF into a translucent type (Figure 3A). The paper-thin OLF can be safely detached with a freer elevator or fine pituitary forceps, and its removal reduces the risk of additional neural injury (Figure 3B); (4) if removing the OLF is dangerous due to dural ossification or severe adhesion, it is recommended to remain the thinned OLF. The dural defect should be thoroughly applied with a fibrin collagen patch after the OLF has been floated; and (5) intraoperative electrophysiological monitoring is required to detect iatrogenic spinal cord inury during operation [9].
The reported water-related complications were minor; however, serious complications could be possible. Therefore, it is necessary to monitor the fluid output and complications due to the poor fluid output, which can be prevented by using a retractor or a working sheath.
This study has several limitations. First, only a few case series with short follow-up periods have been published on biportal endoscopic thoracic surgery. Second, 3 articles reviewed were all retrospective study, thus the inherent weakness and limitation of all retrospective studies would be expected.
CONCLUSIONUBE technique in thoracic spine surgery is a viable, effective, and minimally invasive treatment option that, when performed by experienced surgeons, provides favorable clinical outcomes for select patients. UBE technique has remarkable advantages, but endoscopic thoracic surgery is technically challenging and has the potential to cause serious complications. For avoidable complications, surgeons should be familiar with prevention methods and pitfalls to minimize complications.
Figure 1.The management of dural tear by fibrin collagen patch (TachoComb, CSL Behring, Tokyo, Japan). 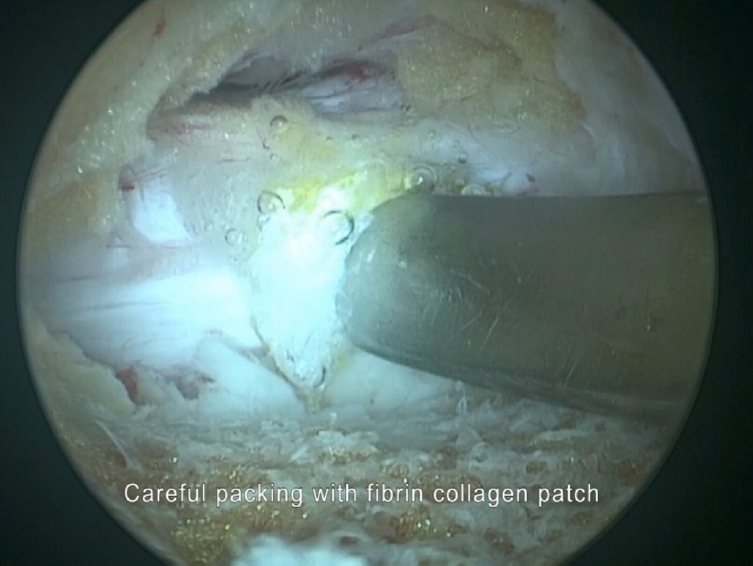
Figure 2.Bleeding control when performing thoracic laminectomy by unilateral biportal endoscopy. (A) Bleeding from the removed bone surface should apply bone wax to prevent the risk of hematoma. (B) Focal epidural bleeding from the epidural vessel can be controlled by using an radiofrequency probe. (C) For epidural bleeding whose bleeding focus is not clear, the use of hemostatic agents (Gelfoam or WoundClot) could be helpful. 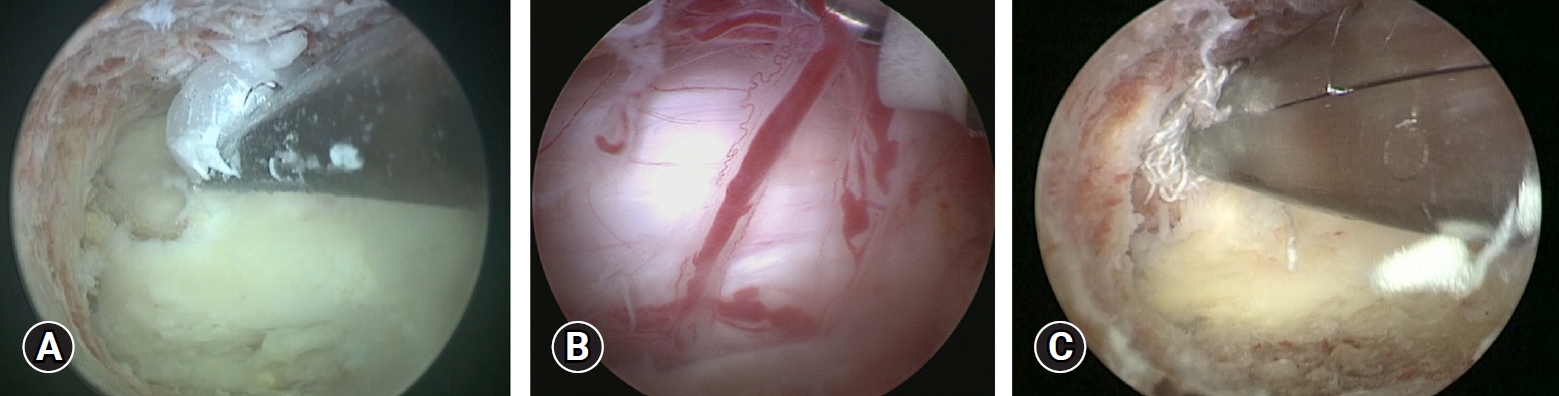
Figure 3.The prevention of iatrogenic cord injury in thoracic laminectomy by unilateral biportal endoscopy. (A) It is recommended to thin the ossified ligamentum flavum (OLF) with a diamond burr through the OLF into a translucent type. (B) The paper-thin OLF can be safely detached with a Freer elevator. 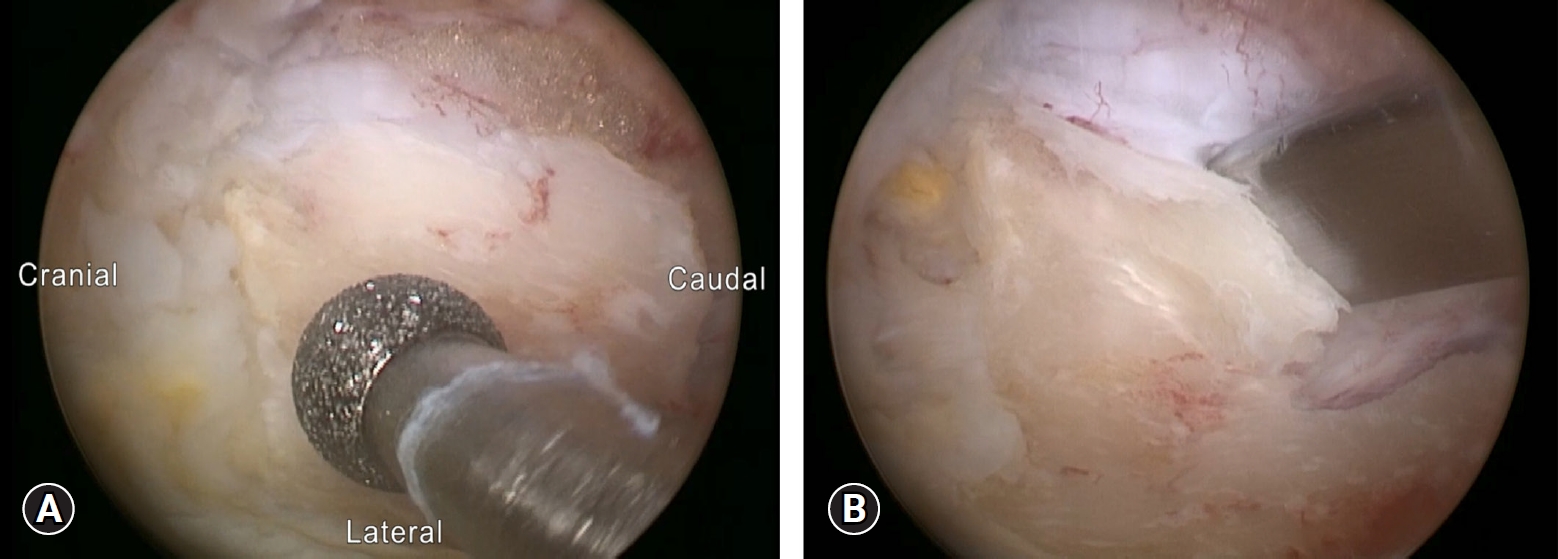
Table 1.Summary of the included studies on thoracic laminectomy by unilateral biportal endoscopy
Table 2.Complications reported in thoracic laminectomy by unilateral biportal endoscopy
REFERENCES1. Palumbo MA, Hilibrand AS, Hart RA, Bohlman HH. Surgical treatment of thoracic spinal stenosis: a 2- to 9-year follow-up. Spine (Phila Pa 1976) 2001;26:558–66.
2. Jia LS, Chen XS, Zhou SY, Shao J, Zhu W. En bloc resection of lamina and ossified ligamentum flavum in the treatment of thoracic ossification of the ligamentum flavum. Neurosurgery 2010;66:1181–6.
4. Osman NS, Cheung ZB, Hussain AK, Phan K, Arvind V, Vig KS, et al. Outcomes and complications following laminectomy alone for thoracic myelopathy due to ossified ligamentum flavum: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2018;43:E842–8.
5. Ahn DK, Lee S, Moon SH, Boo KH, Chang BK, Lee JI. Ossification of the ligamentum flavum. Asian Spine J 2014;8:89–96.
6. Okada K, Oka S, Tohge K, Ono K, Yonenobu K, Hosoya T. Thoracic myelopathy caused by ossification of the ligamentum flavum. Clinicopathologic study and surgical treatment. Spine (Phila Pa 1976) 1991;16:280–7.
7. Deng Y, Yang M, Xia C, Chen Y, Xie Z. Unilateral biportal endoscopic decompression for symptomatic thoracic ossification of the ligamentum flavum: a case control study. Int Orthop 2022;46:2071–80.
8. Kang MS, Chung HJ, You KH, Park HJ. How I do it: biportal endoscopic thoracic decompression for ossification of the ligamentum flavum. Acta Neurochir (Wien) 2022;164:43–7.
9. Kim JY, Ha JS, Lee CK, Lee DC, Hong HJ, Choi SY, et al. Biportal endoscopic posterior thoracic laminectomy for thoracic spondylotic myelopathy caused by ossification of the ligamentum flavum: technical developments and outcomes. Neurospine 2023;20:129–40.
10. Ikuta K, Tarukado K, Senba H, Kitamura T, Komiya N, Fukutoku Y, et al. Decompression procedure using a microendoscopic technique for thoracic myelopathy caused by ossification of the ligamentum flavum. Minim Invasive Neurosurg 2011;54:271–3.
11. An B, Li XC, Zhou CP, Wang BS, Gao HR, Ma HJ, et al. Percutaneous full endoscopic posterior decompression of thoracic myelopathy caused by ossification of the ligamentum flavum. Eur Spine J 2019;28:492–501.
12. Ruetten S, Hahn P, Oezdemir S, Baraliakos X, Merk H, Godolias G, et al. Full-endoscopic uniportal decompression in disc herniations and stenosis of the thoracic spine using the interlaminar, extraforaminal, or transthoracic retropleural approach. J Neurosurg Spine 2018;29:157–68.
13. Kim HS, Wu PH, Kim JY, Lee YJ, Kim DH, Lee JH, et al. Comparative clinical and radiographic cohort study: uniportal thoracic endoscopic laminotomy with bilateral decompression by using the 1-block resection technique and thoracic open laminotomy with bilateral decompression for thoracic ossified ligamentum flavum. Oper Neurosurg (Hagerstown) 2022;22:391–9.
14. Yang Z, Xue Y, Zhang C, Dai Q, Zhou H. Surgical treatment of ossification of the ligamentum flavum associated with dural ossification in the thoracic spine. J Clin Neurosci 2013;20:212–6.
15. Dommisse GF. The blood supply of the spinal cord. A critical vascular zone in spinal surgery. J Bone Joint Surg Br 1974;56:225–35.
16. Choi G, Kang HY, Modi HN, Prada N, Nicolau RJ, Joh JY, et al. Risk of developing seizure after percutaneous endoscopic lumbar discectomy. J Spinal Disord Tech 2011;24:83–92.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||