AbstractLumbar disc herniations (LDHs) located in foraminal lesions are difficult to approach using the normal posterior approach while preserving the facet joints. The translaminar approach (TLA) of fully endoscopic spine surgery allows access to a foraminal lesion through a small fenestration on the isthmus of the vertebral lamina, thereby preventing facet joint destruction. TLA is particularly suitable for L5/S1 foraminal LDH cases where the transverse diameter of the foramen is anatomically long. From 2020 to 2022, TLA was performed in 17 patients with foraminal LDH (12 men and 5 women), with a mean age of 67 years. The operative levels were L3/4 in 1 case, L4/5 in 2 cases, and L5/S1 in 14 cases. The mean operative time was 72 minutes, and the mean blood loss was negligible in all patients. The mean postoperative hospital stay was 1.2 days, and no major complications occurred. The mean preoperative and postoperative Numerical Rating Scale scores for leg pain were 6.4 and 1.8, respectively, and the mean patient satisfaction score at 3 months after TLA was 7. In conclusion, TLA is a minimally invasive approach for foraminal LDH, with particular advantages for facet joint preservation.
INTRODUCTIONForaminal and extraforaminal lumbar disc herniations (LDHs) have been reported to account for 6.5% to 12% of all LDH cases [1-3]. Compression of the spinal nerve and dorsal root ganglion may occur, causing severe pain that is often unresponsive to conservative management, requiring surgery [3].
Foraminal LDH are located ventral to the facet joints, making them difficult to approach using a normal posterior approach while preserving the facet joints, possibly resulting in postoperative instability. Although various modifications of standard open and microsurgical techniques have been described for foraminal LDH [1,2,4,5], endoscopically approaching the foraminal lesions allows for facet joint preservation. There are 2 types of approaches: the transforaminal approach (TFA), which is accessed from approximately 8–12 cm lateral to the midline, and the translaminar approach (TLA), which is accessed by creating a small fenestration on the isthmus of the vertebral lamina. This article outlines the key points for foraminal LDH removal using full-endoscopic TLA.
MATERIALS AND METHODS1. IndicationTLA to access foraminal lesions, such as disc herniation and foraminal stenosis, is particularly effective for foraminal LDH protruding from the medial part of the foramen at the L5/S1 level [6-8]. Because the transverse diameter of the L5/S1 foramen is anatomically long, it is relatively difficult. Furthermore, the iliac crest frequently disturbs disc puncture, which is an initial step in TFA. TFA for foraminal LDH is more challenging than for other vertebral levels.
Between 2020 and 2022, 896 full-endoscopic surgeries for LDH were performed at Iwai Orthopaedic Hospital. Among these, TLA was used in 17 patients with foraminal LDH.
The patients’ background data, including age, sex, length of hospital stay, operation time, blood loss, surgical levels, Numerical Rating Scale (NRS) for leg pain at admission and discharge, and postoperative subjective satisfaction score (ranging from 1 [low satisfaction] to 10 [extreme satisfaction]), were retrospectively assessed at 3-month postsurgery.
2. Surgical Procedure1) Anesthesia and skin markingAfter induction of general anesthesia, the patients were placed in the prone position. Muscle relaxants were reversed and motor-evoked potential (MEP) monitoring was initiated. A fluoroscope centered across the operating table ensured appropriate positioning. An 8-mm skin incision was made 15–20 mm lateral to the midline. Although it can improve the intraoperative orientation, discography was not performed in all cases, as the puncture points differed.
2) Insertion of endoscopeThe obturator was positioned on the lamina dorsal surface. As fenestration is mainly performed in the isthmus of the lamina, the obturator was inserted parallel to the endplate at the level of the foramen while monitoring lateral fluoroscopy. A 7-mm diameter working sheath was placed at the deepest insertion site at a 30° angle (Figure 1A, B). Subsequently, an endoscope with a working channel diameter of 4.1 mm is introduced (RIWOspine GmbH, Knittlingen, Germany).
3) Surgical procedure (endoscopic manipulation)After inserting the endoscope, forceps and a bipolar radiofrequency electrode system (Elliquence, Baldwin, NY, USA) were used to expose the isthmus of the lamina. Instrument positioning was confirmed using a lateral fluoroscopic view. The lamina was thinned using a 3.5-mm diameter (NSK-Nakanishi Japan, Tokyo, Japan) diamond bar on a high-speed drill. The area of bone resection should be approximately 10 × 10 mm instead of focusing on a single deep point. Cases of severe degeneration may require drilling the tip of the inferior articular process of the rostral lamina. After exposing the inner cortical bone of the lamina, resection of the inner cortical bone began at the site covering the superior articular process (SAP) to provide guidance and ensure safe progression (Figure 2A). After SAP resection, the vertebral disc underneath was visible (Figure 2B) and could be subsequently removed.
4) Final checking pointAfter successfully performing the discectomy, the decompressed nerve root became visible (Figure 2C). Decompression of the nerve root may increase the MEP response in the corresponding nerve root region. No drains were placed and bedrest was not required 3-hour postsurgery. The patient was discharged on the following day. Preoperative magnetic resonance imaging (Figure 3A, B) and postoperative computed tomography demonstrating the extent of bone removal in the left L5/S1 foraminal LDH (Figure 4A–C) are shown.
RESULTSOf the 17 patients, 12 were men and 5 were women (mean age, 67 years). The operative levels were L3/4 in 1 case, L4/5 in 2 cases, and L5/S1 in 14 cases. The mean operative time was 72 minutes; blood loss was negligible in all patients. The average postoperative stay was 1.2 days, and there were no major complications. The mean pre- and postoperative NRS for leg pain improved from 6.4 to 1.8. The mean patient satisfaction score was 7 (Table 1).
DISCUSSIONDiscectomy for foraminal LDH reportedly has a higher postoperative incidence of residual radicular pain and paresthesia than central LDH due to direct compression of the dorsal root ganglion [9].
Upward migrated LDH to the axilla of the exiting nerve has been termed the “hidden zone’’ by Macnab in 1971, and accounts for 10% of patients with extruded LDH [10]. Preservation of the facet joints with the conventional posterior approach is challenging, and postoperative instability can be a concern.
The TLA was developed to approach the hidden zone directly from above by creating a window in the isthmus part of the lamina. Many reports exist using the transpars approach using the open technique by Di Lorenzo et al. [4] in 1998, as well as reports utilizing the caspase retractor, tubular retractor under the microscope, and endoscopic techniques [5,11]. Currently, an 8-mm full-endoscopic surgery is considered the least invasive technique [12-16].
The endoscope has a 25° angle at its tip, allowing for a wider osteotomy of the deeper layers compared to the superficial layers. This enables preservation of the medial and lateral lamina, thereby preventing iatrogenic spondylolisthesis.
The TFA for foraminal lesions is also effective [17]; however, accessing the medial side of the foramen at the L5/S1 level is challenging because of the iliac crest. Accessing the foramen in patients with degenerative narrowing of the L5 transverse process and sacral alar is also difficult. In such cases, the TLA is more suitable than the TFA.
TLA is also useful for accessing the hidden zone at L4/5 and higher; although, iatrogenic spondylolisthesis due to excessive bone resection is possible, as the width of the isthmus becomes narrower anatomically at higher lumbar levels.
The average age of the patients in this study was slightly higher and many had mild foraminal stenosis. TLA can also enlarge the corresponding foramen in cases of foraminal stenosis by drilling the SAP [6-8].
Extraforaminal lesions are unsuitable for use in TLA because they are inaccessible. The posterolateral approach, which is accessed 5–8 cm lateral to the midline, is appropriate for extraforaminal pathologies. Therefore, an accurate preoperative diagnosis of the nerve root compression location using imaging and electrophysiological studies is crucial.
TLA is a minimally invasive approach to reach the foraminal lesion; however, it should only be performed after mastery of the usual endoscopic approach techniques, as the lack of anatomical landmarks is challenging for beginners in endoscopic surgery.
Figure 2.Intraoperative image of left L5/S1 fully endoscopic discectomy via the translaminar approach. (A) Exposure of the superior articular process (SAP) after removal of the inferior articular process (IAP). (B) Exposure of the disc herniation (DH) after removal of SAP. (C) Decompressed nerve root (NR) visible after removal of the DH. 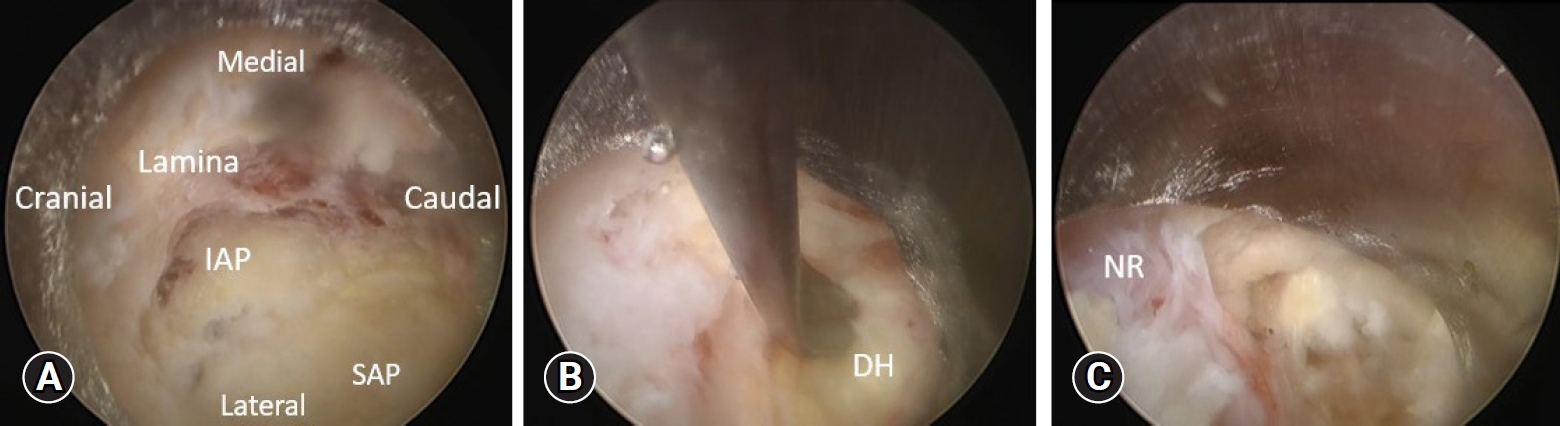
Figure 3.Preoperative magnetic resonance image showing left L5/S1 foraminal stenosis. (A) Sagittal view. (B) Axial view. 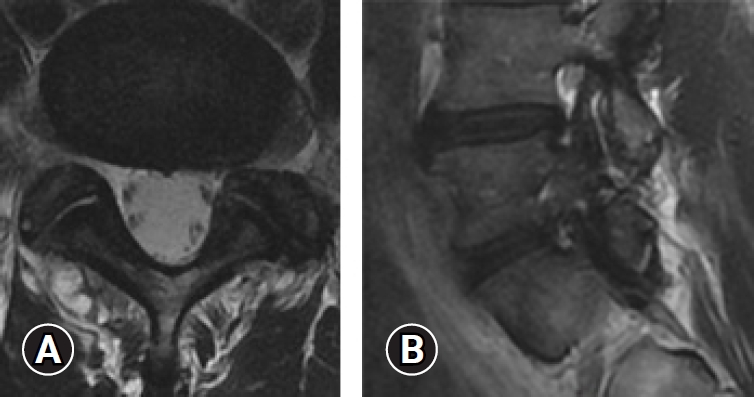
Figure 4.Postoperative computed tomography showing the range of bone removal. (A) Sagittal view. (B) Axial view. (C) Three-dimensional view. Arrowheads indicate the areas of removed bone. 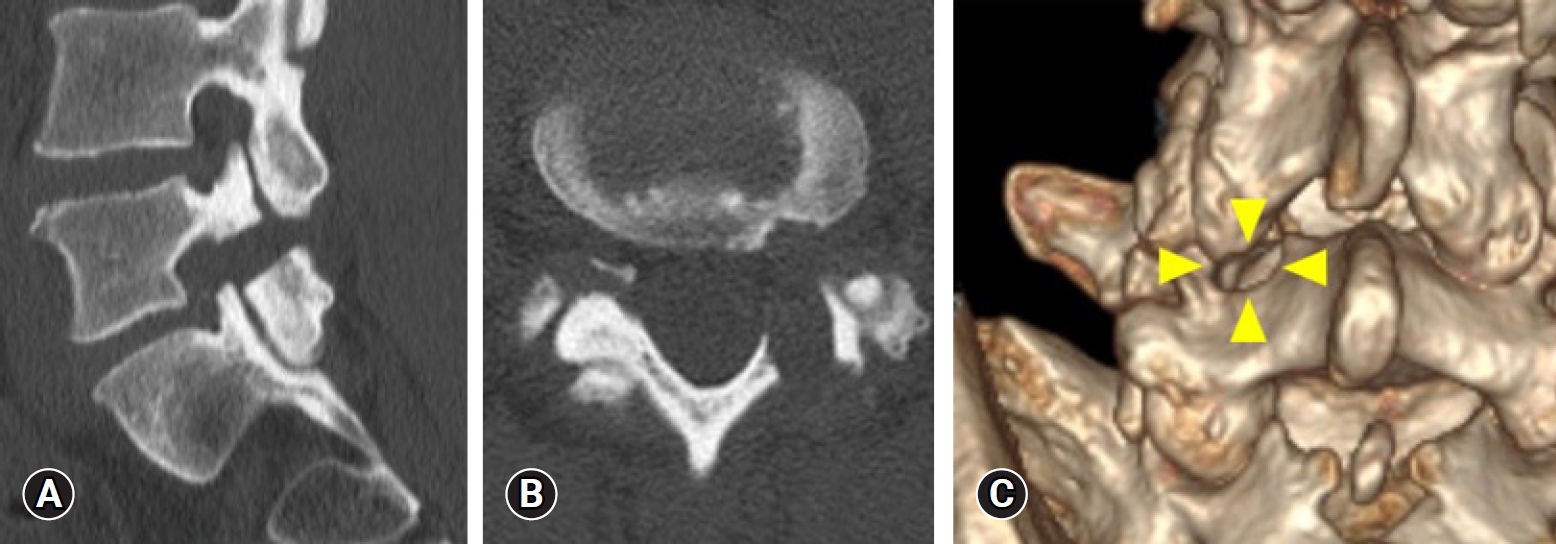
Table 1.Summary of 17 cases REFERENCES1. Epstein NE. Foraminal and far lateral lumbar disc herniations: surgical alternatives and outcome measures. Spinal Cord 2002;40:491–500.
2. Siebner HR, Faulhauer K. Frequency and specific surgical management of far lateral lumbar disc herniations. Acta Neurochir (Wien) 1990;105:123–31.
3. Berra LV, Rita AD, Longhitano F, Mailland E, Reganati P, Frati A, et al. Far lateral lumbar disc herniation part 1:Imaging, neurophysiology and clinical features. World J Orthop 2021;12:961–9.
4. Di Lorenzo N, Porta F, Onnis G, Cannas A, Arbau G, Maleci A. Pars interarticularis fenestration in the treatment of foraminal lumbar disc herniation:a further surgical approach. Neurosurgery 1998;42:87–9.
5. Abdelrahman H, Seyed-Emadaldin S, Krajnovic B, Ezzati Ali, Abdelgawaad AS. Trans-tubular translaminar microscopic-assisted nucleotomy for lumbar disc herniations in the hidden zone. Global Spine J 2022;12:1420–7.
6. Fujita M, Inui T, Oshima Y, Iwai H, Inanami H, Koga H. Comparison of outcomes of lumbar interbody fusion and full-endoscopic laminectomy for L5 radiculopathy caused by lumbar foraminal stenosis. Neurol Med Chir (Tokyo) 2022;62:270–7.
7. Ishibashi K, Oshima Y, Inoue H, Takano Y, Iwai H, Inanami H, et al. A less invasive surgery using a full-endoscopic system for L5 nerve root compression caused by lumbar foraminal stenosis. J Spine Surg 2018;4:594–601.
8. Koga H. Improved percutaneous endoscopic translaminar approach for foraminal stenosis at L5/S1. Mini-invasive Surg 2017;1:3–5.
9. Maio K, Yoshida M. Clinical outcomes of microendoscopic discectomy for extraforaminal lumbar disc herniation. In: Dezawa A, Chen PQ, Chung JY, editors. State of the art for minimally invasive spine surgery. Tokyo: Springer; 2005. p. 35–42.
10. Macnab I. Negative disc exploration:an analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 1971;53:891–903.
11. Ikuta K, Tono O, Senba H, Kitamura T, Komiya N, Oga M, et al. Translaminar microendoscopic herniotomy for cranially migrated lumbar disc herniations encroaching on the exiting nerve root in the preforaminal and foraminal zones. Asian Spine J 2013;7:190–5.
12. Xin Z, Liao W, Ao J, Qin J, Chen F, Ye Z, et al. A modified translaminar osseous channel-assisted percutaneous endoscopic lumbar discectomy for highly migrated and sequestrated disc herniations of the upper lumbar: clinical outcomes, surgical indications, and technical considerations. Biomed Res Int 2017;2017:3069575.
13. Dezawa A, Mikami H, Sairyo K. Percutaneous endoscopic translaminar approach for herniated nucleus pulposus in the hidden zone of the lumbar spine. Asian J Endosc Surg 2012;5:200–3.
14. Khandge AV, Kim JS. Modified interlaminar endoscopic lumbar discectomy for highly upmigrated disc herniation:a proctorship description of the technique via translaminar route. Neurospine 2020;17(Suppl 1):S66–73.
15. Du J, Tang X, Jing X, Li N, Wang Y, Zhang X. Outcomes of percutaneous endoscopic lumbar discectomy via a translaminar approach, especially for soft, highly down-migrated lumbar disc herniation. Int Orthop 2016;40:1247–52.
|
|
|||||||||||||||||||||||||||||||||||||