Mahesha: Transforaminal Endoscopic Drainage of Massive Anterior Epidural Abscess-Novel Technique
Abstract
A 54 year old female presented with recent onset of fever, back pain, radicular pain with bowel and bladder paralysis. Magnetic resonance imaging with contrast revealed a massive anterior spinal epidural abscess extending from D10 to L4 with osteomyelitis of L4 vertebral body. Patient was treated with transforaminal endoscopic drainage of abscess. Abscess was drained using a Ryle’s tube passed through the endoscope. Patients had relief from fever and radicular pain with improvement in back pain. Post operative magnetic resonance imaging scan showed drainage of abscess. Pus culture report showed growth of staphylococcus aureus. Patient was treated with antibiotic therapy according to culture report. Patient achieved complete neurological recovery three months after surgery. At two year follow up, patient was asymptomatic and MRI showed well decompressed cord and healed osteomyelitis L4 vertebral body. Transforaminal endoscopic drainage is safe and effective minimally invasive technique for anterior epidural abscess of thoracolumbar spine.
Key Words: Endoscopic drainage, Epidural abscess, Transforaminal endoscopy.
INTRODUCTION
Spinal epidural abscess (SEA) is the collection of pus and granulation tissue between the spinal dura mater and spinal column [ 1]. The reported incidence of spinal epidural abscess is 0.2-2.8 cases per 10,000 hospital admissions per year [ 2]. However, it has been recently increasing with a prevalence of 10-12 persons/10,000 patients due to increased elderly population, intravenous drug abuse, patient controlled analgesia, and spinal anaesthesia for pain treatment as well as decreased immune response caused by chronic diseases [ 3]. Clinical evolution of SEA encompasses 4 stages: pain, radiculopathy, weakness and paralysis [ 4]. The source of infection in SEA is, in most cases, haematogenous dissemination of bacteria from a localized focus elsewhere in the body, especially the skin. Staphylococcus aureus is the most common pathogen responsible for approximately 50% of cases [ 5]. Magnetic resonance imaging (MRI) is the method of first choice in the diagnosis. Despite the advances of modern diagnostic and management methods the associated morbidity and mortality in spinal epidural abscess remain high [ 6]. Laminectomy and decompression with antibiotic therapy is the standard treatment for spinal epidural abscess [ 6]. Lyu et al. described computed tomography (CT) guided drainage of massive epidural abscess [ 7]. Ito et al. first reported used of transforaminal endoscopy in 15 patients with pyogenic spondylodiscitis [ 8]. We describe transforaminal endoscopic drainage of massive anterior epidural abscess.
CASE REPORT
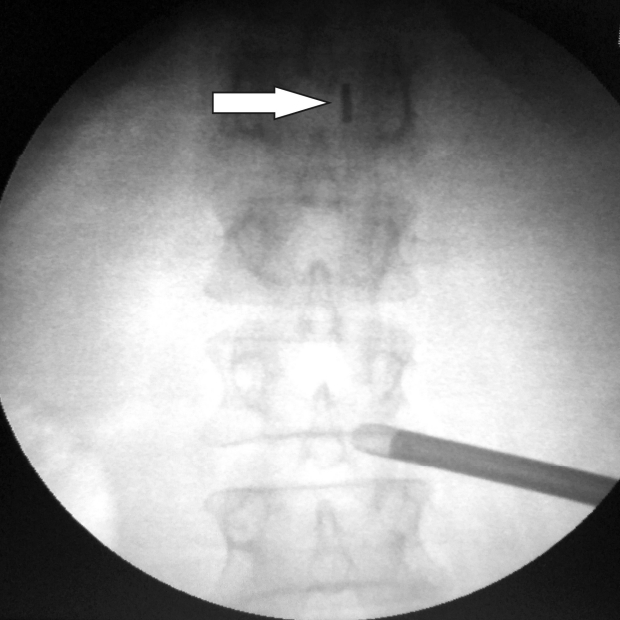
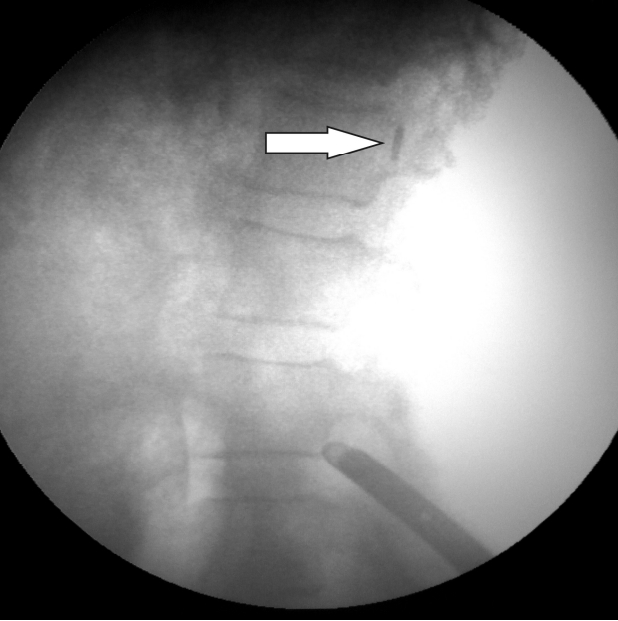
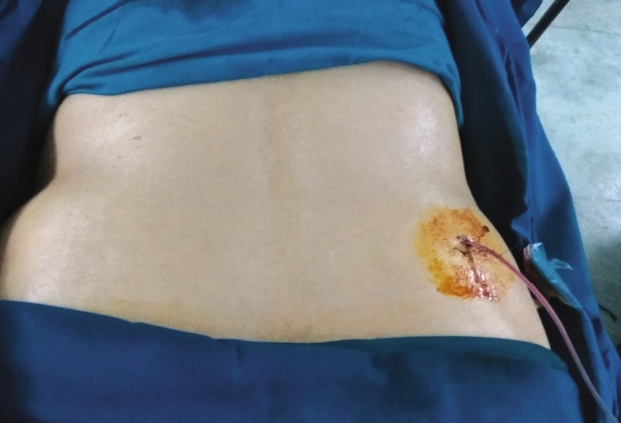
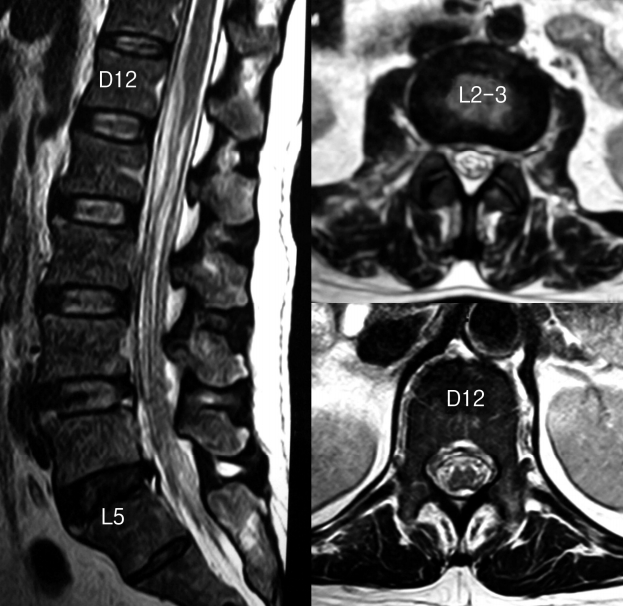
A 54 year old female non diabetic patient presented with fever of 15 days duration. Patient had severe back pain and bilateral radicular pain since 10 days. Patient developed weakness of both lower limbs, constipation and urinary retention since 5 days. The patient was a known case of depression on treatment. Patient was on broad spectrum antibiotics for fever and catheterised. Patient was febrile and had difficulty even to turn on the bed due to back pain. Physical examination revealed tenderness at the thoracolumbar area and grade III power in both lower limbs and reduced sensations below D12 level. Deep tendon reflexes were brisk in both lower limbs. Plantar reflex was extensor. Magnetic resonance imaging (MRI) scan dorlumbar spine with contrast revealed massive anterior epidural abscess extending from D10 to L4 with severe compression of thecal sac with osteomyelitis of body of L4 vertebra ( Fig. 1). Laboratory studies showed total count of 15,400 with neutrophilia, ESR of 120 mm/hour and CRP 110 mg%. Blood culture and urine cultures were negative. Patient was diagnosed to have massive anterior epidural abscess with cauda equina syndrome. Patient was taken up for immediate surgery in view of neurologic deficit. Surgery was done under local anaesthesia and sedation. Diclofenac sodium injection (75 milligrams) was given intramuscularly before starting the procedure. Intra operatively, intravenous fentanyl 50 micrograms and midazolam one milligrams were used for pain control. Transforaminal approach was made to L2-3 foramen on the right side. As there was no discitis, care was taken not to enter the disc space with any instrument. Dilator followed by cannula was placed at L2-3 foramen, directed cranially. Floating cannula was stabilised with hand and endoscope was inserted. Bleeding was controlled with radiofrequency ablation. Saline irrigation was used for improving the vision and to avoid dural injury. Epidural space was identified between the dura and posterior surface of L2 body. Endoscopic dissector was used to puncture the abscess. Pus started to leak out. Paediatric Ryle’s tube (No 8) was passed through the working channel of the endoscope and directed cranially into the abscess. Saline irrigation was temporarily stopped. Ryle’s tube was passed up to the D12 level under image control ( Figs. 2 & 3). Pus was seen coming out through the Ryle’s tube. Ten mL syringe was connected to feeding port of Ryle’s tube. Frank pus was aspirated and sent for analysis. Suction was connected to feeding port of Ryle’s tube to drain the pus. To and fro movements of the Ryle’s tube were done under continuous saline irrigation and suction to drain the abscess. Saline wash was given using irrigation fluid until clear fluid returned in the Ryle’s tube. Feeding port of the Ryle’s tube was cut off and left in situ as a drain in the epidural space. By this technique, we avoided another incision for drain. Endoscope and cannula were removed with care not to pull out the Ryle’s tube. Ryle’s tube was secured with 3-0 Ethilon suture ( Fig. 4). Cut end of Ryle’s tube was connected to suction drain. Dressing was done. Patient had relief from fever and leg pain with marked improvement in back pain. Pus culture and sensitivity report showed heavy growth of staphylococcus aureus sensitive to clindamycin, cefoperazone and sulbactam, cotrimoxazole, imipenem, meropenem, rifampicin, chloramphenicol. Post operative radiographs showed anterior placement of drain (Ryle's tube) up to D12 level. Drain was removed on second day with total collection of 10 mL. Post operative MRI scan done after drain removal showed drainage of the abscess and good decompression of the cord ( Fig. 5). Intravenous clindamycin 300 milligrams eighth hourly with cefoperazone sulbactam 1.5 grams 12 th hourly were given for two weeks. Follow up laboratory examinations showed decreasing trends in the patient’s white blood count, neutrophils, ESR and CRP levels. Bowel and bladder recovered at 10 days after surgery. Patient showed gradual motor recovery and was able to walk with support at the time of discharge. Patient was discharged at two weeks after the procedure with oral clindamycin 300 mg thrice daily for one month. Complete motor recovery was seen at three months after surgery. At two year follow up, patient was asymptomatic and MRI showed well decompressed cord and healed osteomyelitis L4 vertebral body.
DISCUSSION
Treatment options for spinal epidural abscess (SEA) traditionally consist of laminectomy to allow surgical drainage and decompression; computed tomography (CT) guided percutaneous aspiration, prolonged antibiotic therapy, or a combination of these approaches [ 9]. The nonsurgical versus surgical management of SEA remain controversial. Conservative treatment with antibiotics alone is justifiable only for specific indications [ 5, 6]. The vast majority of studies advocated early surgery to achieve better outcomes for treating SEA; this avoids high failure rates (41-42.5%) for non operative therapy, and limits morbidity/mortality rates [ 10]. In conservatively treated patients, delays in surgical decompression may lead to irreversible neurological deterioration, which is difficult to predict [ 11]. Tuchman et al. in their review article suggested that patients who are deemed good surgical candidates should receive their operation as soon as possible because the rate of clinical deterioration with SEA is notoriously unpredictable [ 12]. Spinal epidural abscesses most often occur at the lumbar level (50%), followed by the thoracic (38%) and cervical levels (12%) [ 9]. Dorsal abscesses extending across multiple spinal segments and exhibiting minimal cord compression with minimal or no neurological deficits can be considered appropriate candidates for CT guided or percutaneous techniques [ 7, 11]. Percutaneous needle aspiration is relatively contraindicated for anteriorly located abscesses [ 13]. Possible complications associated with percutaneous needle aspiration of epidural abscesses include dural tear, with subsequent development of meningitis [ 7]. Anterior abscess location, spondylodiscitis, osteomyelitis, and spinal instability are relative contraindications for a CT-guided, percutaneous, minimally invasive procedure [ 11]. The other disadvantages of CT guided drainage include need for experienced interventional radiologists, increased radiation exposure. Adogwa et al. in their study of 82 patients with spinal epidural abscess found that 70% were ventrally located and 30% dorsally located9. Hwang et al. reported a case of long level ventrally located thoracic spinal epidural abscess, where multilevel laminectomy failed to achieve motor recovery [ 14]. Hence ventrally located abscesses are difficult to drain using standard techniques. Percutaneous endoscopic lumbar discectomy is a safe and effective procedure in lumbar disc prolapse [ 15]. Transforaminal endoscopic surgery is increasing used in the last two decades for management of spinal infection as reported by multiple authors [ 8, 16]. It is easy to enter the anterior epidural space by transforaminal approach under direct vision. In our case, patient had osteomyelitis of L4 vertebral body with no spondylodiscitis. Hence it was very important to stay in the epidural space without entering the disc space. The abscess was centrally located in the anterior epidural space. The abscess was prominent up to L2-3 disc level and faded distally towards L4. Hence L2-3 space was selected for the approach. Additionally, L2-3 foramen is wide and allows easy epidural access without bone removal. The entry was directed cranially towards the abscess avoiding injury to exiting root. Once the abscess was opened; paediatric Ryle’s tube (No 8) was passed under image control to drain the entire abscess. Ryle’s tube has radio opaque marker at the tip which can be seen very well under image intensifier. The Ryle’s tube was connected to suction to evacuate the entire abscess. Irrigation fluid used during surgery helps in washout. Ryle’s tube was retained as a drain to achieve complete drainage of the abscess. Akbik and Shin reported transforaminal endoscopic drainage of ventrally located thoracic epidural abscess using vascular guidewire and paediatric feeding tube [ 17]. We have used paediatric Ryle's tube to drain the abscess. This technique is simpler and less expensive. Transforaminal drainage of thoracolumbar abscess is easier with lumbar approach when compared with thoracic approach. In the present case, intravenous antibiotics were given for two weeks and oral antibiotics for four weeks. This was to treat the osteomyelitis of L4 body. Soehle and Wallenfang noted significant association between spondylodiscitis or osteomyelitis and anterior abscess locations [ 18]. If it was a case of epidural abscess alone, a shorter duration of antibiotic therapy would have been adequate. The effectiveness of this technique is demonstrated by the complete abscess drainage on post-operative MRI and full neurologic recovery from cauda equina syndrome. MRI scan done at two years showed no evidence of infection. Because the procedure is performed under local anaesthesia and sedation, it can be performed even in high-risk patients. An acute abscess, defined as an abscess present for less than 16 days that consists of liquid purulent material, can be drained by endoscopic epidural catheter technique. Transforaminal endoscopic drainage of epidural abscess has the following advantages.
1. Done under local anaesthesia and sedation. 2. Minimally invasive with no resection of bone. 3. Does not require CT scan or interventional radiologist. 4. Easy access to anteriorly located abscess. 5. Familiarity of epidural access with endoscopy 6. Retraction of neural structures is not required. 7. Epidural catheter advanced under image guidance helps in drainage of abscess. 8. Irrigation with saline and use of suction helps in clearing the abscess. 9. Epidural catheter is retained as drain and helps in drainage post operatively. 10. Low risk of dural injury and other complications.
The limitations of this study are that it is a retrospective study and done on one patient at thoracolumbar spine. In case of cervical epidural abscess and dorsally located epidural abscess, interlaminar endoscopic technique can be used. If the abscess is chronic with granulation tissue, then it may not be possible to use this technique.
CONCLUSION
Transforaminal endoscopic drainage is a safe and effective minimally invasive technique in patients with anterior epidural abscess, especially in thoracolumbar spine. As the procedure is done under local anaesthesia, it can be performed even in patients with high risk for general anaesthesia. Abscess is drained under vision without retraction of neural tissues making it an effective alternative to the existing techniques. In cervical epidural abscess and dorsally located SEA, interlaminar endoscopic approach can be considered.
NOTES
Conflict of Interest
Author has no conflict of interest.
Fig. 1.
Preoperative MRI showing anterior epidural abscess D10-L4, osteomyelitis of L4 vertebral body. 
Fig. 2.
AP view of cannula and endoscope at L2-3 foramen with Ryle’s tube tip at D12 level. 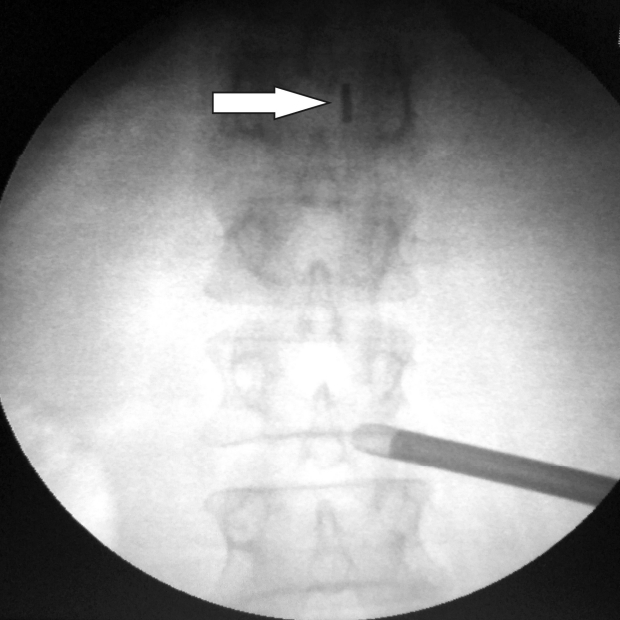
Fig. 3.
Lateral view of cannula and endoscope at L2-3 foramen with Ryle’s tube tip at D12 level. 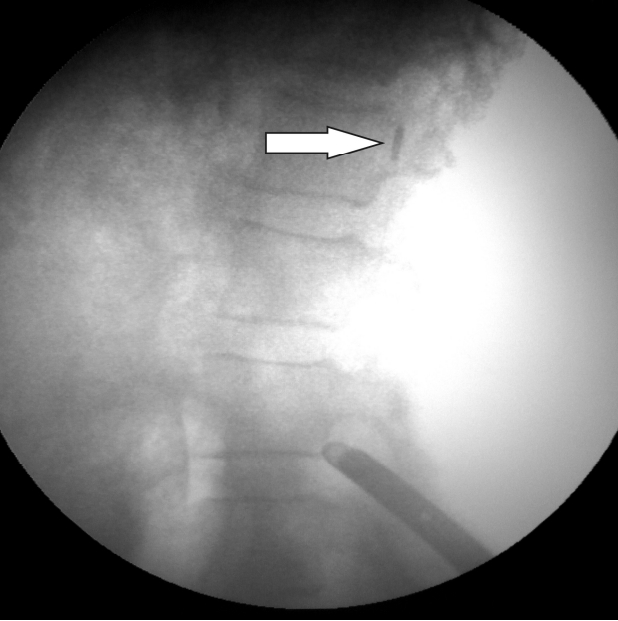
Fig. 4.
Ryle’s tube secured as drain. 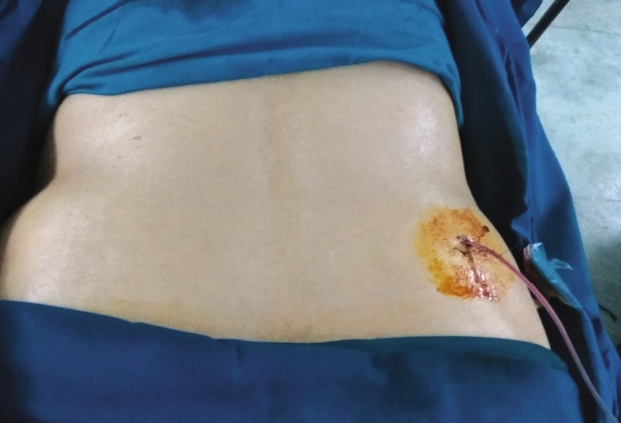
Fig. 5.
Postoperative MRI showing drainage of epidural abscess. 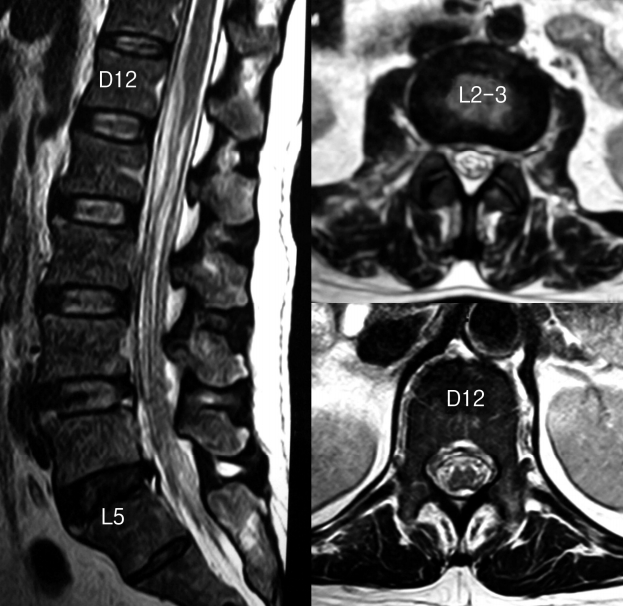
REFERENCES
1. Bluman EM, Palumbo MA, Lucas PR: Spinal epidural abscess in adults. J Am Acad Orthop Surg 12:155–163, 2004  2. Baker AS, Ojemann RG, Swartz MN, Richardson EP Jr: Spinal epidural abscess. N Engl J Med 293:463–468, 1975   3. Ma H, Kim I: Clinical outcomes of spinal epidural abscess. Korean Journal of Spine 9(1):6–11, 2012   4. Heusner AP: Non tuberculous spinal epidural infections. N Engl J Med 239:845–854, 1948   5. Tang HJ, Lin HJ, Liu YC, Li CM: Spinal epidural abscess-experience with 46 patients and evaluation of prognostic factors. J Infect 45(2):76–81, 2002   7. Lyu RK, Chen CJ, Tang LM, Chen ST: Spinal epidural abscess successfully treated with percutaneous, computed tomography guided needle aspiration and parenteral antibiotic therapy: Case report and review of the literature. Neurosurgery 51(2):509–512, 2002  8. Ito M, Abumi K, Kotani Y, Kadoya K, Minami A: Clinical outcome of posterolateral endoscopic surgery for pyogenic spondylodiscitis: results of 15 patients with serious comorbid conditions. Spine 32:200–206, 2007   9. Adogwa O, Karikari IO, Carr KR, Krucoff M, Ajay D, Fatemi P, et al: Spontaneous spinal epidural abscess in patients 50 years of age and older: A 15-year institutional perspective and review of the literature: Clinical article. J Neurosurg Spine 20:344–349, 2014   12. Tuchman A, Pham M, Hsieh PC: The indications and timing for operative management of spinal epidural abscess: Literature review and treatment algorithm. Neurosurg Focus 37:E8, 2014   13. Walter RS, King JC, Manley J, Rigamonti D: Spinal epidural abscess in infancy: Successful percutaneous drainage in a nine-month-old and review of the literature. J Pediatr Infect Dis 10:860–864, 1991  16. Yang SC, Fu TS, Chen HS, Kao YH, Yu SW, Tu YK: Minimally invasive endoscopic treatment for lumbar infectious spondylitis: A retrospective study in a tertiary referral center. BMC Musculoskelet Disord 15:105, 2014   17. Akbik OS, Shin PC: Endoscopic transforaminal drainage of a ventrally located thoracic epidural abscess. World Neurosurg 139:268–273, 2020  
|
|