INTRODUCTION
Coccygodynia is pain in the coccyx (tailbone area). Classic symptoms include midline pain located caudal to the sacrum and cephalad to the anus. This diagnosis is made clinically with pain in the coccyx region that is worse during activities such as sitting, standing, defecation, and sexual intercourse. Often, it is associated with lumbar pain, presumably from constant repositioning of the patient when sitting. Physical exam elicits tenderness to palpation of the coccyx. Clinical suspicion along with imaging techniques are used to make the diagnosis. Radiographs, especially sitting-versus-standing radiographs can be used to assess for dynamic instability. Common scans including Magnetic resonance imaging (MRI) and computerized tomography are often used to define the coccyx defect and to rule out other sources of sacrococcygeal pain [1]. Female sex, Body Mass Index (BMI) and trauma have been established as independent prognostic factors for coccygodynia treatment [2]. The higher incidence in women is perhaps due to differences in the shape and angles of the female pelvis and increased risk while giving birth [1]. Treatments include conservative therapies (physical therapy and capsaicin patch), interventional techniques (local injections with steroids and local anesthetic, pulsed radiofrequency ablation of ganglion, and extracorporeal shock wave therapy), and surgical techniques (complete and partial coccygectomies). There is a growing body of clinical evidence to support that coccygectomy is an effective treatment for patients with debilitating pain who had failed conservative therapies [3-5]. Failure is associated with certain pre-operative characteristics such as psychiatric illness, poor quality of life features, higher levels of pain, and use of opiates [6]. There is little research on the surgical approach to coccygectomy and its implications on post-operative outcomes. To our knowledge, this is the only study examining the paramedian approach to coccygectomy as compared to the midline approach.
MATERIALS AND METHOD
1. Patients
The investigation included a retrospective review of the electronic health care record of 36 patients from 2010-2019 with a history of coccygectomy for chronic coccygodynia performed by the most senior author. Patients were excluded if they underwent coccygectomy in addition to another procedure (2) such laminectomy or discectomy, did not trial conservative treatment, or if complete information could not be obtained from the medical record (1). The diagnosis of coccygodynia was confirmed based on a history of pain in the sacrococcygeal area exacerbated by sitting and recreated by palpation of the coccyx. Anteroposterior and lateral radiographs of the coccyx were obtained to aid clinical diagnosis. Patients were evaluated and deemed candidates for surgical treatment. Coccygectomy was preformed using a midline or novel paramedian approach described below. Recoded data included demographics, duration of symptoms, etiology, comorbidities, previous treatment, surgery time, complications, pre and post-operative 10-point visual analog scale (VAS) for pain, use of opiate drugs, and surgical approach. Data was transferred to a Microsoft Excel document and analyzed.
2. Statistical Analysis
It was preformed using a standard one-tailed T-test with alpha level set at 0.05 (5%).
3. Description of the Paramedian Approach
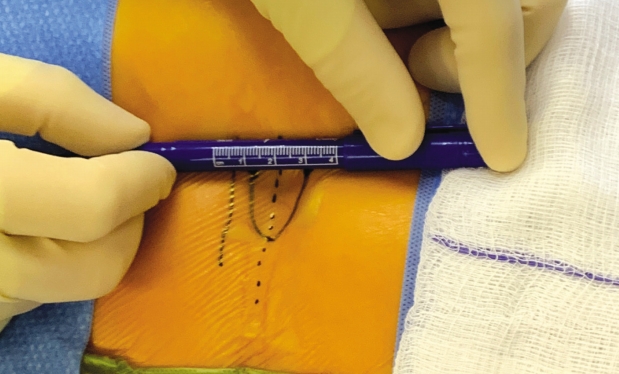
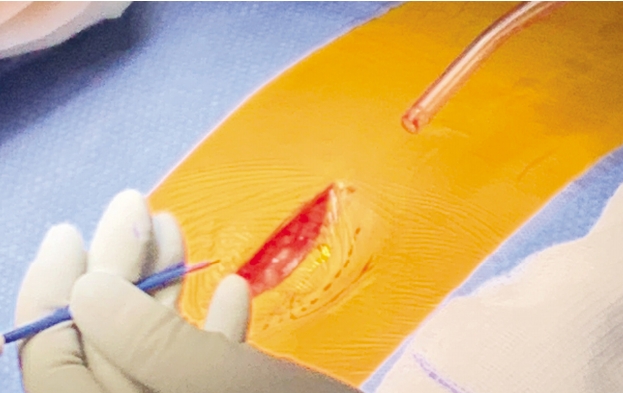
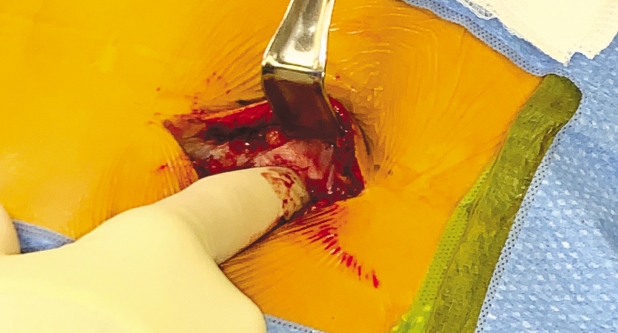
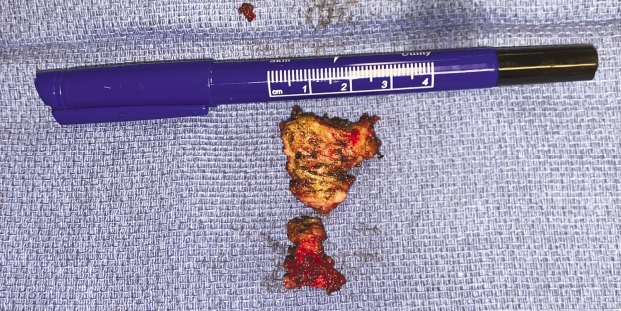
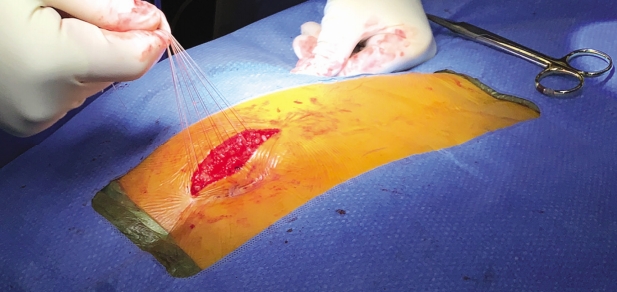
After operative consent is obtained, the patient is taken to the operating room to receive general anesthesia. The patient is then turned to the prone position on a WilsonTM frame mounted upon it. All pressure points are padded. The buttock and coccyx area are pre-prepped with isopropyl alcohol and allowed to dry. DuraPrepTM is then applied. The back and the coccyx are then sterilely draped utilizing IobanTM as a final barrier draping (Fig. 1). After the surgical timeout is conducted, a ~3 cm left paramedian incision is made adjacent to the intergluteal cleft approximately 2-3 cm cephalad to the anus (Figs. 2 & 3). A headlight is utilized for better visualization. The dissection is then taken tangentially to the midline of the coccyx in the sub-periosteal plane so as to obtain direct access dorsally (Figs. 4 & 5). The coccyx is palpated along the way. Assurances are made to prevent interference with the rectum or the anal area. The edges of the coccyx are then trimmed off utilizing a 4 Kerrison, curved curets and coagulation electrocautery at a setting of 20 watts. The coccyx is removed (Fig. 6). The wound is then irrigated and anesthetized with 0.5 Marcaine in the absence of epinephrine, and without penetrating anterior to the surgical field at all. #0 Vicryl is then utilized to close soft tissue to itself and to the residual elements of the sacrum using transosseous suture fixation (Fig. 7). The subcutaneous tissue is closed with 2-0 nylon using interrupted horizontal mattress sutures (Fig. 8). Sterile dressings are applied, and the patient is allowed to shower the wound without dressings on post-operative day number 2, after which, dressings are re-applied.
4. Description of Midline Approach
The midline approach, an earlier approach used by the senior author, is the same as the paramedian approach except that the initial incision is taken in the midline through the skin and subcutaneous tissue through the periosteum and then into the periosteal plane around the coccyx. The closure sequence is the same, but the amount of tissue closure is less because it is more direct.
RESULTS
Between 2010 and 2019, 36 patients with coccydynia (ICD-10 Code M53.3) with record of coccygectomy were identified. Three patients were excluded from the study due to additional spinal surgery (2) or missing data (1). Included in the study were 24 females and 9 males with a mean age of 46 years (range 18-74 years). The most common etiology was trauma (26) and idiopathic (7). 27 patients underwent coccygectomy with a paramedian approach and six had the same procedure with the midline approach. Demographics are displayed in Table 1. The average BMI was 27.8 (range 21.4-38.2). Injections, offloading, physical therapy, and non-steroidal anti-inflammatory medications were common conservative treatments reported in our patients. The average duration of symptoms was 8.2 years (range 2 months to 35 years). 25 of the patients required post-operative opioid pain medication, most commonly oxycodone 5-10 mg. For the paramedian group, 3 of 27 patients required antibiotics due to post-op infection. For the midline group 4 of 6 had wound complications requiring either incision and drainage and/or antibiotics. There was a significantly lower infection rate in the paramedian group (p=0.00871, alpha <0.05). No operative complications were noted in the paramedian group. In the midline group one patient required a wound-vacuum placed at the end of the operation. Data for wound complications is displayed in Table 2.
For the paramedian group 17 Patients reported a decrease in pain per VAS, 5 reported no change, 5 reported an increase in pain, and one reported complete resolution with a VAS score of 0 post-operatively. VAS data for the paramedian approach averaged 7.1 pre-operatively and 4.4 post operatively. These values were obtained at pre and post-op visits. On average, VAS scale was administered 7 days before surgery range (1-18 days) and 175 days after surgery range(17-529 days). The average surgery time in this group was 40.6 minutes. The maximun surgery time was 53 minutes and the minimum surgery time was 29 minutes. Surgery time was not recorded for 4 patients and those were excluded from the operating time analysis.
DISCUSSION
Coccygectomy for chronic coccydynia has been established as a promising treatment for pain refractory to conservative management [3-6]. The most common complications after coccygectomy are infection and postoperative wound dehiscence. In a review of the literature Kleimeyer and colleagues report postoperative dehiscence and infection rates ranging from 0% to 30% [3]. Infection is most commonly with S. aureus [7], however recent authors have reported using preoperative rectal enemas and broadening antibiotics to cover gram negative microbes [8]. In our patients we use cefazolin intravenously with 1 gram applied directly into the wound at the end of the case. Notably, we saw significantly less infections and/or postoperative dehiscence with the paramedian approach (p=0.000871).
We believe that the lower infection rate is due to the paramedian surgical approach in addition to antibiotic coverage and surgical technique that allows a deeper skin flap away from the less exposed intergluteal cleft. In the classic midline approach described by Key et al. [9] a two and one-half inch long midline vertical incision is made over the sacrococcygeal articulation and carried down to the bone. This approach described in 1937 is still the most commonly used approach today [10-13]. We presume that the wound location within the intergluteal cleft acts as a nidus for infection. Our approach avoids this natural crevice and instead allows wound closure adjacent to intergluteal cleft. We also speculate that the location of the incision site may avoid direct pressure while sitting. Another small study of 25 patients by Bilgic et al. [14] suggests that periosteal preservation and closure are related to low risk of infection. They report an infection rate of 0% (0/14) with periosteal preservation vs 36% (4/11) without. However, the superficial surgical approach was not examined.
The paramedian approach does not appear to negatively impact surgery time. Our average surgery time was 40.6 minutes;10 minutes lower than reported in a recent study with total excision of the coccyx [15].
Although our study involves a small sample size, the demographics are similar to recent studies [11]. Trauma remains the most common etiology, and middle age females also make up the majority of our patients. Limitations of this study include small sample size and lack of data relating to outcomes. Only one pain scale (VAS) was used to evaluate post-operative pain, while other studies employ multiple. The Coccygodynia Disability Index (CDI) which is a four-question instrument using questions 1, 5, 8, and 9 from the Oswestry Disability Index [16], should be included for further studies of this approach. Another limitation was the small comparison group for the midline coccygectomy. There was a lack of available data in the midline group in regard to VAS reporting and surgery time.
CONCLUSION
The paramedian and midline approach to coccygectomy are both viable treatments for coccygodynia. While the traditional midline approach has low complication rates and high patient satisfaction, it is possible the paramedian approach offers these same positive outcomes. Surgeon and patient preference should be taken into account when choosing a surgical approach for coccygectomy. Further examination of the paramedian approach and its role in reducing infection is needed. Additional prospective studies comparing traditional midline vs. paramedian approach are needed to assess whether there is superiority of one method versus another.