INTRODUCTION
Cauda equina syndrome (CES) has a significant place in the field of spine surgery because of its devastating consequences such as bowel, bladder, sexual and lower limb dysfunction [1]. Prompt diagnosis and investigation followed by timely and skillful surgery and rehabilitation are the ways to have best outcomes in the treatment of this rare but often very damaging condition.
Most common causes are lower lumbar disc herniation, prolapse, and sequestrations [1]. Traditional open and microscopic procedures for cauda equina are associated with undue traction on the thecal sac and nerve roots while approaching the disc. The placement of rongeur with large foot plate under lamina during laminectomy may further compromise the canal with undue pressure on neural structures [2].
We report a case of CES due to massive disc prolapse at L4-L5 level which was operated by percutaneous endoscopic transforaminal lumbar discectomy (PETLD) under local anesthesia. This report mainly highlights the effectiveness of PETLD in approaching the herniated disc without handling the neural structures and with prompt recovery.
CASE REPORT
A 37 years old women presented with back pain which was radiating to bilateral buttocks and legs (left>right) with inability to lift her left ankle and associated with numbness over left leg and ankle since 4 days. She also complained of difficulty in passing urine but no incontinence. The patient did not pass a motion on the day of the visit. There was no significant medical or surgical history.
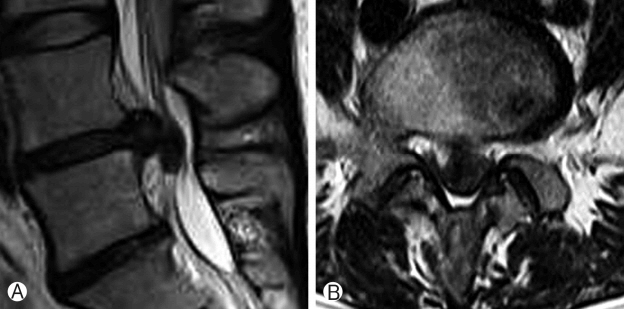
On examination, she was found to have left side Straight leg raising test was positive at 30 degrees and 1/5 power in her left ankle dorsiflexors and plantar flexors. In addition, decreased sensation (3/10) was noted in her left L5 and S1 distribution with saddle anesthesia. There was no weakness on right side. MRI (Fig. 1) showed massive disc herniation at L4-L5 level causing significant compression of cauda equina.
The operation was done in the prone position on a radiolucent table. It was performed under conscious local anesthesia induced by an initial injection of 8-10 mL of 1% lidocaine during needle insertion in the foraminal space and a second booster injection of 2-4 mL of 1.6% lidocaine (8 mL 2% lidocaine plus 2 mL saline plus 0.05 mL epinephrine) 4-5 minutes after the initial injection. To avoid injuries to exiting and traversing nerve roots during the approach, the operation was proceeded with continuous feedback from the patient. Fluoroscopic guidance was used to identify the intervertebral disk space.
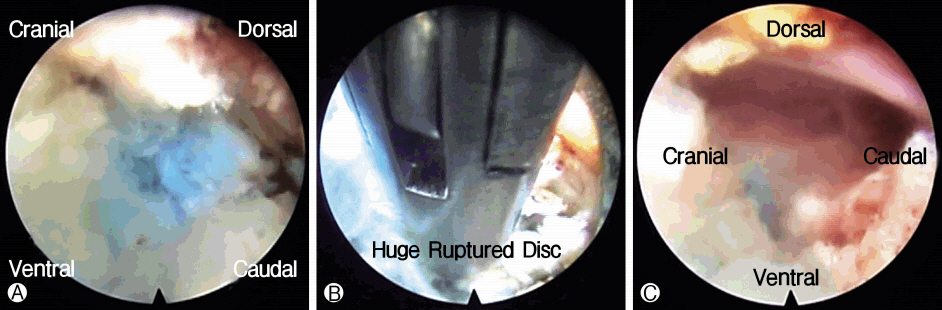
The skin entry point was marked at the midline of the disk space. An 18-gauge spinal needle was inserted at the point using the manual back muscle assessment method [3], approximately 12-14 cm away from the vertebral midline and at 25-35 degree angle. After passing through the fascia and back muscle, the needle was docked at Kambin’s triangle, near the intervertebral disk. After checking the free epidural space with contrast dye injection (Iobrix injection; Taejoon Pharm, Seoul, Korea), a needle was inserted in the discal space, and discography was performed using 0.8% indigo carmine (Carmine, Korea United Pharmaceutical, Yoenki, Korea) mixed with contrast. A guide wire was inserted through the needle, and the needle was removed. Through the inserted guide wire, an obturator was inserted in Kambin’s triangle, and the wire was removed. A working cannula was inserted through the obturator which was then removed and an endoscope (Joimax GmbH, Germany) was inserted through the working cannula. After insertion of the endoscope in the working cannula, the epidural fat and soft tissue were dissected with a radiofrequency probe (Elliquence, New York, USA). We used an endoscope with a 30-degree view angle in all the routes. The out-and-in trans-foraminal approach was followed. After decompression of the intradiscal ruptured disc, the next step was to remove main herniated disc (Fig. 2A).
High canal compromised LDH were approached by the intervertebral route [3]. Next, we made a half-and-half view of the epidural space and discal space with the insertion of a bevel-type working cannula in the fenestrated annulus. The next step was targeted fragmentectomy (Fig. 2B).
The endoscope was turned to check for any remnants. The decision for adequate decompression was accomplished by visual inspection of the mobility of free floating dural sac, exiting root, traversing root, and epidural space (Fig. 2C). The entire procedure was performed using constant saline irrigation.
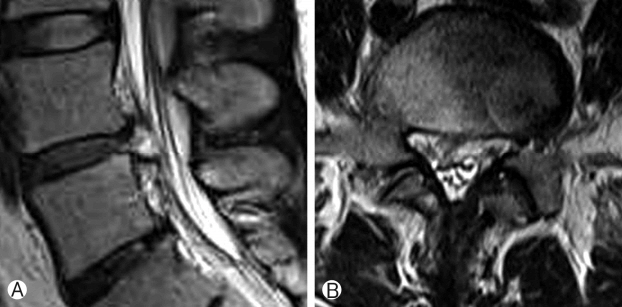
The postoperative period was uneventful and MRI (Fig. 3) showed a complete decompression of cauda equina. The patient was discharged on the second postoperative day with moderate paresis of ankle dorsiflexors and plantar flexors (3/5). After 2 months with a rehabilitation program, her muscle strength of left ankle dorsiflexors and plantar flexors improved to 4/5 (Video 1) with full recovery from saddle anesthesia. Left L5 and S1 hypoesthesia (3/10) persisted for many days.
DISCUSSION
Most surgeons have advised emergent surgical decompression for CES [4]. Open decompression (e.g., wide laminectomy, hemilaminectomy, and fenestration) and microendoscopic discectomy (MED) has been recently advocated to obtain optimal decompression for CES. Recent advances in newly developed instruments and endoscopes have minimized damage to normal tissues and made the approach minimally invasive for lumbar disc herniation (LDH) which is feasible under local anesthesia.
To date, PETLD is recognized as the most minimally invasive approach for the treatment of disc herniation. The most beneficial aspect of this technique is local anesthesia with the awake patient so that we can avoid iatrogenic nerve root injury and risk of general anesthesia. Additional benefits of PETLD are shorter hospital stays, faster return to daily activities, less blood loss and low infection rate [5].
Traditional open surgical treatment causes more soft tissue violation and bone resection [6] which may lead to postoperative instability. This instability requires fusion surgery, which is associated with more morbidity and prolonged rehabilitation needs. Open surgery for excision of disc herniation is associated with retraction of nerve roots which increases the possibility of neuro deficit in already compromised neural tissue in cauda equina syndrome which can be easily avoided with PETLD [7].
Kim et al. reported a rare case of CES caused by LDH during the third trimester of pregnancy, which was treated successfully by PETLD [8]. Namboothiri et al have reported two cases of percutaneous transforaminal access using inside-out technique done under local anesthesia for acute CES [7]. Subash et al. presented a case of LDH causing acute CES that was resected by PETLD through a transforaminal approach [9]. However, most surgeons did not recommend PETLD for CES, as it considered potentially high-risk with complications.
PETLD technique is technically more demanding than open surgery so, in order to decrease the surgical risk, it should be used to treat CES only after the surgeon has extensive training and surgical experience in spinal endoscopy.
Surgery is performed with the endoscopic transforaminal approach using the “outside-in” technique, in which the working cannula placed into the lower part of the neuroforamen, thus, retracting and avoiding the exiting nerve root. The cannula tip or the endoscope is not inserted into the disc space. This reduces the chances of increase in intradiscal pressure and further compression of cord.
In outside in technique annulotomy is essentially made in the foraminal area which is away from the compressed thecal sac and nerve roots and hence has no chance of worsening of neurological deficit. In addition to mentioned features incision of 0.8 cm gives better aesthetic outcome. As these surgeries are required to be performed in an emergency, the medical comorbidities can be very well managed under local anesthesia.
Since this is only case report, the superiority of the technique could not be proved but we want to report on a minimally invasive technique for cauda equina syndrome with massive disc prolapse.