INTRODUCTION
Lumbar disc herniation (LDH) is a common cause of back pain and sciatica, and it imposes a significant financial burden on the medical system. Surgical management is typically considered when conservative treatments fail. However, conventional open discectomy may not be suitable for patients with massive upmigrated herniations in the hidden zone of MacNab. The anatomical characteristics of the bony canal in this area contribute to severe compression of the nerve root, resulting in intense pain and complete disability, necessitating a more aggressive treatment approach. LDH in the hidden zone is often accompanied by acute onset neurological weakness in the exiting root.
Surgical treatments for LDH include conventional open surgery, microscopic-assisted surgery, and endoscope-assisted surgery. Although conventional open surgery and minimally invasive approaches such as microendoscopic discectomy (MED) and postendoscopic techniques have shown good results, they can potentially damage the bony spinal structures and paraspinal muscles, including the multifidus and rotators groups [1].
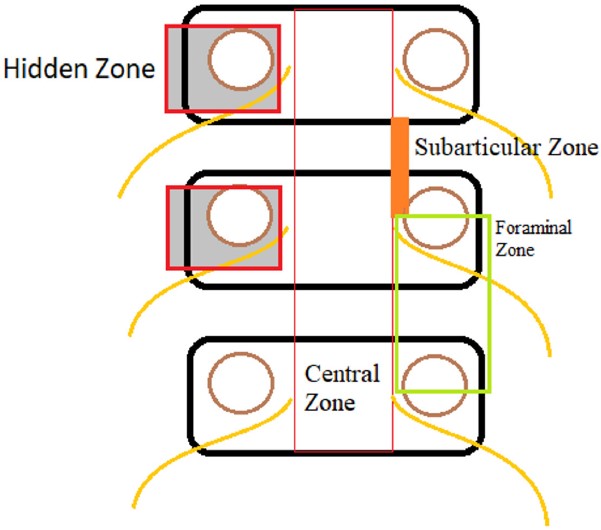
The extrusion of nuclear material in a cranial or caudal direction with disc material displacement occurs at the annulus-apoptosis interface in an acute manner. It has been classified into 4 zones by Lee (Table 1) [2,3].
The herniation of the nucleus pulposus depends on the separation of the annulus at the apoptotic interface of Sharpey's fibers, determining whether the herniation occurs cranially or caudally. The L4–5 level has the highest incidence of compressive radiculopathy, followed by the L5–S1 level [4].
The lateral part of the lumbar spinal canal is subdivided into the lateral recess (subarticular), pedicle (foraminal), and far lateral (extraforaminal) zones. Within these regions lies the "hidden zone of MacNab," which is known for its challenging surgical exposure [5]. The hidden zone of MacNab is bordered by the dorsal part of the vertebral body anteriorly, the pedicle laterally, and the pars interarticularis of the hemilamina of the cranial vertebrae posteriorly (Figure 1). This region can be compromised both due to bony stenosis of foramen as well as disc herniations.
In approximately 10% of patients with LDHs, a fragment migrates cranially into the hidden zone of MacNab, affecting both the traversing and exiting nerve roots. The management of LDH located in the pre- and intraforaminal regions of the hidden zone of MacNab remains a subject of debate. Many approaches require significant removal of the lamina and other important bony anatomical structures, which may result in biomechanical instability and accelerated degeneration [6].
The interlaminar route in open surgical methods involves partial removal of the ipsilateral hemilamina (extended laminotomy or hemilaminectomy) and may also require partial removal of the facet joint (medial facetectomy) [7]. Manipulation of a fragment underneath and proximal to the axilla during the procedure may inadvertently lead to lateral displacement and potential fractures or weakening of the pars interarticularis superiorly, fracture of inferior articular process (IAP). Especially at higher levels as the lumbar disc is higher in relation to lower edge of cranial lamina [6].
Various surgical approaches that involve the removal of important biomechanical structures increase the risk of secondary segmental instability, necessitating additional surgical procedures [6].
Among the less invasive modalities endoscopic translaminar approach through a fenestration of the pars interarticularis was proposed by Di Lorenzo et al. [8] and a crossover translaminar approach was proposed by Reinshagen et al. [6,9] which uses a fenestration of the contralateral hemilamina at the base of the spinous process. Beside the increased operative time, and increased incidence of complications and revisions, these techniques have limited access to intervertebral disc space at lower lumbar levels [2,10,11].
Though transforaminal endoscopic procedures are helpful, they are not recommended for the more medial foraminal lesions of the hidden zone due to imposed spatial restrictions, especially in the lower lumbar levels [6].
In contrast, the transforaminal endoscopic method involves partial anchoring of the transforaminal cannula and its directional turning towards the axilla, facilitating the identification of the elevated exiting nerve root due to the fragment in the hidden zone of MacNab.
The key to extracting a highly migrated fragment from the hidden zone of MacNab in a relatively bloodless manner lies in identifying the space between the exiting nerve root and the posterior surface of the bony Kambin triangle.
This study evaluated the effectiveness of transforaminal endoscopic discectomy for superiorly migrated LDH in the hidden zone of MacNab. The surgical method was assessed using the visual analogue scale (VAS) score, Oswestry Disability Index (ODI) score, and modified MacNab criteria.
This study aims to investigate the efficacy, advantages, and safety of TPED for superiorly migrated LDH in the hidden zone of MacNab, focusing on patients with isolated causative factors such as prolapsed discs.
We hypothesized a novel way by which marginal cutting of annular fibers gave direct access to the posterior vertebral surface underneath the axilla thereby securing a safe and easily reproducible technique. Using flexible grasper and hooks allows sweeping of the posterior vertebral surface reaching parallel to proximal pedicle and higher if need be to extract an up migrated fragment.
MATERIALS AND METHODS
The study duration spanned 2 years, from January 2020 to January 2022. The patients were selected on the basis of the following.
1. Inclusion Criteria
• Patients experiencing low back pain and radicular symptoms in unilateral lower extremity with radiologically confirmed superiorly migrated disc or sequestrated disc.
• Presence of polyradiculopathy involving both the exiting and traversing nerve roots, muscle weakness, absent ankle reflex, and sensory changes.
• Acute onset neurological symptoms of weakness and severe pain affecting daily activities, with radiological confirmation of LDH in the hidden zone.
• Imaging findings consistent with single-level disc herniation in the hidden zone of MacNab.
• No previous surgical history at the same level.
2. Exclusion Criteria
• Radiographic findings that did not align with the patient's symptoms or signs.
• Presence of symptomatic LDH at other levels or facet arthropathy.
• Patients with known neurovascular disorders or any other pathological conditions that could mimic the clinical condition (e.g., neurofibroma, Tarlov's cyst, facet cyst).
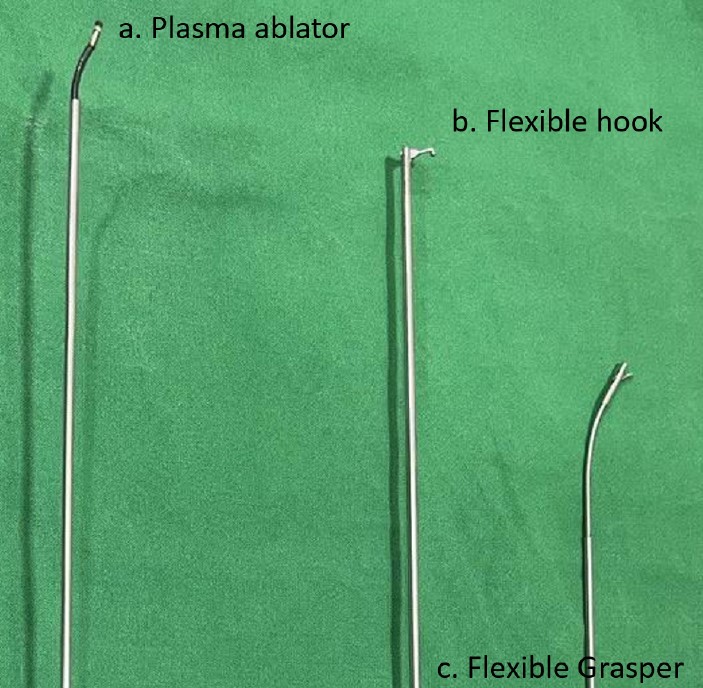
3. Instruments Used
The following instruments (Figure 2) were utilized during the transforaminal endoscopic discectomy procedure for superiorly migrated LDH in the hidden zone of MacNab:
1. The standard transforaminal 6.6-mm endoscope with 3.2 mm working channel was used.
2. Flexible grasper: The 2-mm diameter flexible grasper was used to grasp and manipulate tissues within the surgical field. It allows the surgeon to carefully handle and extract the sequestrated disc fragment during the procedure.
3. Hook: flexible hooks measuring 2 mm in diameter and 5/10 mm in length is utilized. This instrument aids in creating a pathway and facilitating the removal of the disc fragment with precision.
4. Plasma frequency ablator: The plasma frequency ablator, with a length of 230 mm, is employed for tissue ablation and coagulation. It assists in creating a safer pathway and reducing the risk of bleeding during the procedure.
4. Surgical Procedure (Supplementary Video Clip 1)
The surgical procedure was preferably performed under deep sensory epidural anesthesia, supplemented with local anesthesia. It is crucial to extract the fragment from the anterior epidural space, superior to the axilla. Performing the procedure from below the axilla using only local anesthesia is not satisfactory due to the proximity and tension on the elevated exiting root caused by the LDH.
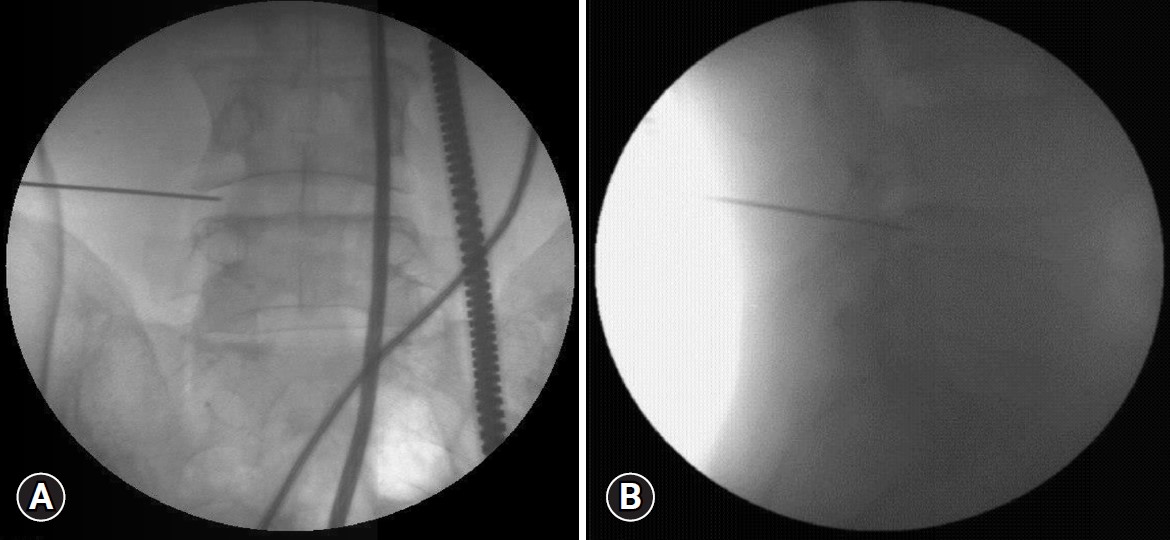
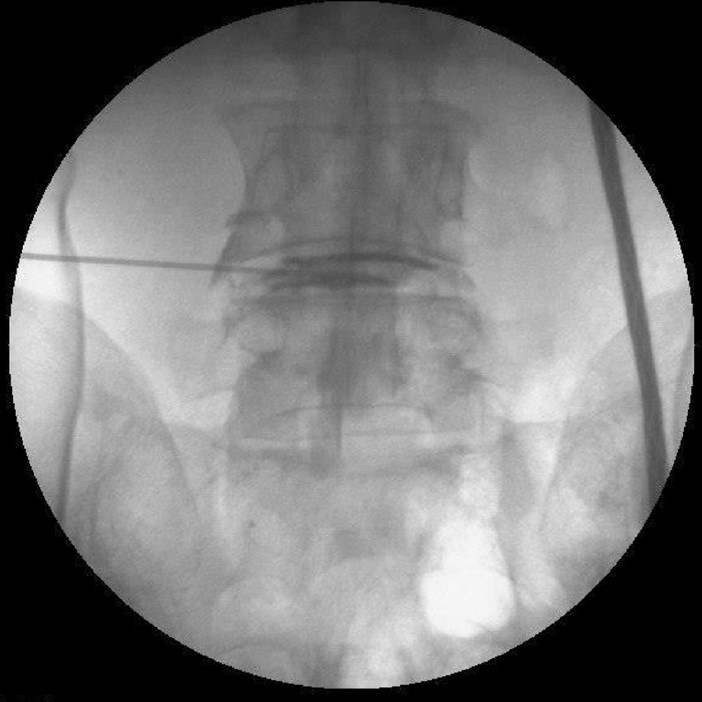
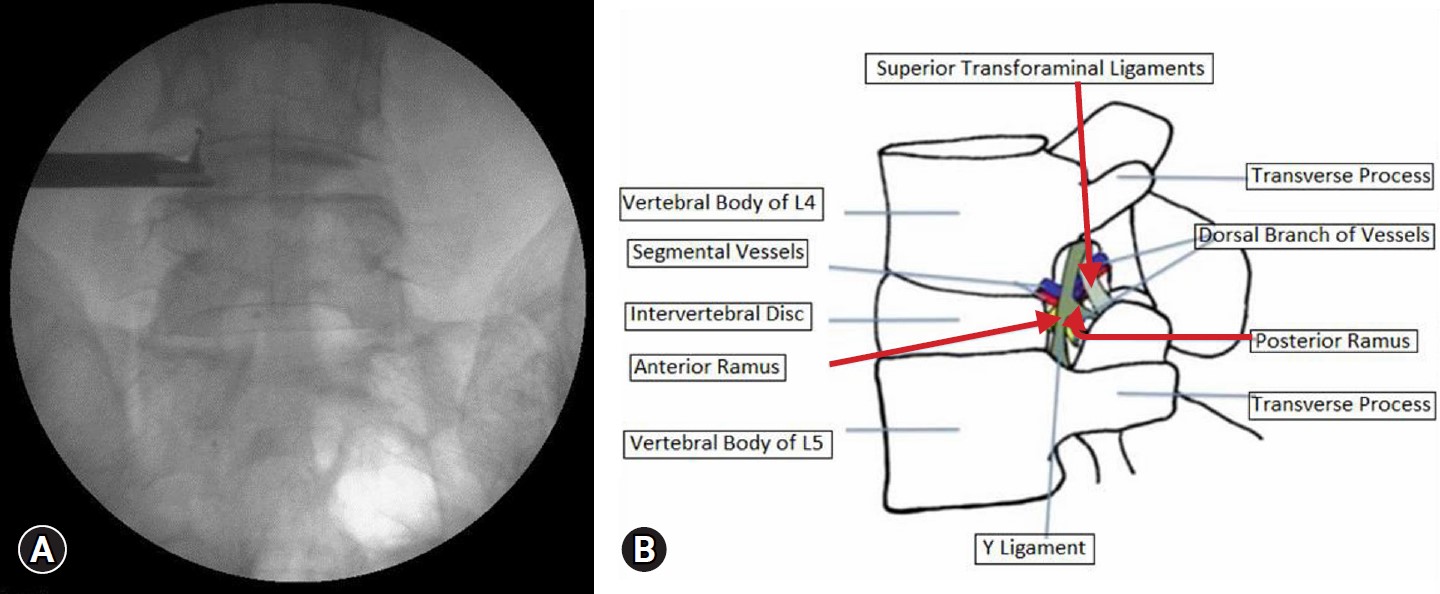
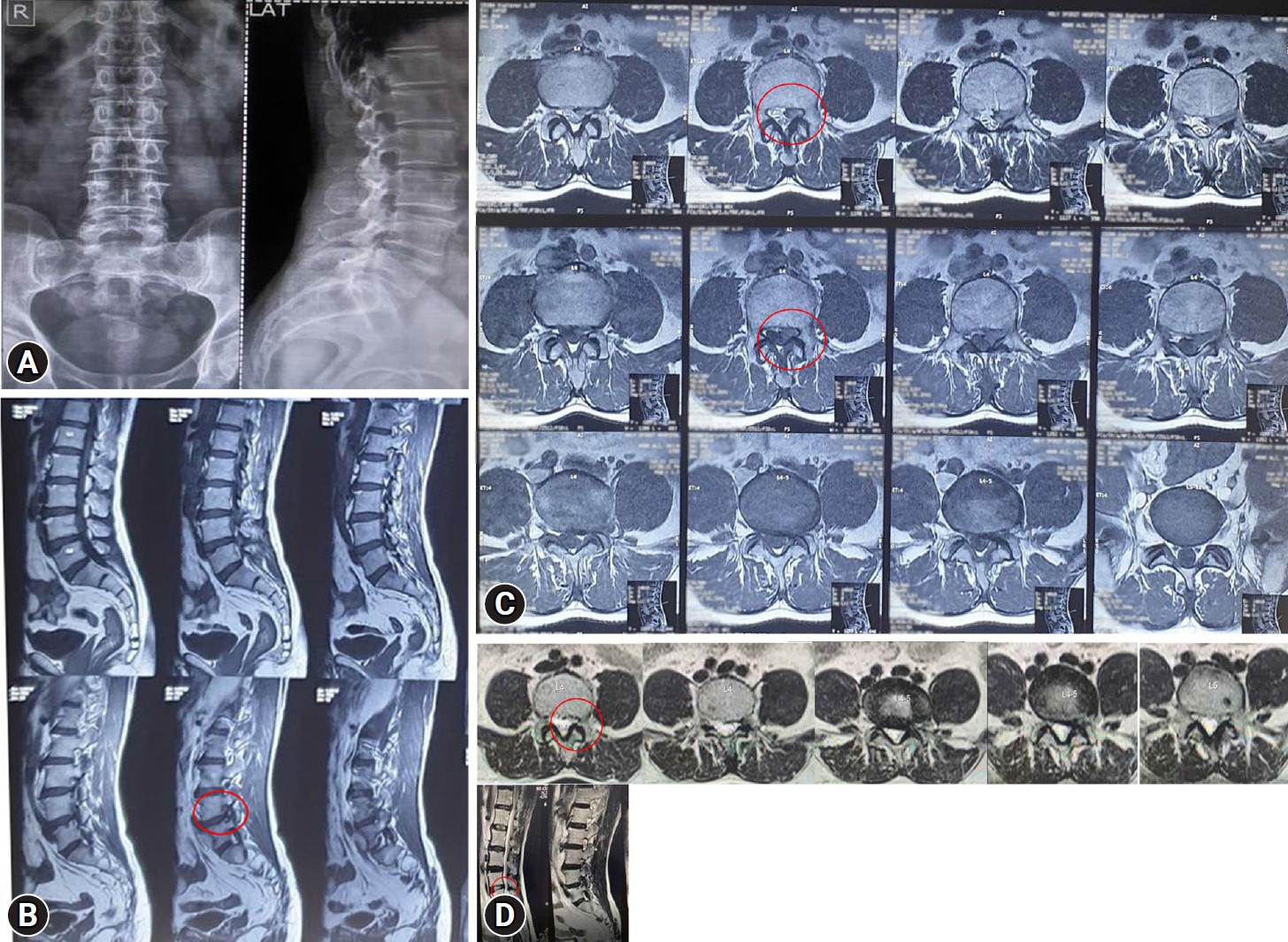
Under C-Arm guidance in anteroposterior and lateral views, the foraminal space was identified (Figure 3). To facilitate identification of the annulus and extruded fragment, dye (indigo carmine) was injected into an intervertebral disc. The staining helps identify the rent, and the additional use of Omnipaque 300 contrast material aids in pinpointing the rent (Figure 4).
The transforaminal scope was introduced into the foraminal space in a cranial direction, followed by partial anchoring of the sheath on the annulus fibrosus. The open end of the sheath was turned towards the axilla to facilitate the identification of the exiting nerve root. The endoscopic hook was then introduced, and the superior articular process (SAP) tip was identified. The foraminal attachment of the flavum and foraminal ligaments was separated from the tip of the SAP, ensuring the release of the tethered exiting root and axilla. This maneuver reduces stress on the exiting nerve root and minimizes the risk of inadvertent damage to the root and dysesthesia (Figure 5).
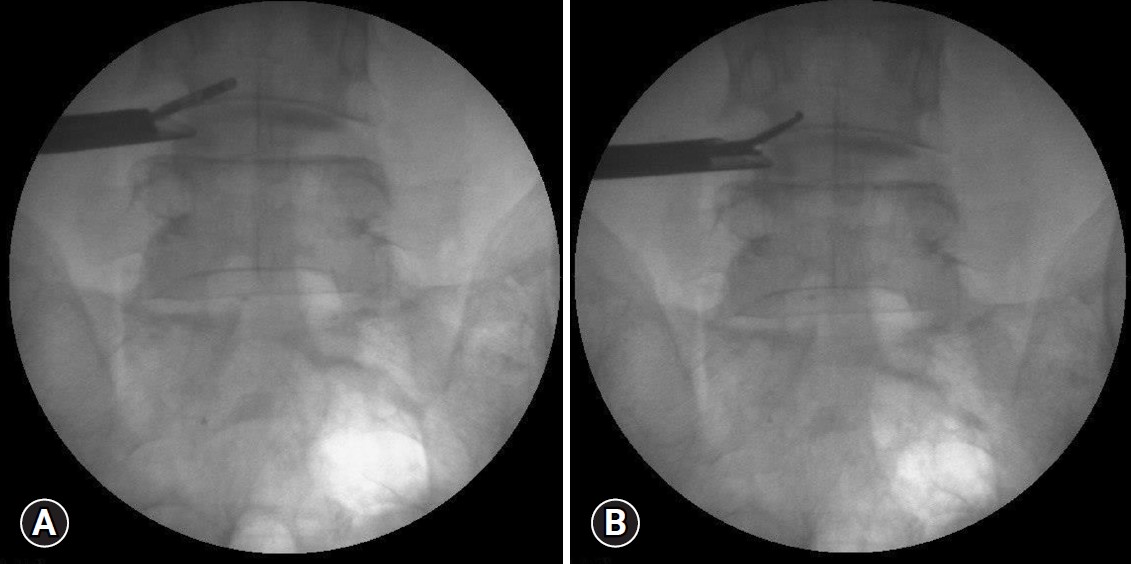
In the case of a left-sided disc, the cut surface of the endoscopic cannula was rotated to the 8 o'clock position. For a right-sided disc, it was rotated to the 4 o'clock position. This rotation helped bring the exiting nerve root to the upper and outer corner of the endoscopic view (Figure 6).
The interface between the discal surface and the root was exposed to close off the axilla. This step prevented accidental migration of the plasma radiofrequency (RF) ablator towards the axilla and unintended damage to the root. The RF ablator, when fired at low-temperature settings (below 40°C), does not cause any permanent nerve root damage. In case it comes into contact with the nerve root, the patient's leg may twitch, but there is no permanent root injury.
Using a flexi-tip plasma probe, a space was created below the exiting nerve root and the dorsum of the vertebral body in the upper part of the bony Kambin triangle. The location was confirmed under fluoroscopy. Probing upwards from this space with the use of a hook and flexible grasper allowed access to the hidden zone, located anterior to the neural tube and beside the superior pedicle. Confirmation of the position was again performed using fluoroscopy.
During this manoeuvre, elevating the head end of the table reduces epidural pressure, which prevents post procedure headache. Additional use of transient fentanyl (up to 100 μg) may be necessary, despite providing the patient with sensory epidural anesthesia.
All patients completed VAS, ODI for preoperative and postoperative evaluations at 2 weeks, as well as at 1, 6, and 12 months following the procedure to assess pain and improvement in their clinical condition. Modified MacNab criteria questionnaires were done at the end of 12 months.
5. Ethics Approval
This is an observational study. The authors confirm that written informed consent was obtained from all participants or their legal guardians, and they were adequately informed about the nature of the study, its objectives, potential risks, benefits, and alternative treatment options. The confidentiality and anonymity of the participants were maintained throughout the study, and all applicable ethical guidelines and regulations were adhered to. The authors have confirmed that no ethical approval is required.
RESULTS
Twelve patients, with a mean age of 48.8 years, were included in the study with a minimum follow-up of 12 months. There were 7 males and 5 females. The distribution of the LDH is shown in Table 2. The mean duration of surgery was 97.5 minutes (range, 60–130 minutes).
The average VAS scores for both back pain and radicular pain significantly decreased from 8.9 and 7.6, respectively, before the surgery to 2.9 and 1.0 at 1 month postoperative. At 12 months, no pain was reported (p<0.05). These findings are summarized in Table 3 and Figure 7.
The average ODI scores significantly decreased from 91.33±6.34 to 8.16±2.75 at the 12-month postoperative assessment (p<0.05). This indicates a significant improvement in functional disability following the surgery. The results are summarized in Table 4.
Based on the modified MacNab criteria, 11 out of 12 patients were rated as having an excellent outcome, while 1 patient was rated as having a good outcome. These results highlight the favorable postoperative functional outcomes achieved with the surgical intervention.
DISCUSSION
Transforaminal percutaneous endoscopic discectomy (TPED) is a widely employed treatment for symptomatic LDH. Various techniques, such as the use of a microscope, tubular systems, destandu technique, interlaminar endoscopy, and unilateral biportal endoscopy (UBE) have been developed for decompression during TPED surgery. These techniques often involve excessive removal of the lamina and IAP to access and remove sequestrated upmigrated disc fragments above the axilla, or requiring contralateral approaches that result in significant bone removal and even sacrifice of the spinous process base. Unfortunately, these approaches pose risks, including accelerated facetal arthritis, pars interarticularis fractures, and subsequent instability. To address this challenge, we proposed a novel approach that avoids excessive bone work, preserves the facets and does not disturb the multifidus muscle mass. This approach offers alternative method for managing this complex problem.
Compared to open surgery, TPED for LDH provides several advantages, including minimal invasiveness, reduced impact on spinal stability, rapid recovery, minimal blood loss (less than 50 mL), and immediate mobilization facilitated by sensory epidural anesthesia.
The traditional approach of hemilaminectomy for LDH in hidden zone of MacNab presents a higher risk of pars interarticularis fractures due to requirement of extensive laminectomy which can lead to subsequent degeneration and complications. Furthermore, when performing partial laminectomy for the removal of superiorly migrated disc fragments, surgeons often resort to lateral surgical exposure rather than an upward approach to avoid cord and exiting nerve root injuries or dural tears. However, this lateral exposure increases the risk of pars fractures and damage to the inferior articular process. Additionally, the presence of the Batson venous plexus in the axillary areas and superior and inferior communicating veins may cause severe bleeding, hindering the effective removal of fragments.
In the MED technique, a partial laminectomy tube is directly docked on the lamina, followed by the removal of the outer laminar surface, cancellous bone, and thinning of the partial inner laminar undersurface using a high-speed burr to expose the dural surface. However, the direct contact of the dural surface under the lamina, without the protective cover of the ligamentum flavum, increases the risk of dural rent and tear. In cases of dural tears, conversion to open surgery is necessary due to the limited range of movement and restricted access within the tube, making suturing of the dural tear challenging, particularly in the axillary or lateral part of the dura.
Posterior endoscopic procedures, such as the UBE and monoportal techniques, which involve interlaminar approaches, require laminectomy and significant tilting of instruments or lamina removal to access the MacNab zone. This makes the upward approach challenging.
Our study shows comparable results with Ruetten et al. [12] and Schulz et al. [10,11] for endoscopic transforaminal approach used for MacNab hidden zone LDH. However, added advantage with our novel technique can overcome the limitation of endoscopic transforaminal approach [10,12,13].
In TPED, 2 techniques are commonly employed:
1. Outside in Technique
The floating technique involves anchoring the scope with a sheath in the foraminal area. The exiting nerve root is identified, and an approach is made from below the exiting nerve root/axilla to access the fragment. Instruments like the hook and RF ablator are introduced to create a pathway for the flexible grasper, enabling the capture and removal of the fragment.
2. Inside out Technique
The anchoring into the disc technique is more relevant when dealing with a large sequestered fragment that has a tail within the disc. In this method, the sheath is anchored inside the disc, and the rent in the disc and annulus junction is identified. By employing the RF ablator and hook, the collar of the rent is opened, allowing for the retrieval of the extruded fragment by catching its tail with the flexible grasper. However, this technique is not suitable for free-sequestered fragments.
The floating technique of TPED offers significant advantages for removing free-sequestrated fragments as it allows for visualization and safeguarding of the exiting and traversing nerve roots. After identification, surgical RF ablation is performed in the space between the exiting nerve root and vertebral body, creating a safer pathway to access the fragment. This approach provides adequate space between the axilla and the vertebral body, facilitating the creation of a glide path to reach the fragment. Importantly, the fragment can be removed without performing laminectomy/laminotomy or sacrificing any bone or vital structures. Consequently, the patient retains a functional spinal unit capable of supporting future activities.
Limitation of our study was single-level LDH and study had only L4–5, L5–S1 levels patients owing to less incidence of LDH into MacNab hidden zone and exclusion criteria. Number of patients were limited to 12 during this study period. A more focused study with higher number of patients and multicentric study needed to evaluate this technique in future.
CONCLUSION
In conclusion, TPED can be an ideal procedure for managing high-migrated zone 1 and zone 2 herniations in the hidden zone of MacNab, particularly at the L4–5 and L5–S1 levels. It offers minimal blood loss, deep sensory epidural anesthesia, and preservation of vital bony and muscular structures, thereby ensuring the complete functional preservation of the lumbar spine.