INTRODUCTION
Thoracic disc herniation accelerates the myelopathy at the level of thoracic stenosis caused by the ossification of the ligamentum flavum (OLF). Decompression surgery is required in patients presenting with neurological symptoms of thoracic myelopathy; thus, the thoracic OLF and disc herniation should be simultaneously treated.
Open en bloc laminectomy, with or without fusion, is commonly performed to treat thoracic OLF. However, owing to the invasiveness of open surgeries, endoscopic approaches for thoracic OLF, including full endoscopy and biportal endoscopy, have been attempted and have shown favorable outcomes with feasible surgical techniques [1-4].
Postoperative instability can occur if normal posterior structures in the cervicothoracic junction are damaged during surgery. The upper thoracic vertebrae, such as the cervical vertebrae, have smaller facet joints, lamina, and spinous processes. Therefore, preserving the midline and contralateral bony structures during bilateral canal decompression through a unilateral approach is technically demanding. Owing to the small facet joints of the upper thoracic vertebrae, excessive facet resection may be inevitable during thoracic discectomy through an endoscopic posterior thoracic approach.
Despite the anatomical disadvantages of the upper thoracic vertebrae, we successfully removed the bilateral thoracic OLF and disc herniation simultaneously while preserving the normal posterior thoracic structures and facet joints at the T2–3 level. The unrestricted use of both hands facilitates intimate drilling of the lamina, thoracic OLF, and facet joints. A small-diameter endoscope was used to visualize every corner of the spinal canal through a narrow extra space created by precise drilling.
MATERIALS AND METHODS
1. Case Presentation
A 50-year-old man presented with abrupt-onset motor weakness that progressed to his lower extremities 3 weeks ago. He complained of upper back and left chest wall pain and radicular pain in both legs. Neurological examination revealed that the motor power of his legs had decreased to grade 4 (of 5) and hypesthesia developed in both legs. He complained of difficulty with micturition. Clumsy and staggered gaits were observed. The Japanese Orthopaedic Association (JOA) score was 7.
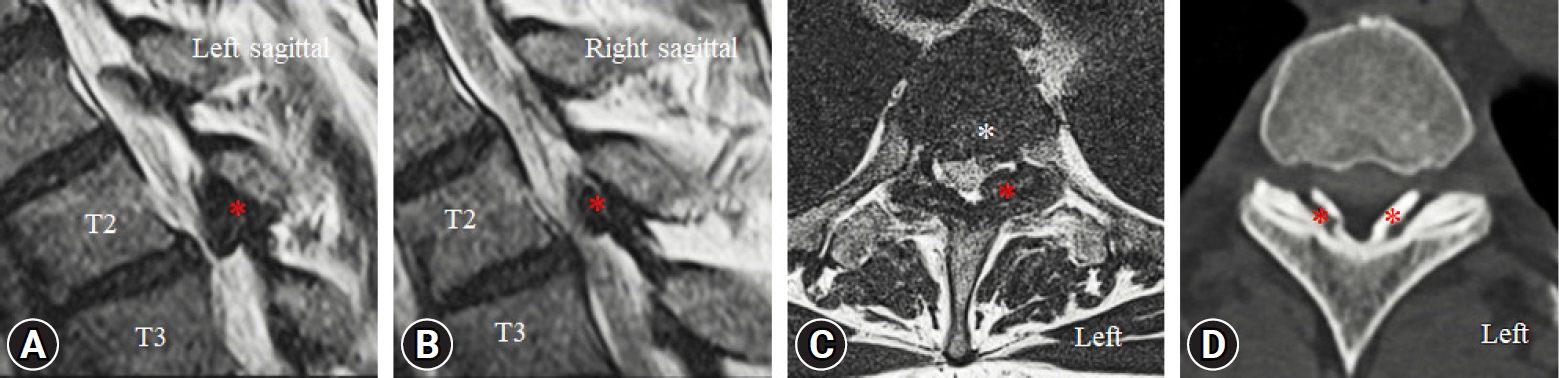
Preoperative T2-weighted magnetic resonance imaging (MRI) and computed tomography (CT) showed thoracic OLF in the bilateral spinal canal at the T2–3 level (Figure 1). Thoracic disc herniation was also observed, and the spinal cord was severely compressed between the prominent and herniated discs (Figure 1C).
The spinal cord was more severely compressed in the left spinal canal, and we performed a left-side biportal endoscopic approach to remove the thoracic OLF and herniated disc at the T2–3 level. This study was approved by the Wiltse Memorial Hospital Ethics Committee (NR-IRB 2022-W12).
2. Operation Technique (Supplementary Video Clip 1)
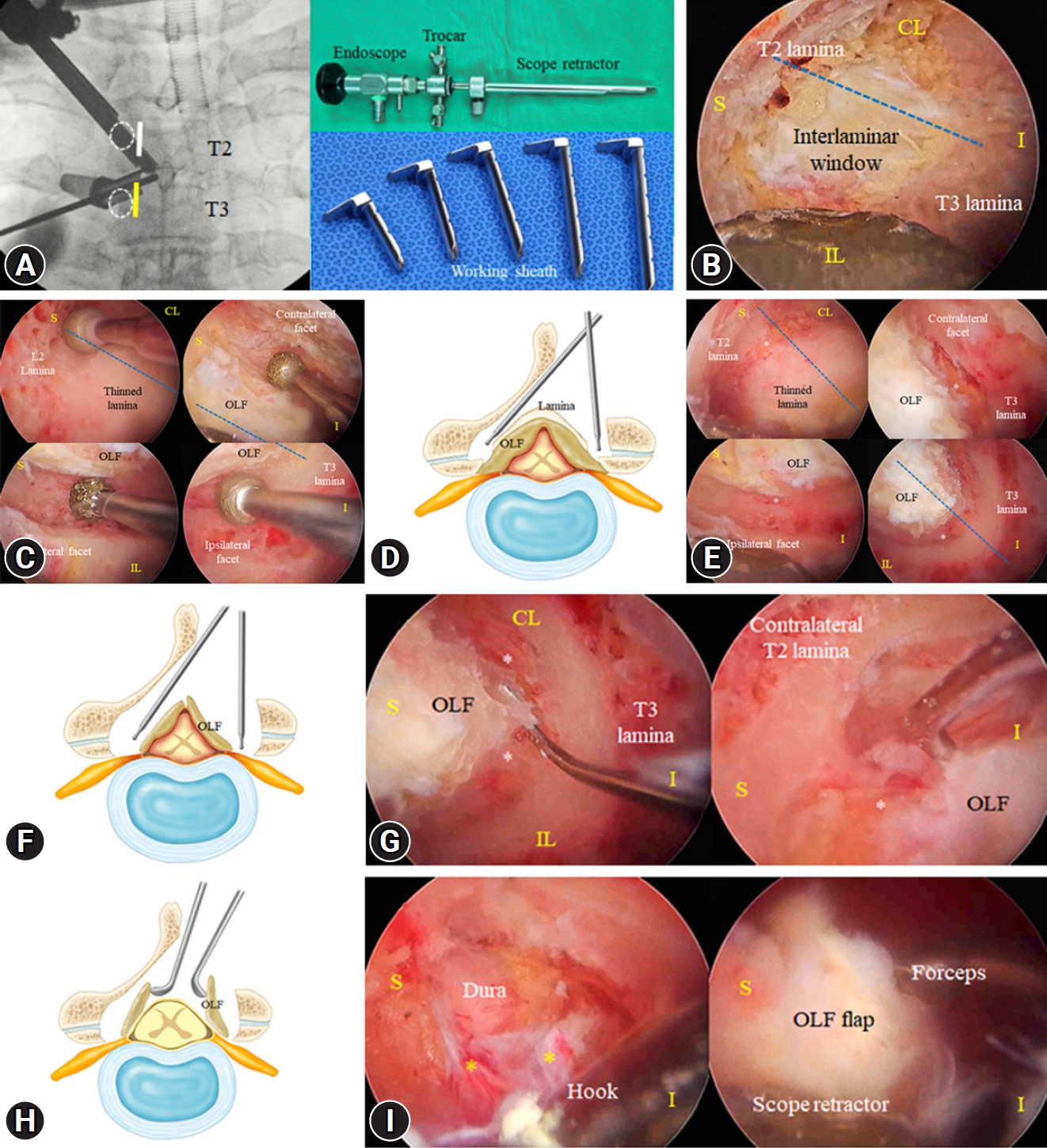
Patients underwent surgery under general anesthesia in the prone position on a chest bar or radiolucent Wilson frame. Under image intensification, 2 paramedian skin incisions were made on the medial border of the T2 and T3 pedicles to access the contralateral spinal canal and ipsilateral disc space at the T2–3 level (Figure 2A). We used biportal endoscopic systems (4 mm, 0° endoscope), a toolkit set, a customized scope retractor, and a working sheath (MD&Company, Seoul, Korea) [5-7]. A working sheath is essential for the smooth insertion of surgical instruments and drainage of irrigation fluid (Figure 2A).
The entire ipsilateral T2 lamina, upper part of the T3 lamina, facet joint, and bilateral interlaminar window were exposed after soft tissue dissection using a radiofrequency (RF) probe and forceps. Ipsilateral laminotomy, including the spinous process base, was performed using an endoscopic diamond drill to expose the bilateral interlaminar window (Figure 2B).
Cranial laminotomy was extended until the proximal end of the OLF and ligamentum flavum were exposed through the space created by sublaminar drilling. The cranial end of the laminotomy can be determined by identifying the superior articular process (SAP) tip or by confirming the intervertebral foramen under C-arm guidance because the OLF is usually thinned at the foraminal area. Subsequently, circumferential bony drilling was performed over the estimated boundary of the OLF, laterally with the bilateral medial facet joints, and caudally with the upper border T3 lamina (Figure 2B). The contralateral sublaminar space was created by drilling the cancellous bone of the T2 lamina while maintaining the inner cortical bone and preserving the outer laminar contour. The spinous process was also preserved, with the contralateral lamina attached (Figure 2B). The medial part of the SAP should be exposed after the initial bony drilling because the OLF is commonly fused with the SAP (Figure 2C, D).
After identifying the OLF contour, the remaining lamina and bulky OLF were thinned using a diamond drill for easy manipulation during en bloc OLF removal (Figure 2E, F). OLF thinning should be performed using a layer-by-layer pattern while the OLF is attached to the SAP. Subsequently, the cranial and caudal margins of the inner cortical bone were drilled to resemble a thin paper. The medial part of the SAP was drilled bilaterally along the lateral dural border until the epidural space was exposed (Figure 2E, F). The flap consisted of lamina, and the OLF was detached from the drilled bony edge using a fine dissector. The detached flap gradually floated from the dura when the edges were hooked using a fine hook (Figure 2G). As the flap floated, dural compression was partially relieved, which reduced the risk of spinal cord injury while manipulating the OLF flap. The secured OLF flap was elevated from the most movable area (Figure 2H). Epidural dissection was safely performed using fine dissectors, while holding the OLF flap with a scope retractor (Figure 2I). Subsequently, an entirely detached OLF flap was removed en bloc using forceps (Figure 2I). A sufficiently decompressed thecal sac with free dural pulsation was observed.
Diffuse epidural bleeding commonly occurs in the epidural vessels after OLF flap removal. A foamy hemostatic agent was used for hemostasis because excessive use of an RF probe for the epidural vessels can induce spinal cord thermal injury.
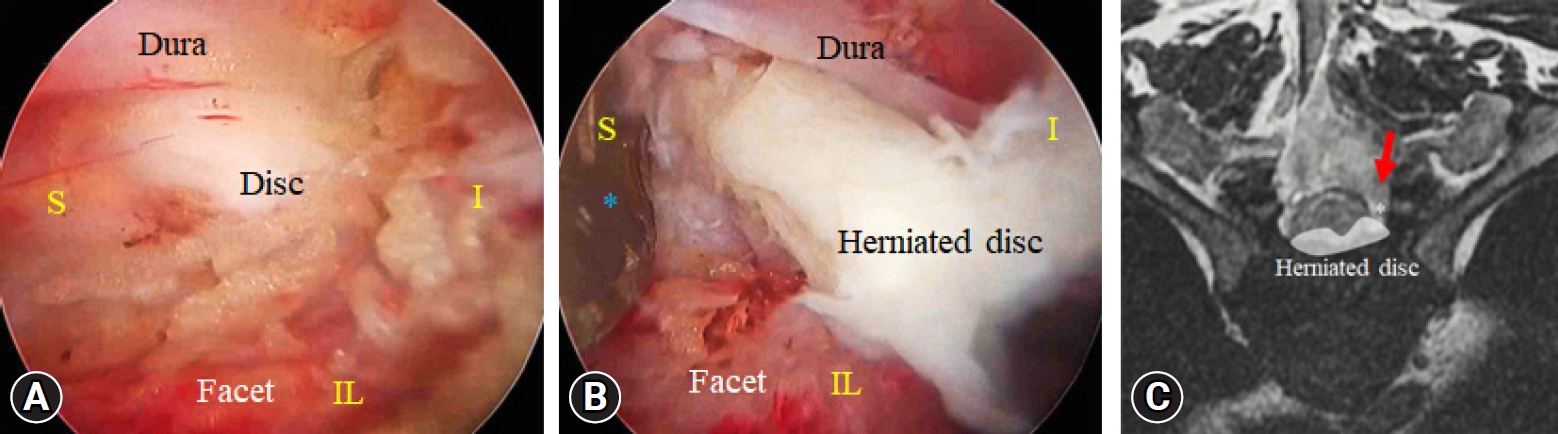
Small-diameter endoscopy advanced the lateral disc portion through the space created by the medial facet removal. As the small-diameter endoscope obliquely approaches the disc space, a broader endoscopic view is acquired to observe the lateral thecal sac and herniated disc. Under magnified endoscopic vision, a thoracic herniated disc was explored using dissectors (Figure 3A). Subsequently, the herniated disc was removed using forceps, while protecting the thecal sac with a scope retractor (Figure 3B, C). Skin wounds were closed by inserting a drainage catheter through the working portal. Blood loss during surgery was minimal, with a total surgical duration of 80 minutes.
RESULTS
Postoperatively, chest wall and upper back pain improved. Motor weakness of the lower extremities was enhanced to walk upstairs, and gait clumsiness improved after surgery. The radicular pain and numbness in both legs decreased. The hospital stay was 3 days. The postoperative JOA scores were 8 at 1 week and 10 at 4 weeks. After 10 months of follow-up, the patient could perform low-level exercises.
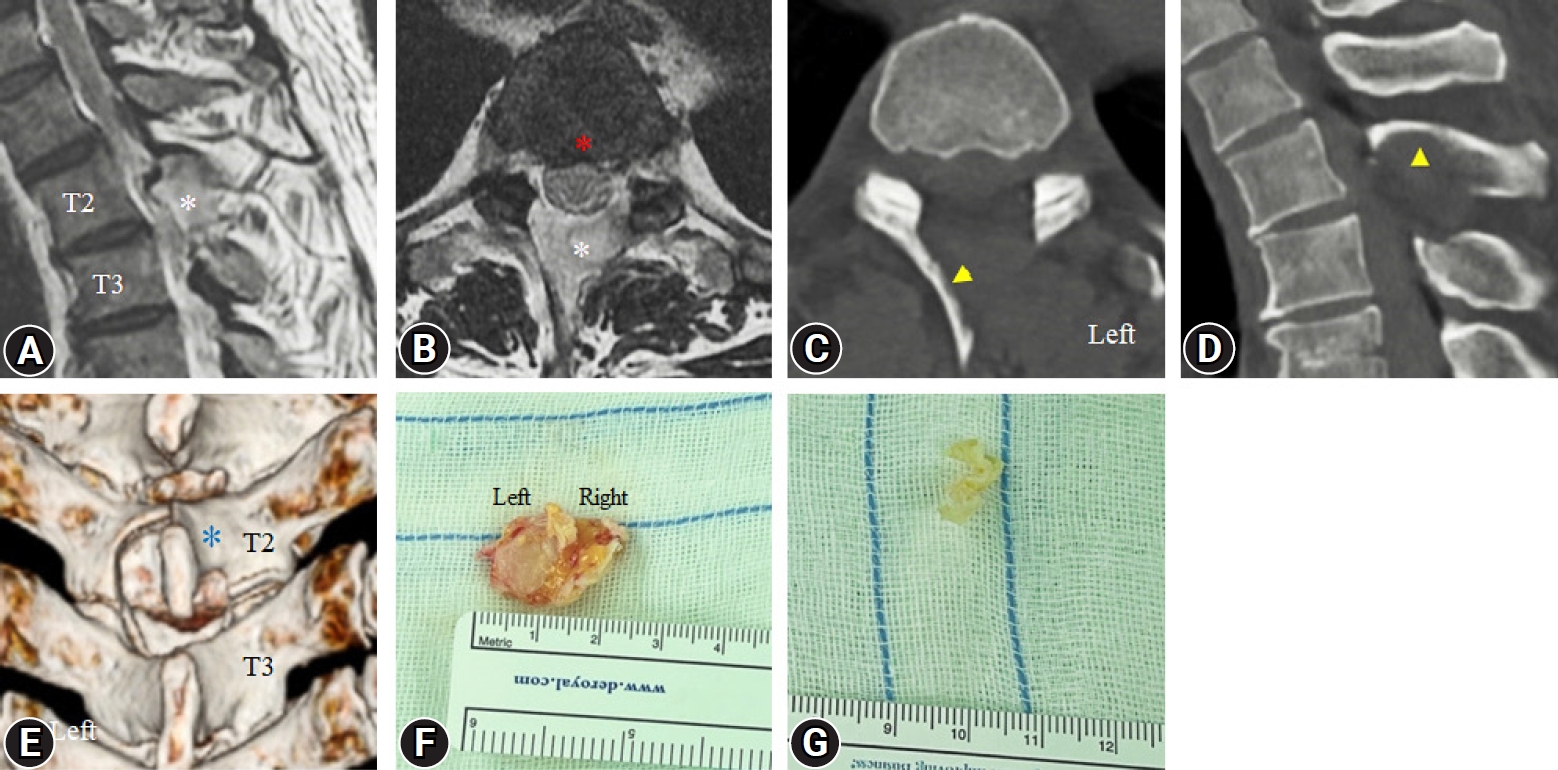
Postoperative MRI showed a sufficiently decompressed spinal canal after complete removal of the bilateral OLF and herniated disc at the T2–3 level (Figure 4A, B). Postoperative CT images revealed well-preserved contralateral lamina and spinous processes (Figure 4C–E). Although discectomy was performed through the endoscopic posterior approach, half of the ipsilateral facet joint was preserved (Figure 4C). An extracted OLF flap and herniated disc were observed (Figure 4F, G).
DISCUSSION
Thoracic OLF and disc herniation are common causes of thoracic spinal stenosis. The occurrence of thoracic disc herniation at the spinal level in thoracic OLF can accelerate spinal cord myelopathy. Two lesions should be treated simultaneously for complete neural decompression if surgical decompression is necessary.
The traditional surgical techniques for treating thoracic OLF include open microscopic laminectomy. However, these techniques are traumatic to the normal structures of the thoracic vertebrae, and posterior instrumentation is necessary in cases of wide laminectomy [8]. Compared with open laminectomy, minimally invasive surgery and endoscopic approaches reduce perioperative morbidity [9].
Endoscopic spine surgeries, including full endoscopy and biportal endoscopy, have evolved from lumbar discectomy to the current treatment of a wide range of degenerative diseases [10-14]. Full endoscopic thoracic approaches have been used for the treatment of thoracic stenosis and herniated discs. These full endoscopic techniques are feasible and have good surgical outcomes [1,3,15]. Biportal endoscopic surgery has also been described as a surgical technique for treating cervical and thoracic spondylotic myelopathy [4 6,16].
In patients with cervical or thoracic spondylotic myelopathy, the compressed spinal cord is vulnerable and may be injured, even with slight pressure exerted by the instruments. If piecemeal removal procedures are used for patients with myelopathy, repetitive insertion of the instruments between the dura and ligamentum flavum can cause irreversible spinal cord injury [17].
Therefore, among posterior thoracic endoscopic approaches, over-the-top decompression and en bloc removal techniques might have been considered safe and efficient surgical procedures to treat spondylotic myelopathy, minimizing dural manipulation. Recently, Kim et al. [1,17] described biportal endoscopic en bloc removal techniques for treating cervical spondylotic myelopathy and cervical epidural cysts, without complications [6,16]. Biportal and full endoscopic surgery use the en bloc removal technique to treat thoracic OLF and has shown favorable surgical outcomes.
We used the over-the-top decompression and en bloc removal technique to safely extract the thoracic OLF and hypertrophied ligamentum flavum at the T2–3 level. Preoperative CT images revealed a bilateral fused OLF without signs of dural ossification (Figure 1C) [18]. The midline portion of the OLF was fused to the lamina. If punches are inserted into the epidural space, additional compression of the spinal cord may induce irreversible cord injury. In this case, the en bloc removal technique might be a better surgical option for OLF resection than piecemeal removal. However, the half-and-half removal technique may be safer than en bloc removal procedure in the case of bilateral nonfused OLF (Figure 2H). Smaller halved OLFs offer easier manipulation of OLF and reduce the risk of spinal cord compression.
The bulky OLF should be thinned to resemble the inner cortical bone because bulky OLF can compress the spinal cord during OLF manipulation. The diamond drill slides the outer surface of the OLF and peels off the OLF in a layer-by-layer pattern. Sliding drilling procedures prevent compression forces on the spinal cord while thinning the OLF.
The upper thoracic vertebrae and cervicothoracic junction vertebrae are critical structures for the insertion of the upper back and posterior neck muscles. Preserving the upper thoracic spinous process and lamina is essential for maintaining neck and upper back muscle function. However, the upper thoracic vertebrae have smaller laminae, facet joints, and short spinous processes, such as the cervical vertebrae. Therefore, during the removal of the bilateral OLF from the unilateral side of the upper thoracic level, preserving the spinous process and contralateral lamina at the upper thoracic level is more technically challenging than at the lower thoracic level.
Despite the anatomical disadvantages of the upper thoracic vertebrae, we successfully removed the bilateral OLF and preserved the spinous process and contralateral lamina using a biportal endoscopic approach. A 3-mm diameter drill removed the cancellous bone of the contralateral lamina and created extra space for the smooth use of instruments in the contralateral spinal canal. A small-diameter endoscope (4-mm outer diameter) can also access the contralateral corners through the narrow sublaminar space. Therefore, intimate drilling can be performed under clear endoscopic vision by independently using the endoscope and drill in both hands (Figure 2B, C).
Choi et al. [15] reported percutaneous endoscopic thoracic discectomy via a transforaminal approach; this technique has been mainly used for full endoscopic thoracic discectomy than the interlaminar approach because of the narrow interlaminar space in the thoracic vertebrae. However, bilateral thoracic canal decompression is impossible through the transforaminal approach if thoracic disc herniation is combined with spinal canal stenosis. Similarly, the full endoscopic interlaminar approach can be used to successfully treat thoracic spinal stenosis. However, discectomy through the interlaminar space is challenging because the space created lateral to the thecal sac is narrow for working cannula insertion, even with wide-facet resection.
Biportal endoscopy allows access to the intervertebral disc space through the space created by medial facet drilling. The extra space created by medial facetectomy (approximately 50%) is sufficient for unrestricted access of the endoscope and forceps to the disc space. The medial oblique angle of endoscopic access offers a broader endoscopic view of the lateral thecal sac and intervertebral disc space even through a narrow corridor. The scope retractor in the endoscopic hand was moved independently for neural protection. Subsequently, the forceps could smoothly access the herniated disc while protecting the spinal cord with a scope retractor.
Although this technique has remarkable advantages, biportal endoscopic thoracic OLF removal and discectomy should be considered in selected patients who have bilaterally fused OLF without dural ossifications. We recommend the half-and-half removal technique if the OLF bisection is feasible to reduce spinal cord compression during OLF manipulation as Kim et al. [17] described. This technique may not be suitable for patients with prominent calcified disc herniation or centrally located disc herniation. Excessive neural retraction is inevitable to resolve these lesions, even with wide-facet resection. Open surgery with wide laminectomy should be performed in patients with definite dural ossification signs [18] and Sato classification of tuberous types [19] on preoperative CT images.
Continuous saline infusion pressure in the spinal cord may increase epidural pressure and induce spinal cord injury [20]. We should carefully monitor the patency of the saline outflow and recommend saline infusion pressures below 30 mmHg. If incidental durotomy occurs during surgery, the hole should be repaired using a fibrin sealant patch or sutureless clip. However, if endoscopic repair fails, open microscopic surgery should be performed for complete dural repair [21].
CONCLUSION
Disc herniation can worsen myelopathy caused by thoracic OLF. We completely removed the thoracic OLF and the herniated disc through a biportal endoscopic posterior approach. Biportal endoscopic surgery enables the smooth use of drills and instruments in the narrow spinal canal of the upper thoracic vertebrae. The biportal endoscopic posterior thoracic approach may be an attractive surgical option for the treatment of thoracic myelopathy caused by combined degenerative pathologies. However, this technique should be performed in selected patients after obtaining abundant experience with endoscopic spine surgeries.