INTRODUCTION
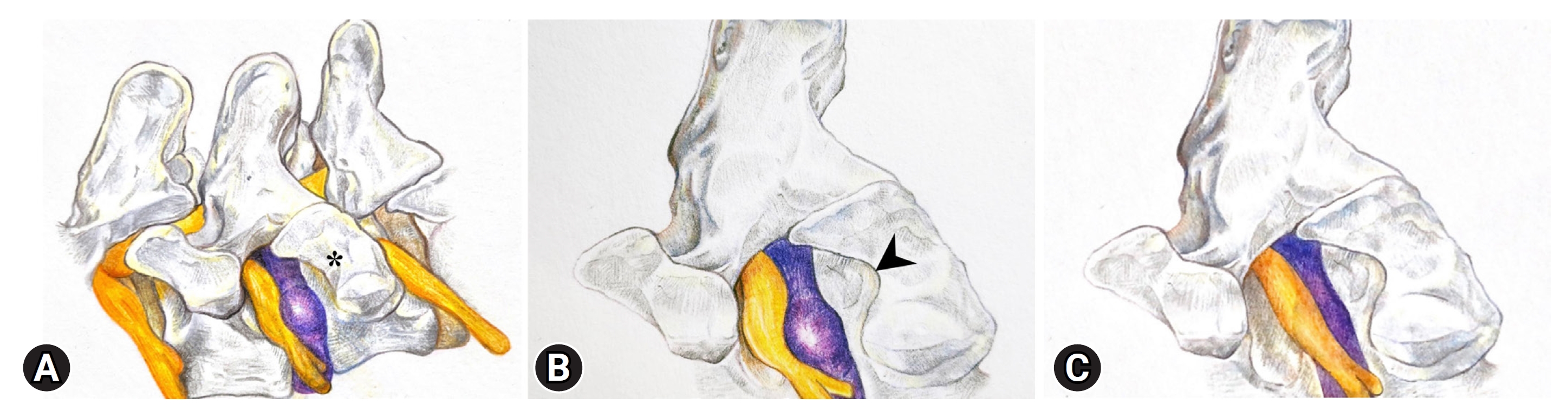
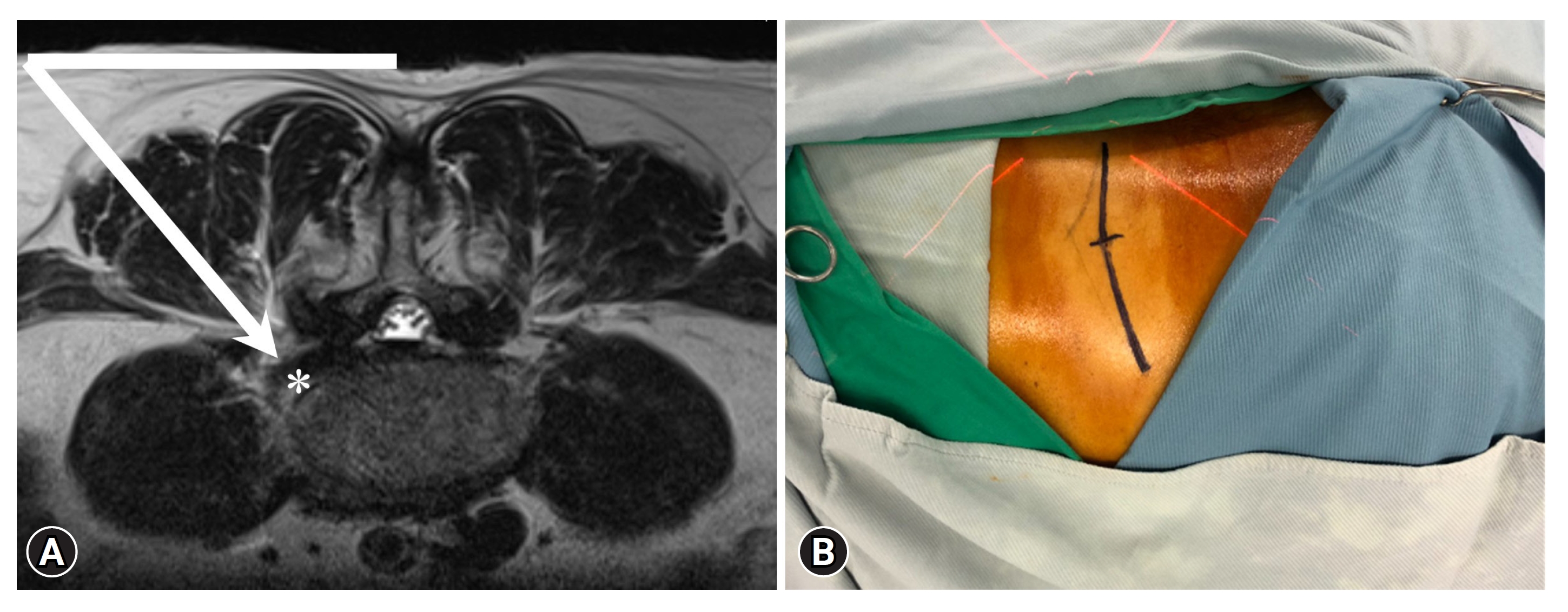
Extraforaminal lumbar disk herniation (E-LDH) constitutes 7%–12% of all types of lumbar disk herniations [1,2]. In the case of E-LDH, the herniated disk protrudes beyond the neuroforamen, compressing the nerve roots and resulting in symptoms such as lower extremity pain (Figure 1A) [3]. Conservative treatments like physical therapy and medication can provide relief, but surgery is often required. Conventional surgical techniques, like using a midline or paramedian approach with medial facetectomy, and total facetectomy can effectively remove E-LDH [4-6]. However, these methods frequently result in spinal instability, necessitating additional spinal fusion procedures [7]. Minimally invasive approaches such as full-endoscopic lumbar discectomy are a technique that provides directly access to the disc herniation by inserting an 8-mm working sheath with an endoscope without dissecting surrounding structures [8]. Although conventional transforaminal approach with either inside-out or outside-in technique can effectively remove E-LDH, a certain number of patients were expected to have postoperative dysesthesia (POD) or nerve root injury following manipulation of the endoscopic instruments [9-11]. The following case report describes a challenging case who could not lie prone before the endoscopic procedure due to experiencing severe lower extremity pain on the left. This technical note discusses the L3 nerve block under fluoroscopy guidance before the extraforaminal full-endoscopic approach for E-LDH discectomy.
CASE REPORT
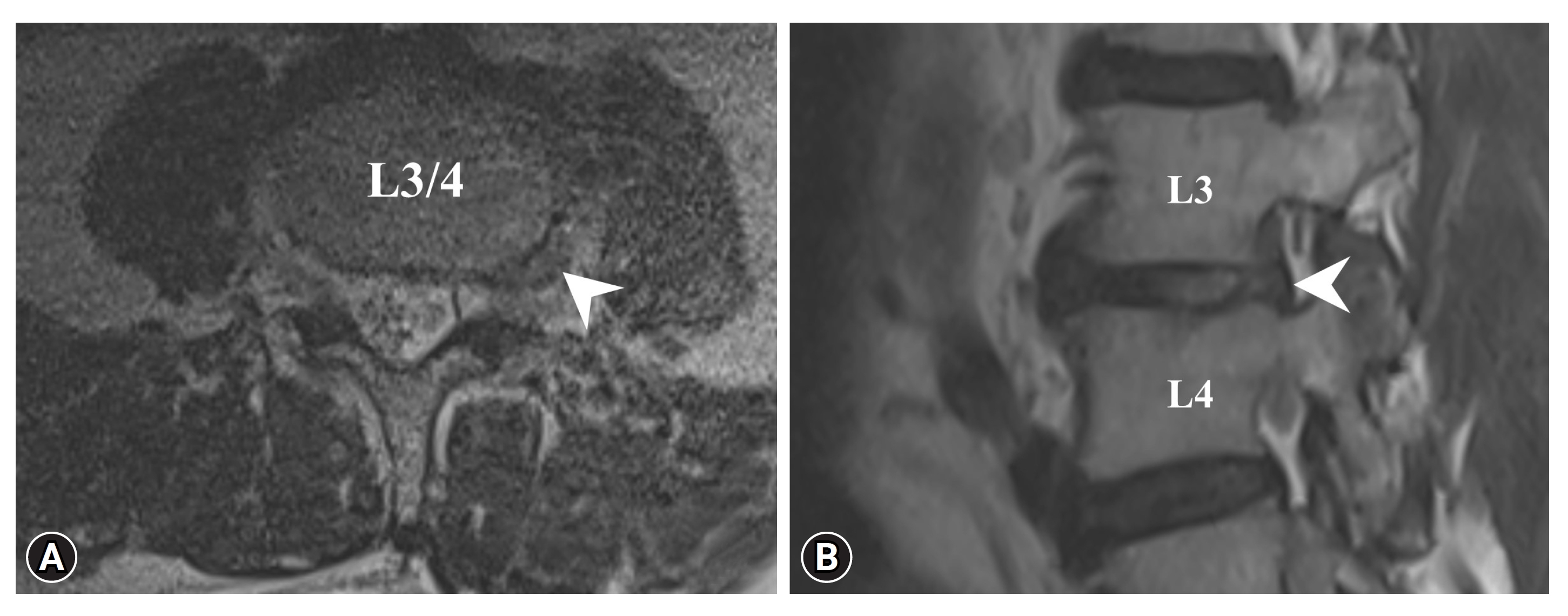
A 62-year-old male with a medical history of congestive heart failure with reduced ejection fraction, coronary artery disease with 2-vessel disease with previous stent placement, essential hypertension, and type 2 diabetes mellitus was admitted to the hospital due to progressive left back pain and difficulty ambulating for 3 days. The pain was severe, that is visual analogue scale (VAS) score 10 out of 10 and radiated to the left thigh and knee. He could only be relieved from the pain when lying down on the right side with hip flexion. The patient had tingling sensations and weakness in the left leg as well. Physical examination demonstrated numbness over L3 dermatome, muscle power decreased 4 out of 5 over left knee extension. Left big toe extension showed 5 out of 5. Magnetic resonance imaging (MRI) revealed an E-LDH at L3/4, causing impingement of the exiting nerve root (Figure 2A, B). Initially, conservative treatment was offered, but due to the patient's unmanageable pain, he requested surgical intervention.
SURGICAL PROCEDURE
1. Preoperative Procedure (The L3 Nerve Root Block)
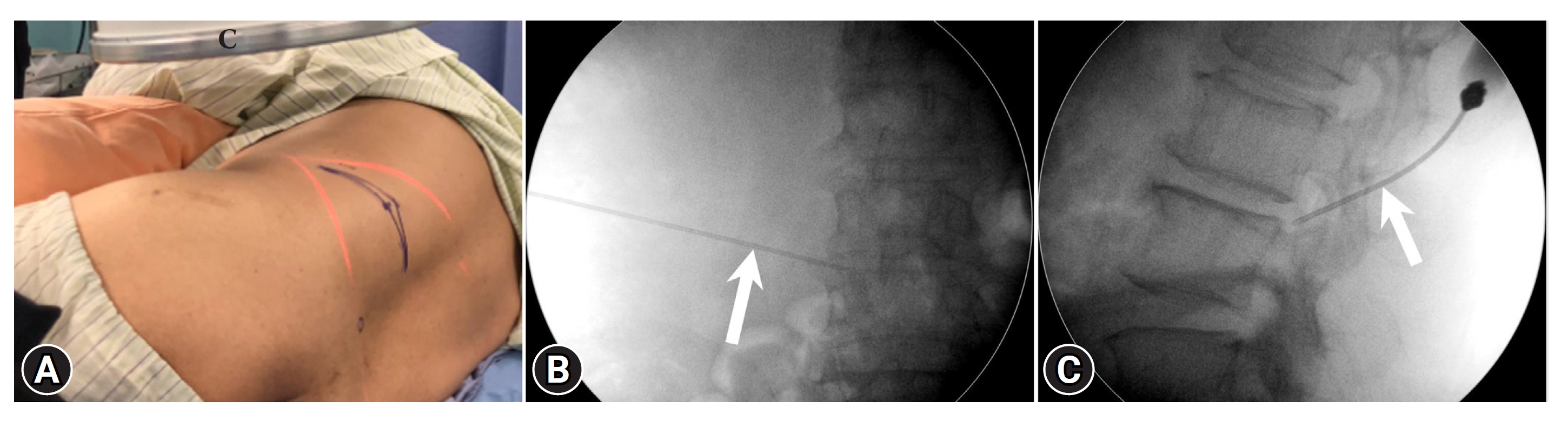
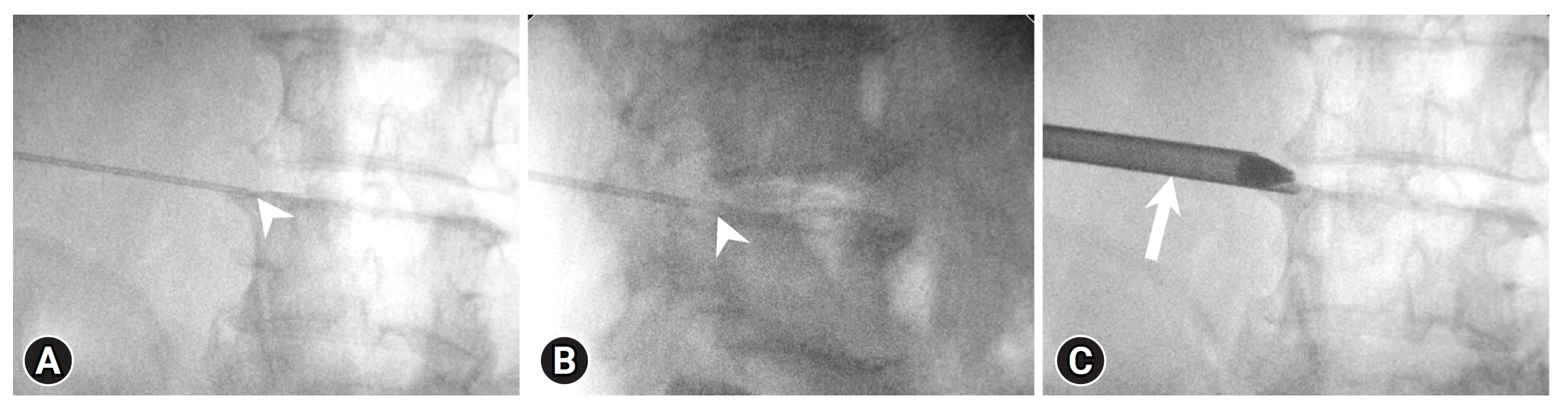
As he was experiencing severe left lower extremity pain, he could not lie prone on a radiolucent table. In the right decubitus position, with hips and knee flexed on the table (Figure 3A), the entry point and the trajectory were determined on the skin using anteroposterior (AP) and lateral fluoroscopy. After local anesthesia at the entry point, a spinal needle was inserted. The needle’s tip reached the ipsilateral medial interpedicular line (Figure 3B), posterior to the posterior vertebral line (Figure 3C), about 3–5 mL 0.25% diluted lidocaine solution was injected slowly for L3 nerve root block.
2. Patient Position and Skin Marking
After the nerve block, the pain on the left lower extremity partially decreased immediately. The patient was positioned in a prone on the radiolucent table, with his hips and knee flexed. The entry point was determined to be about 8–9 cm from the midline (Figure 4A), the cross section of the trajectory line towards the base of superior articular process (SAP) of L4, obtained from AP and lateral fluoroscopy (Figure 4B).
3. Needle Puncturing and Placing of the Working Cannula
Following the preoperative planning of the entry point and trajectory, the patient received local anesthesia using 1% lidocaine. Subsequently, an 8-mm stab incision with No.15 blade was made. Then, the cannulated needle was inserted through the entry point and advanced along the intended trajectory until it reached the base of the SAP. While inserting the needle into the lateral aspect of the SAP, we infiltrated approximately 5 to 10 mL of 1% lidocaine into the muscle layer [12]. Upon reaching the lateral aspect of the base of the SAP, tactile feedback from the bone was detected (Figure 1A), and the needle position was confirmed using fluoroscopy assistance. We injected approximately 5 mL of 0.25% lidocaine to infiltrate and dissect the surrounding soft tissues of the SAP. Once the needle’s position was confirmed through AP and lateral fluoroscopy (Figure 5A, B), a guide-wire was introduced through the cannulated needle. The guide-wire was then used as a pathway, and sequential dilator was employed to create the necessary track for the working cannula. After confirming the tip of the working cannula with fluoroscopy, the dilator was removed. To avoid irritating the nerve root and the dorsal root ganglion (DRG), the working cannula was not rotated (Figure 5C).
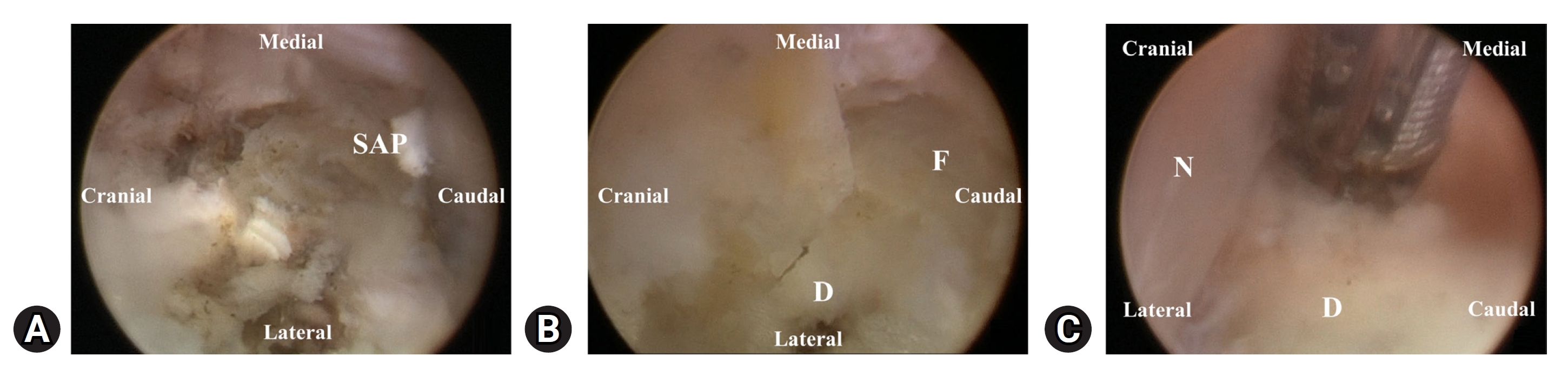
4. Foraminoplasty Under Endoscope
The endoscope with 4.3-mm working channel (Spinendos GmbH, Munich, Germany) was inserted through the 8-mm working channel. The procedure was performed under continuous saline irrigation. To establish the boundaries of the SAP, a radiofrequency (RF) coagulator (Vantage Biotech Co., Ltd., Taoyuan, Taiwan) along with grasping forceps was used to carefully isolate the surrounding soft tissue. The area is well-vascularized, and maintaining good hemostasis is key to the successful procedure. The SAP was demarcated under the endoscopic visualization (Figure 6A). For enlarging the working space in the neuroforamen, a high-speed diamond burr (Vantage Biotech Co., Ltd.) was used to drill the base of the SAP (Figures 1B, 6B). Subsequently, the forceps were employed to excise the foraminal ligament. The disc in the foraminal region was partially removed with forceps or reduce in size using the RF coagulator to create more space for the surgical instruments (Figure 6B).
5. Extraforaminal Discectomy
After performing foraminoplasty and removing the foraminal part of the disc, the endoscope was rotated cranially without rotating the working sheath, allowing for the visualization of the nerve root with the extraforaminal bulging disc underneath (Figure 6C). The E-LDH that was causing impingement on the nerve root and DRG was carefully removed using forceps (Figure 1C). Hemostasis was done meticulously maintained using the RF coagulator during the procedure to ensure clear visualization of the surrounding structures.
6. Final Checking Point
With the use of local anesthesia, both the patient and the surgeon could maintain communication throughout the procedure. The patient expressed immediate pain relief after the extraforaminal discectomy. Under endoscopic visualization, a ball-tip probe was used to check for any remnants beneath the nerve root. We also confirmed the nerve root was freely mobilized. To identify any remaining invisible disc fragments, the patient was asked to perform certain maneuvers (such as coughing and hip flexion and extension while lying prone) to increase pressure on the disc. In some cases, remnant discs would bulge out in the area where discectomy was performed. Ensuring the removal of these remnant discs was essential to decrease the risk of recurrence. A drain was not inserted as meticulous bleeding control was achieved using the RF coagulator. Closure of the surgical wound was done with a single 4-0 polyglactin 910 stitch.
RESULTS
The VAS score for leg pain reduced significantly from 10 to 0 right after the procedure. The patient was ambulated from the next day following the procedure with the lumbar support. At the end of 6-months follow-up period, the patient’s leg symptom completely improved, with no associated back pain.
DISCUSSION
Conventional transforaminal endoscopic discectomy has shown positive clinical results in the treatment of E-LDH [13]. However, it is not without complications, such as POD caused by irritation of DRG, and the nerve root injury [9,10]. To address these complications, modified transforaminal or various types of extraforaminal endoscopic discectomy for E-LDH have been described in the past decades [14-18].
Our procedure was performed under local anesthesia, even though the patient was uncooperative due to excessive pain in the left leg. There are multiple benefits to using local anesthesia in order to minimize various complications. Firstly, patients with comorbidities such as severe heart failure as seen in this case, may benefit more from local anesthesia than general anesthesia [19]. This approach helps to reduce the risk of complication associated with general anesthesia. Secondly, it allows for continuous communication with the patient during the procedure, enabling immediate feedback and thus reducing the risk of nerve root injury. Thirdly, monitoring the improvement of leg pain assists in reducing the incidence of inadequate decompression. Additionally, maneuvers like coughing and hip movements can be performed under local anesthesia to identify any remaining discs and decrease recurrence rates. The successful management under local anesthesia was facilitated by the preoperative L3 nerve block. Instead of using 1% lidocaine, which would cause complete paralysis of the nerve root and impede immediate feedback, a diluted 0.25% lidocaine was used to provide partial pain relief, allowing for better patient cooperation during the procedure.
Preoperative planning based on the MRI determined that the entry point was about 8–9 cm away from the midline, which is consistent with the published conventional transformainal approach for E-LDH [20]. However, in our technique, the spinal needle was punctured to the base of SAP instead of the tip, allowing our surgical instruments to remain at the base of the SAP [21]. The working sheath does not go through the neuroforamen or entry into the epidural space, differentiate it from the conventional transforaminal approach.
POD is a common complication that significantly impacts patient satisfaction following transforaminal endoscopic procedures and delays the patient’s return to work. The incidence of POD incidence varies widely (from 9.7% to 29%) and is frequently underreported due to the absence of established diagnostic criteria [9-11]. During conventional transforaminal endoscopic discectomy, manipulation of the working sheath within the Kambin triangle carries the potential for compressing, irritating, and harming DRG or exiting nerve root, thereby leading to POD and nerve root injury [9]. Unlike the central and peripheral nervous systems, DRG lacks a protective barrier, rendering it more susceptible to injury [22]. Our technique is designed to minimize the risk of DRG irritation by maintaining the working sheath at the base of the SAP without sheath rotation.
Foraminoplasty is a procedure intended to widen the neural foramen. Various tools, including bone trephines, can be employed to perform foraminoplasty [23-25]. Although foraminoplasty with bone trephines is effective, it may be associated with an increased potential for nerve injury and uncontrollable bleeding. In contrast, the use of a high-speed diamond burr enables bone removal and hemostasis under endoscopic visualization [25]. We utilized the burr to drill the base of the SAP without damaging the facet joints. Through foraminoplasty, we could facilitate the removal of the foraminal disc using forceps, as well as address the extraforaminal herniated discs, without irritating DRG or the nerve root.
The crucial key points for this surgical technique are as follows: (1) Peripheral nerve block with a 0.25% lidocaine injection to partially alleviate leg pain before the upcoming procedure in the prone position; (2) Precise docking of the working cannula without excessive manipulation; (3) Maintaining effective hemostasis during the procedure to enhance the identification of surrounding structures and prevent damage to the nerve root; (4) Utilizing a high-speed diamond burr for precise drilling of the base of the SAP, aiding in the subsequent discectomy; (5) Removing the disc within the neuroforamen first to create more space for surgical instruments before addressing the extraforaminal portion; (6) Instructing patients to perform certain maneuvers to increase the intervertebral disc pressure, facilitating the removal of remnant discs. This approach is designed to reduce the incidence of recurrence.
This technique has its own limitation such as its high technically demands, requiring precise docking and bony drilling with a high-speed diamond burr to avoid POD, nerve root injury, and spinal instability.