INTRODUCTION
Lumbar extradural schwannoma are uncommon, accounting for 2.4%–3.2% of all nerve sheath tumors [1,2]. Their rarity has prohibited methodologic examination in order to establish an optimal surgical approach for treatment [1]. Rather, the surgeon must consider the individual tumor’s size, location, and involvement of adjacent structures when selecting a surgical approach. Traditional anterior open or laparoscopic retroperitoneal approaches require an access surgeon and extensive mobilization of the viscera. Posterior midline or paraspinal approaches have been employed with good results. However, these approaches involve disruption of muscular and ligamentous attachments, laminectomy, total or medial facetectomy, and possibly instrumented fusion for spinal instability [3].
Minimally invasive surgical (MIS) techniques have garnered increasing popularity in treating a variety of spinal pathologies due to their associations with less soft tissue disruption, decreased blood loss, and shorter hospitalizations [4]. More recently, Benjamin et al. [5] reported the use of a MIS lateral transpsoas approach for the successful resection of an extraforaminal L4 nerve root schwannoma. The lateral retroperitoneal transpsoas approach as described by Ozgur et al. [6] obviates the need for an access surgeon, and should present the most direct approach to an extraforaminal lumbar nerve sheath tumor. In this report, we describe our experience with the use of a minimally invasive lateral transpsoas approach for resection of an extraforaminal L3 nerve root schwannoma. We provide a review of the literature on minimally invasive lateral surgical approaches to extraforaminal schwannomas and discuss technical challenges of consideration to the surgeon.
CASE REPORT
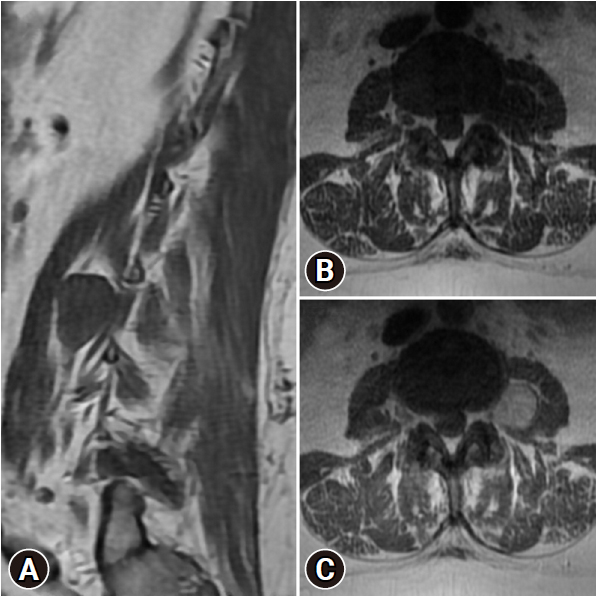
A 53-year-old obese (body mass index [BMI], 42.3 kg/m2) female presented with over 1 year of progressive pain and numbness across the left anteromedial thigh. Physical examination revealed grade 4 out of 5 weakness in her left iliopsoas and hyperesthesia in the left L3 dermatome. Lumbar spine magnetic resonance imaging (MRI) demonstrated a 24 × 23 × 24-mm well-circumscribed, T2 hyperintense, homogenously enhancing mass within the left psoas muscle. The mass was contiguous with the extraforaminal L3 nerve root and avidly contrast enhanced (Figure 1). No additional masses were seen on cervical and thoracic spine MRI. Electromyography (EMG) and nerve conduction studies were unremarkable.
Based on the imaging findings, a benign nerve sheath tumor such as schwannoma or neurofibroma was favored. A traditional anterior approach was discussed with the patient. As the bulk of the mass was within the psoas muscle, we elected for a minimally invasive lateral retroperitoneal approach.
1. Surgical Approach
A minimally invasive lateral transpsoas approach as previously described by Boah and Perin [7] was used. Briefly, the patient was placed in lateral decubitus position and C-arm fluoroscopy used to localize the appropriate vertebral level. Using O-arm neuronavigation, a vertically oriented incision was made with subsequent blunt dissection of the oblique and transverse abdominal muscles. The transversus fascia is identified and opened bluntly in order to expose the retroperitoneal fat over the level of interest. A self-retaining retractor system (Phantom XL3, TeDan Surgical Innovations, Sugar Land, TX, USA) was inserted over the surface of the psoas muscle and the exoscope (Modus V, Synaptive Medical, Toronto, ON, Canada) brought into the field for microsurgical dissection.
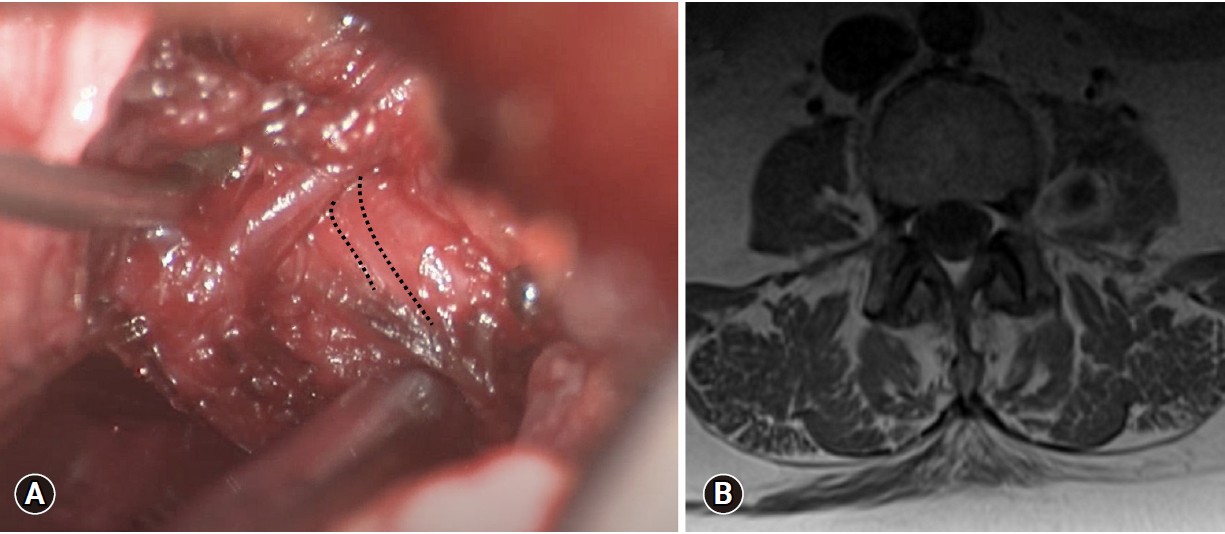
The psoas muscle was carefully dissected parallel with the muscle fibers in order to identify the intramuscular mass. Intraoperative neuromonitoring (IONM) consisted of continuous somatosensory evoked potentials and continuous and evoked EMG. Using direct simulation, the L3 nerve root was identified and found to be splayed over the lateral portion of the mass (Figure 2A) based on IONM. A narrow safe working window without overlying nerve was identified at the anterior aspect of the tumor. The capsule was coagulated and incised to allow for central suction aspiration and pituitary rongeur debulking. Frozen section specimens returned intraoperative as schwannoma. Unfortunately, the positioning of the overlaying nerve root did not allow for further safe debulking of the superior and lateral portions of the mass. After debulking, the nerve stimulated easily and appeared significantly decompressed. Hemostasis was achieved, the retractor system removed, and incisions closed in the usual fashion.
2. Follow-up
The patient did well postoperative, with immediate improvement in her pain and left iliopsoas strength improving to 5 out of 5. Postoperative MRI (Figure 2B) demonstrated debulking of the anterior and inferior portions of the mass, although residual tumor remained. Final pathology was consistent with schwannoma. At most recent 3-month follow-up, she continues to be full strength with significant pain relief.
Informed consent was obtained from the patient prior to publication.
DISCUSSION
Extraforaminal lumbar schwannomas are an exceptionally uncommon clinical entity, representing 0.7%–4.2% of all extradural schwannomas [2,8]. Mainstay of treatment is gross total surgical resection with preservation of the involved nerve root, which is generally curative and associated with limited morbidity [9,10]. However, methodical establishment of optimal surgical strategies for this subgroup of tumors is lacking due to their rarity [1]. As such, the surgeon must consider tumor size, location, and involvement of adjacent structures when selecting a surgical approach.
The traditional approach for these tumors is an open anterior retroperitoneal approach with or without laparoscopic assistance which afford early visualization and isolation of the major vasculature. However, these anterior techniques are limited in their approach of foraminal tumors and do not allow for utilization of a stimulator probe for early identification of nerves. Midline and paraspinal posterior approaches have also been described, and involve total- or hemilaminectomy and/or total or medial facetectomy [3]. For tumors requiring extensive bony resection or those tumors with greater spinal canal or foraminal disease, a posterior approach may be suitable. Concomitant arthrodesis and instrumentation may be necessary to reduce the risk of spinal instability, further adding to surgical morbidity [3,11,12]. In recent years, a number of mini-open or MIS approaches to lumbar extraforaminal schwannomas have been described [12-16]. Minimally invasive techniques allow for less muscle and ligamentous disruption, are associated with less blood loss, and shorter postoperative length of stay, thus lessening surgical morbidity [4,15]. These methods can be of particular importance in obese patient populations that have an even greater risk of postoperative blood loss, surgical site infection and nerve injury with lumbar spine surgery [17].
There have been 4 previous reports of extraforaminal lumbar schwannomas resected via a minimally invasive lateral retroperitoneal transpsoas approach (Table 1) [5,7,13,18]. This approach, adopted from extreme lateral interbody fusion, described by Ozgur et al. [6] permits the use of directional and continuous EMG monitoring along with more direct, less traumatic exposure of extraforaminal tumors. First report of minimally invasive lateral resection of an extraforaminal lumbar plexus schwannoma was presented by Lee and Srikantha [18] in 2016. A mini-open approach achieved complete resection of a 52-mm schwannoma within the psoas muscle at L4–5, followed by L4–5 discectomy and fusion for grade 1 anterolisthesis. Postoperative, the patient had new grade 4/5 iliopsoas weakness which resolved at 3-month follow-up. Benjamin et al. [5] and Boah and Perin [7] each reported successful complete resection of smaller extraforaminal lumbar schwannomas without complications at 12-month follow-up. Most recently, Safaee et al. [13] reported complete resection of a 41-mm extraforaminal right L2 schwannoma. The patient’s preoperative 4/5 iliopsoas and quadriceps weakness improved to 4+/5 and 5/5, respectively, with slight anterior thigh numbness at time of discharge on postoperative day 2. However, they do not provide long-term clinical follow-up.
Our case highlights important limitations of these minimally invasive techniques. Position of the parent nerve in relation to tumor cannot be reliably discerned on conventional MRI, and may only be discovered upon operative examination. Inopportune lateral splaying of the nerve can prohibit a nerve sparing gross total resection resulting in subtotal resection in order to preserve the nerve root and avoid significant functional motor status morbidity, as occurred in the case discussed by this paper. This also highlights the importance of IONM and direct neural stimulation. Splayed nerves may not appear visually distinct from tumor and lead to inadvertent sacrifice and postoperative deficit. Another undescribed limitation of this approach is body habitus and the long working corridor a large body habitus can necessitate. Despite the technical challenges that led to a subtotal resection, the patient’s neurologic examination and radiculopathy improved. It is therefore reasonable to consider this type of minimally invasive approach to such pathologies when stratifying risk with the understanding that gross total resection may not always be feasible and safe.
Nevertheless, the MIS lateral transpsoas approach allowed for debulking and decompression of the nerve root with sustained symptom relief. Traditional anterior and posterior approaches were considered in our patient. Given her age and BMI, a posterior approach with hemilaminectomy and medial facetectomy was felt to present considerable risk of postoperative instability necessitating instrumentation and fusion [19]. Lateral transpsoas approaches are not without risk of injury to the lumbosacral plexus due its proximity, which moves more anteriorly at lower levels [20]. Complications are exceptionally rare and IONM further reduces rate of complications to less than 1% [21]. For select extraforaminal lumbar nerve sheath tumors, a MIS lateral retroperitoneal approach provides a direct, safe working corridor for resection and improvement of patient symptoms.
CONCLUSION
Extraforaminal lumbar schwannomas are an uncommon pathology presenting a complicated surgical paradigm. The MIS lateral transpsoas approach provides direct access for select tumors, while affording the benefits of reduced tissue disruption, blood loss, and postoperative length of hospitalization. Total tumor resection may be inhibited by body habitus and intraoperative discovery of unfavorable nerve root position in relation to tumor, thus demonstrating limitations to this approach. However, substantial nerve decompression and symptomatic relief through subtotal tumor resection may be the most suitable for benign pathologies in order to minimize morbidity in more complex cases.