AbstractAlthough the conventional anterior approach is the gold-standard procedure for multilevel cervical spondylotic radiculopathy, the fully-endoscopic posterior approach has recently become more popular. We present the case of a 73-year-old female patient with neck pain radiating to right shoulder and arm. The patient had adjacent-level cervical foraminal stenosis at C5–6 and C6–7 on right side and was managed with modified fully-endoscopic posterior foraminotomy at C5–6 and C6–7 with total pediculectomy of C6. The patient exhibited excellent clinical results, without any instability during long-term follow-up. Fully-endoscopic posterior cervical 2-level foraminotomy using total pediculectomy can be applied in patients for whom the anterior cervical approach is contraindicated, with the added advantages of the minimally invasive posterior approach. The technique has an extensive learning curve and needs to be selected according to the pathology.
INTRODUCTIONConventional anterior approach (anterior cervical discectomy and fusion or anterior cervical disc replacement) is well established surgical option for single or multilevel cervical spondylotic myelopathy due to its excellent clinical results and high fusion rate [1]. Though the anterior approach is widely used technique; it is associated with the access related several complications [2,3]. Full-endoscopic cervical discectomy consists of 2 approaches; anterior approach called as anterior full-endoscopic cervical discectomy while posterior approach called as posterior full-endoscopic cervical foraminotomy and discectomy (PECFD) [4,5]. Although, PECFD is less soft tissue destructive it is limited by its indications to the single level, paracentral and foraminal pathologies. We present probably first case report of adjacent-level cervical foraminal stenosis managed with full-endoscopic posterior foraminotomy and pediculectomy.
CASE REPORTWe present a case of 73 years’ female with neck pain radiating to right shoulder and arm in the last 3 months with a visual analogue scale (VAS) score of 5 for neck and 9 for arm. She was having multiple medical comorbidities and operated for carotid angioplasty in recent past. Clinically, cervical range of movements was grossly restricted with positive spurling test. The neurological examination revealed right hand grasp power weakness (grade 4) and sensory deficit along C6 distribution.
Plain radiograph of cervical spine revealed degenerative spondylolisthesis C5 over C6. Computed tomography and magnetic resonance imaging scan examination revealed severe right cervical foraminal stenosis at level C5–6, C6–7 (Figure 1). Patient was planned for full-endoscopic posterior cervical C5–6, C6–7 foraminotomy with right C6 total pediculectomy.
Informed consent was obtained from all individual participants included in the study. The patient and next of kin has given informed written consent for the submission of a case report to the journal. Present case report complies with the CARE (CAse REports) 2013 guidelines.
SURGICAL TECHNIQUEPatient was placed prone in reverse Trendelenburg position with neck in slight flexion under general anaesthesia. Surface marking was done under fluoroscopy and the target point is defined as “V” point which is lateral confluence of cranial and caudal lamina of a corresponding level. An 8-mm incision was made and obturator was introduced followed by bevel working cannula. The procedure Was performed using an endoscope with 30° optical angle, 7.3-mm outer diameter, and working channel 4.7-mm working channel (Joimax, GmbH, Karlshruhe, Germany).
1. Posterior Endoscopic Cervical ForaminotmyThe medial border of facet is identified and bony drilling started from the “V” point. The bony drilling was performed in a sequence from inferior border of cranial lamina to laminofacet junction followed by superior border of caudal lamina. It is performed with a 3.5-mm diamond tip high speed drill system (Primado, NSK, Nakanishi, Japan). The bony drilling continued until free margins of ligamentum flavum were seen. Ligamentum flavum resected with the help of endoscopic Kerrison punch. Epidural bleeding controlled with a radiofrequency probe. It is also used to palpate the location and extent of pedicle of caudal vertebra.
2. Posterior Endoscopic Cervical PediculectomyAfter completion of foraminotomy the working channel is rotated in caudal direction to locate the pedicle of caudal vertebra. It is usually present in the axilla of exiting nerve root. The pedicle is circumferentially drilled up to posterior border of vertebra. Thin remnant shell of pedicle along with osteophytes were removed with bone cutter. The final C6 root to C7 root decompression is checked by observing capillary perfusion along the roots (Supplementary video clip 1).
Patient’s pain improved to VAS score of 3 for neck and 1 for arm. Neck range of movements and neurology was improved completely during follow-up visits. post operative CT scan and MRI showed complete decompression of right C5-6 and C6-7 foramen (Figure 2). One-year follow-up dynamic radiograph showed no exaggeration of spondylolisthesis or instability (Figure 3).
DISCUSSIONThe conventional anterior approach is considered as the gold-standard treatment for a degenerative cervical myeloradiculopathy [1]. Though the procedure is associated with the high success rate; approach related complications are well documented in the literature [2,3]. Sometimes, the anterior approach can become difficult in case of previous anterior cervical surgeries such as radical neck dissection, thyroidectomy or carotid angioplasty as in present case. It can be due to disturbed normal anatomy of the neck and postoperative fibrosis or adhesions. The full-endoscopic approach for the cervical spine has evolved over last few decades with excellent clinical results [6-8]. Though it has many advantages such as minimal tissue damage with preservation of cervical motion segment; its indication is restricted for a single level paracentral to foraminal disc herniations [9,10]. For the cervical central disc herniation motion various motion preserving approaches has been described in the literature. Nakai et al. [11] first described anterior transcorporal approach for difficult type of migrated disc herniation performed through small bony tunnel in the cervical vertebra. The ability of transcorporal approach to preserve the motion segment has inspired many spine surgeons to try this approach with various modifications [12,13]. The transcorporal approach was technically demanding as it requires exact location of the herniation and precise trajectory of the bone tunnel. Kim et al. [14] have described transpedicular approach for the difficult central type of disc herniation though posterior endoscopic approach. The controversy exists about the extent of medial facet joint which can be safely resected without causing postoperative instability or kyphosis. According to the study by Raynor et al. [15], 50% of medial facet can be resected during posterior cervical foraminotomy without causing postoperative instability. In present case, we have resected nearly 50% of right side C5–6, C6–7 facet joint along with total C6 pediclectomy. Present case will be the first to report total cervical pediculectomy for the adjacent-level cervical foraminal stenosis. The key point of the technique is to maintain the accurate trajectory between 2 vital structures that is Cervical cord medially and vertebral artery laterally [16,17]. Concentric drilling of the pedicle with 3.5-mm diamond burr prevents its unexpected advancement and injury to the vital structures. The procedure was continuously monitored under fluoroscopy to ensure depth and trajectory of the drilling. The nerve root can be retracted to some extent to approach ventral disc herniation or osteophytes. The adjacent levels of a cervical spine can be decompressed through the single approach. Though, the present technique is preserving the motion segment, overall sagittal alignment cannot be improved with the technique. The technique is lengthy and has long learning curve; hence should be reserved for the selected cases (Figure 4).
CONCLUSIONThe pediculectomy approach is relative safe and efficient technique for the adjacent-level cervical foraminal stenosis. The neural decompression under direct endoscopic vision with less damage to the motion segment can result in better clinical results. The procedure has a learning curve and to be considered based on the pathology.
ACKNOWLEDGEMENTSWe confirm that all the figures included in the manuscript are our own figures, developed with the help of Medart.
Figure 1.Preoperative imaging. (A) Plain radiograph (anteroposterior view) showing a carotid angioplasty stent on the right side. (B, C) Dynamic radiograph showing multiple cervical degenerative disc disease without instability. Computed tomography (sagittal [D], coronal [E], and axial cuts [F]) showing right C5–6 and C6–7 foraminal stenosis (orange arrow). Magnetic resonance imaging (sagittal [G] and axial cuts [H]) showing right C5–6 and C6–7 foraminal stenosis 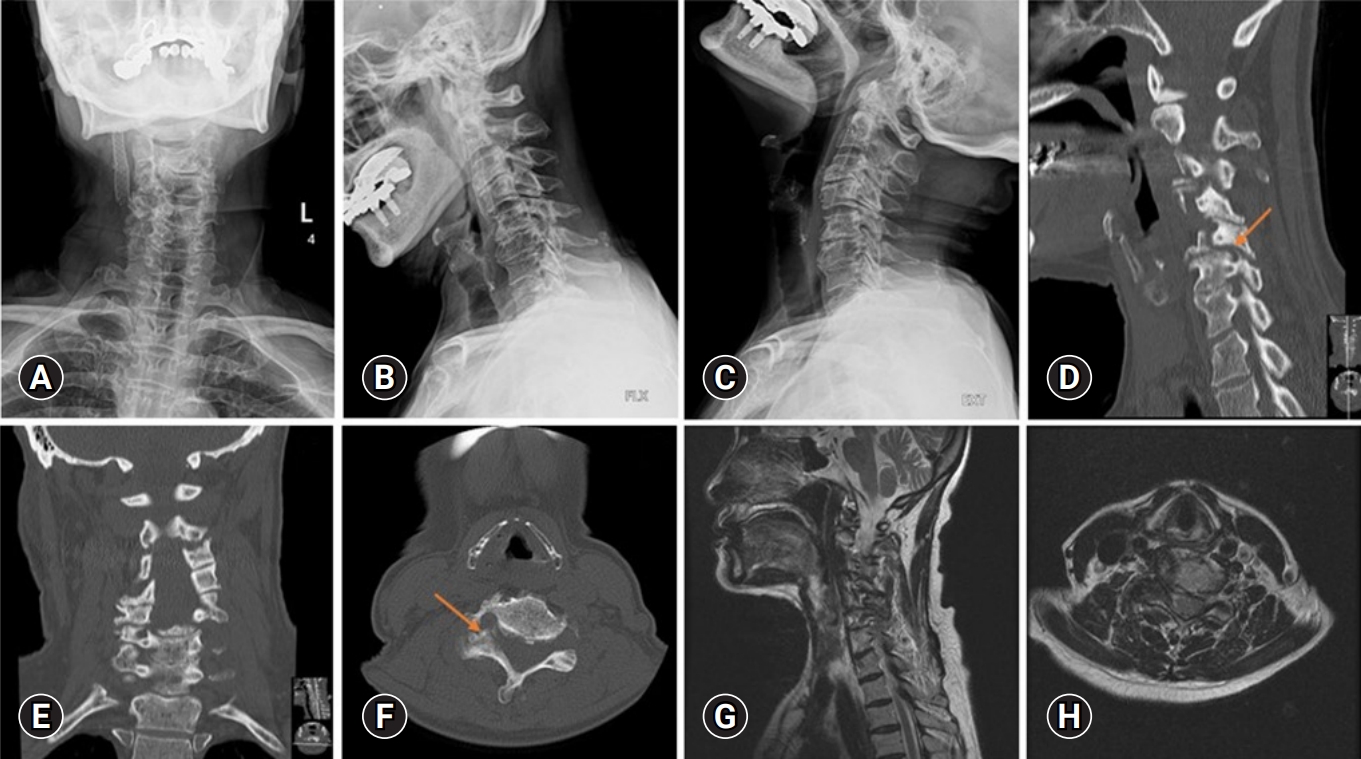
Figure 2.Postoperative imaging. (A, B) Radiograph and 3-dimensional computed tomography (CT) scan showing foraminotomy with the pediculectomy site (blue arrow). CT scan (sagittal [C] and axial cuts [D]) showing right C5–6 and C6–7 foraminal decompression (orange arrow). Magnetic resonance imaging (sagittal [E] and axial cuts [F]) showing right C5–6 and C6–7 foraminal decompression 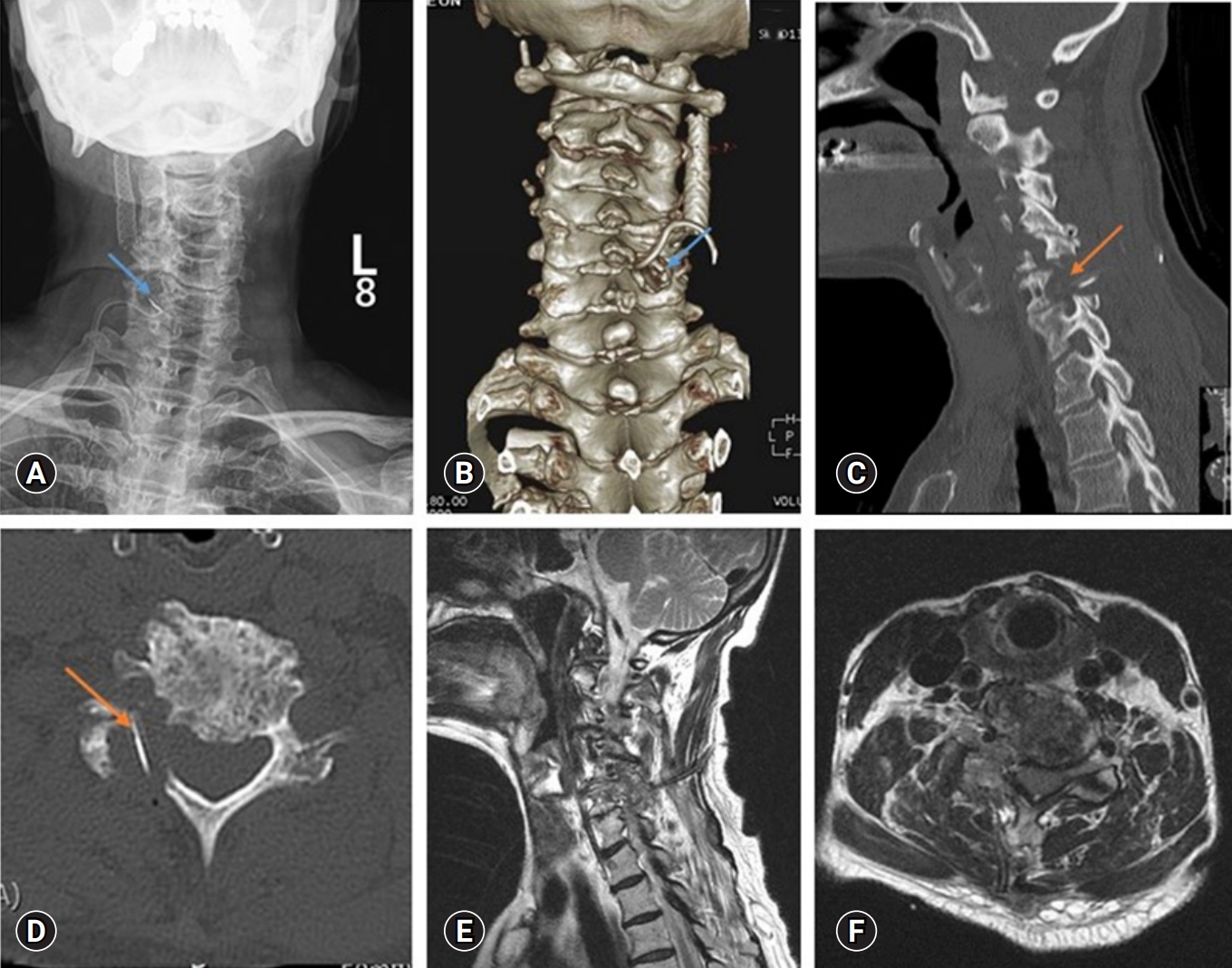
REFERENCES1. Cloward RB. The treatment of ruptured lumbar intervertebral discs; criteria for spinal fusion. Am J Surg 1953;86:145–51.
2. Epstein NE. A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int 2019;10:100.
3. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310–7.
4. Oezdemir S, Komp M, Hahn P, Ruetten S. Decompression for cervical disc herniation using the full-endoscopic anterior technique. Oper Orthop Traumatol 2019;31(Suppl 1):1–10.
5. Komp M, Oezdemir S, Hahn P, Ruetten S. Full-endoscopic posterior foraminotomy surgery for cervical disc herniations. Oper Orthop Traumatol 2018;30:13–24.
6. Selvanathan SK, Beagrie C, Thomson S, Corns R, Deniz K, Derham C, et al. Anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of brachialgia: the Leeds spinal unit experience (2008-2013). Acta Neurochir (Wien) 2015;157:1595–600.
7. Lee DG, Park CK, Lee DC. Clinical and radiological results of posterior cervical foraminotomy at two or three levels: a 3-year follow-up. Acta Neurochir (Wien) 2017;159:2369–77.
8. Kim M, Kim HS, Oh SW, Adsul NM, Singh R, Kashlan ON, et al. Evolution of spinal endoscopic surgery. Neurospine 2019;16:6–14.
9. Zhang C, Wu J, Zheng W, Li C, Zhou Y. Posterior endoscopic cervical decompression: review and technical note. Neurospine 2020;17(Suppl 1):S74–80.
10. Wu PH, Kim HS, Lee YJ, Kim DH, Lee JH, Yang KH, et al. Posterior endoscopic cervical foramiotomy and discectomy: clinical and radiological computer tomography evaluation on the bony effect of decompression with 2 years follow-up. Eur Spine J 2021;30:534–46.
11. Nakai S, Yoshizawa H, Kobayashi S, Hayakawa K. Anterior transvertebral herniotomy for cervical disk herniation. J Spinal Disord 2000;13:16–21.
12. Choi G, Lee SH, Bhanot A, Chae YS, Jung B, Lee S. Modified transcorporeal anterior cervical microforaminotomy for cervical radiculopathy: a technical note and early results. Eur Spine J 2007;16:1387–93.
13. Kim JS, Eun SS, Prada N, Choi G, Lee SH. Modified transcorporeal anterior cervical microforaminotomy assisted by O-arm-based navigation: a technical case report. Eur Spine J 2011;20 Suppl 2(Suppl 2):S147–52.
14. Kim HS, Wu PH, Lee YJ, Kim DH, Kim JY, Lee JH, et al. Safe route for cervical approach: partial pediculotomy, partial vertebrotomy approach for posterior endoscopic cervical foraminotomy and discectomy. World Neurosurg 2020;140:e273–82.
15. Raynor RB, Pugh J, Shapiro I. Cervical facetectomy and its effect on spine strength. J Neurosurg 1985;63:278–82.
|
|
|||||||||||||||||||||||||||||||||||||||||