AbstractObjectiveThe atlantoaxial complex exhibits unique morphological and biomechanical characteristics. Trauma, tumors, and inflammatory or congenital diseases may compromise the stability of this joint. The purpose of this study was to describe a minimally invasive surgical (MIS) technique for C1-C2 fixation through an anatomical corridor and to analyze the clinical, surgical, and fusion outcomes using this approach over a 15-year period.
MethodsWe present a MIS technique utilizing a natural anatomical corridor for C1-C2 screw fixation, which has been used at our institution since 2007. We analyzed the demographic characteristics and clinical results of the patients who underwent this procedure.
ResultsForty-seven patients underwent C1-C2 MIS screw fixation during the study period, with 24 male patients and a median age of 66 years. The indication for surgery was atlantoaxial subluxation in 60% of cases and odontoid fracture in 23%. The median surgery duration was 130 minutes, with a median blood loss of 300 mL. There were no intraoperative complications, and only one patient presented with a superficial wound infection, which was successfully treated with antibiotics.
Conclusion The minimally invasive approach through a natural anatomical corridor to fuse the atlantoaxial joint using C1 lateral masses and C2 pedicle screws bilaterally has been demonstrated to be safe and effective. Preserving the occipital-cervical tension band provides additional biomechanical stability to the construct.
INTRODUCTIONThe atlantoaxial segment is a complex junction with unique morphological and biomechanical features, which play a critical role in the stability of the upper cervical spine. More than half of the head's rotational movement is attributed to this joint [1]. When affected by trauma, tumors, inflammatory or congenital diseases, the stability of this joint may be compromised, leading to potential neurological consequences. Over the years, various posterior fixation techniques have been developed to stabilize the first and second vertebrae of the upper cervical spine [2,3]. Fixation techniques using C2 pedicle screws and C1 lateral mass screws with plates or rods on each side, or trans articular C1-C2 screw fixation, have shown high fusion rates [4-7].
Percutaneous screw fixation using imaging navigation is a minimally invasive surgical technique for the posterior cervical spine, but its application may be limited due to the availability of navigation technology, especially in low- and middle-income countries. To address this issue, since 2007, we have developed a minimally invasive trans-muscular approach for the placement of C2 pedicle screws and C1 lateral mass screws in patients with craniocervical junction pathologies, with promising outcomes [8,9]. This technique provides a safe and effective alternative for patients who require surgical intervention for atlantoaxial instability.
To preserve the occipital-cervical tension band, we have described a minimally invasive surgical technique for C1-C2 screw fixation using a natural anatomical corridor found 2 cm away from the midline and parallel to C2 spinous process, as shown in Figure 1A. This corridor is created by the angle between the posterior major rectus capitis and obliquus capitis inferior muscles and is usually free of vascular and nervous structures until reaching the atlantoaxial joint, where a venous plexus is encountered. The bleeding can be easily controlled with bipolar coagulation and absorbable hemostatic agents. In our microsurgical laboratory, we conducted anatomical dissection studies to identify this corridor and its relationship with the vertebral artery for the screw insertion point as shown in Figure 1B [9-11].
The aim of this study is to describe the use of this minimally invasive surgical technique for C1-C2 screw fixation through the anatomical corridor and analyze the clinical, surgical, and fusion results obtained in a 15-year period. This approach has shown to be safe and effective for patients with craniocervical junction pathologies and can provide an alternative to more invasive surgical techniques while preserving the occipital-cervical tension band.
MATERIALS AND METHODS1. Study PopulationThe study was conducted at Hospital Universitario San Ignacio in Bogotá, Colombia, and utilized the hospital’s Neurosurgery Department databases to collect all data. Medical information from patients who underwent MIS C1-C2 screw fixation between December 2007 and December 2022 was retrospectively evaluated after receiving approval from the institutional review board. All MIS treatments were performed by two spine surgeons with experience in a variety of MIS spinal procedures.
2. Data CollectionBaseline patient data, including age, sex, and prior medical histories, were obtained. Operative notes were reviewed to gather information about the type of surgery, the level of pain prior to and after surgery as measured by the visual analog scale, the duration of the surgery, and intraoperative hemorrhage volume. Postoperative information, such as the length of hospital stay, clinical assessments, and postoperative x-rays and tomography, were collected to evaluate fusion.
INDICATIONSThis surgical technique is most beneficial for patients with C1/C2 instability resulting from inflammatory and degenerative atlantoaxial subluxation, traumatic C1/C2 instability (especially C2 dens fractures and transverse ligament disruption), and basilar invagination associated with fixed atlantoaxial dislocation [2,3]. For cases with significant destruction of the lateral masses of C1 and/or C2 pedicles, requirement of instrumentation and/or decompression of the subaxial cervical spine, a high-riding vertebral artery that obstructs C2 pedicle insertion point or screw trajectory, or presence of ponticulus posticus, alternate posterior fixation techniques are recommended [4-7].
1. Preoperatory PreparationPrior to surgery, a comprehensive medical history and physical examination are conducted. Preoperative laboratory testing and risk assessment are routine procedures. It is crucial that the patient and their family fully comprehend the objectives of the surgical intervention. A spine panoramic x-ray is essential to evaluate global sagittal balance and cervical sagittal balance. Pre-operative cervical tomography is also necessary to assess osseous structures and vascular relationships, such as the presence of ponticulus posticus, high-riding vertebral artery, and vertebral artery location in relation to C1 and C2.
2. Anesthesia and Patient PositionAfter the induction of general anesthesia, the patient was positioned in a prone position on a standard radiolucent table over spinopelvic rolls to reduce intraabdominal pressure and protect skin pressure zones. Continuous intraoperative neurophysiological monitoring was recorded throughout the procedure to ensure neural integrity. The head was fixed in a neutral position and secured in a Mayfield clamp (Integra, LifeSciences, Cincinnati, Ohio, United States) to preserve cervical sagittal alignment and the horizontal gaze plane (Figure 2A).
1) Skin Marking and Skin IncisionParamedian vertical posterior skin marks measuring 25 mm were made (Figure 2B) after identifying the C1 lateral masses and C2 pedicles with intraoperative x-ray. A 10-blade was used to make the skin incision, and monopolar cautery was utilized to dissect the fat tissue and aponeurosis.
2) Insertion of Minimally Invasive SystemA tubular dilator system platform, microMaXcess® (NuVasive Inc., San Diego, CA, USA), was inserted through the superficial nuchal musculature to access the anatomical corridor between the obliquus capitis inferior and the posterior major rectus capitis muscles (Figure 2C). The proper positioning of the tubular dilator system was verified with intraoperative x-ray in anterior-posterior and lateral projections.
SURGICAL PROCEDUREA microMaXcess® MIS tubular dilator system platform (NuVasive Inc., San Diego, CA, USA) was used to perform paramedian vertical posterior skin marks of 25 mm (Figure 2B). Prior to this, the C1 lateral masses and C2 pedicles were identified using intraoperative x-ray. The skin incision was made with a 10-blade, and fat tissue and aponeurosis were dissected with monopolar cautery. The tubular dilator system was then placed through the superficial nuchal musculature to access the anatomical corridor between the obliquus capitis inferior and the posterior major rectus capitis muscles (Figure 2C). Proper positioning of the system was verified with intraoperative x-ray.
A three-valve spreader microMaXcess® with optical fiber light was placed to provide good exposure to the working area. With fluoroscopic guidance, the system was fixed at the entry point of the C2 pedicle without impeding the C1 posterior arch. Adequate positioning of the retractor was verified with anterior-posterior and lateral fluoroscopy. Subperiosteal dissection of the C2 bony surface was performed using monopolar cautery from medial to lateral to expose and fully visualize the lateral border of the C1-C2 joint. During dissection, the epidural venous plexus, which is prone to profuse bleeding, was identified and controlled with bipolar coagulation and standard hemostatic agents. The C2 root was identified, coagulated, and sacrificed to allow screw insertion. The Harms technique was used to for screw insertion with AP and lateral fluoroscopy guidance. Polyaxial screws with a diameter of 3.5 or 4.0 mm were inserted in the C1 lateral mass and C2 pedicles (Figure 2D, E). Figure 3 illustrates the relationship between the screw entry point and vertebral artery trajectory. The articular surface of the C1 and C2 joint was decorticated with micro-curettes to place demineralized bone matrix (Grafton® DBM-Putty, Osteotech®, Inc. New Jersey, USA) within the joint to promote fusion (Figure 2F). The same procedure was performed stepwise on the contralateral side. Finally, a standard layered closure was performed using absorbable sutures for muscle and subcutaneous tissue and nylon thread for the skin.
RESULTSForty-seven patients underwent C1-C2 minimally invasive screw fixation surgery during the study period (December 2007–December 2022), using the previously described surgical technique. Of these patients, 24 were male, and the median age was 66 years, ranging from 14 to 88 years old. All patients reported neck pain, with paresthesia being the second most commonly reported symptom (83%). Lower cranial nerve dysfunction was found in only 6 patients. The indication for surgery was atlantoaxial subluxation in 60% of cases and odontoid fracture in 23%. Table 1 summarizes the demographic characteristics of the patients included in the study. Rheumatoid arthritis was the most frequent comorbidity, and most atlantoaxial subluxations were secondary to RA compromise, with 32% of cases being secondary to fractures associated with trauma. Examples of atlantoaxial subluxation and odontoid fracture correction are shown in Figure 4 and 5.
The visual analog scale (VAS) was utilized to evaluate the preoperative pain perception at 30 minutes prior to surgery and three months postoperatively. The median VAS score was 8 before surgery, which improved to 4 at 3 months after surgery.
The mean duration of surgery was 130 minutes, with a mean blood loss of 300 mL (Table 2). Most of the bleeding originated from the venous plexus at the end of the natural anatomical corridor, although it could be appropriately controlled with bipolar coagulation and Gelfoam® (Pfizer Inc., New York, USA). There were no intraoperative complications, and only one patient with uncontrolled diabetes and rheumatoid arthritis suffered a superficial wound infection that was successfully treated with antibiotics, without the need for surgical intervention. The mean follow-up was 4 years (range: 10 years), and osseous fusion of the atlantoaxial joint was achieved in 99% of the patients. No surgical reinterventions were required during the follow-up period.
DISCUSSIONCraniocervical diseases leading to atlantoaxial instability pose a surgical challenge. The initial surgical management of atlantoaxial instability was reported by Mixter and Osgood, who utilized a braided silk suture encircling the posterior arch of C1 beneath the spinous process of C2 [3]. Since then, various posterior fixation surgical procedures have been described to address this issue [1,2,4-6].
Dorsal wiring has demonstrated fusion rates of 89% to 93%, with complications being infrequently reported. Nonunion is a well-known complication of these techniques [3]. In 1987, Magerl and Seemann [6] first described transarticular atlantoaxial arthrodesis, which requires a midline dorsal incision to expose the posterior elements of C1-C3, with particular attention paid to the atlantoaxial facet joint [3]. Fusion rates in this technique range from 96% to 99% [3].
In 2001, Harms described a dorsal approach involving subperiosteal dissection from the occiput to C3 [3,5]. C1 lateral mass screws are inserted from an entry point located at the middle junction of the C1 posterior arch and the midpoint of the inferior aspect of the lateral mass [5]. Preoperative imaging determines the entry point for inserting pedicle screws in a convergent and cephalad orientation from 20º to 30º on the medial and cranial quadrant of the isthmus surface of C2 [3,5]. The reported osseous fusion rates range from 94% to 100%. Our study demonstrated osseous fusion of the atlantoaxial joint in 99% of the patients.
Vertebral artery injury is a major concern with C1 transarticular screw fixation, although its incidence has been reported to be less than 3% [12]. With the use of Harms’ method in our minimally invasive approach, all inserted screws were 3.5 to 4.0 mm in diameter, and no vascular injuries occurred. The natural anatomical corridor formed by the posterior major capitis and the obliquus capitis inferior muscles allows for adequate screw insertion angulation at a safe distance from the vertebral artery. Accurate preoperative planning is crucial and should involve important aspects of the patient's vascular and osseous anatomy, such as V3 (third segment of vertebral artery) and C1 posterior arch relation, ponticulus posticus, spina bifida, among others. We also consider it important to insert the C1-C2 screws under direct vision and confirm the final position with x-rays.
The incidence of surgical site infection in posterior cervical surgery has been reported to be between 3% to 10% [11-14]. Diabetes has been identified as an independent factor increasing postoperative complications in cervical spine surgery [15]. We found a 2.1% incidence of surgical site infection with our approach. Only one postoperative complication occurred in a diabetic patient as a superficial wound infection 13 days after surgery. No surgical revision was necessary, and it was accurately controlled with antibiotics.
We observed an improvement in the perception of pain according to VAS at 3 months postoperative. However, due to the different pathologies and clinical presentations of patients before surgery, further studies are necessary to determine the statistical significance of these findings. During the postoperative follow-up, no progression of preexisting weakness was reported. Paresthesia was the symptom that persisted the most after surgery.
Minimally invasive techniques have reduced muscle atrophy, intraoperative blood loss, and improved postoperative pain control [16,17]. Our approach uses two small paramedian incisions (less than 3 cm) following a natural anatomical corridor that preserves the medial cervical tension band. This approach provides more biomechanical stability to the construct, reduces postoperative pain, and shortens the inpatient stay with an average hospitalization time of 34 hours since hospital arrival
Raut et al. [18] reported their 5-year experience with C1-C2 minimally invasive transarticular fixation, which showed a progressive reduction in operative time and blood loss over the evaluated period by exposing perioperative parameters in quartiles. The learning curve of our surgical technique has also demonstrated a tendency to reduce operative time, blood loss, and hospitalization over the last decade (Figure 6).
The limitations of this study should be highlighted, mainly because it is a retrospective study. It does not have a control cohort to compare the results, which limits the interpretation of the findings. However, during the period evaluated, a trend was observed in the improvement of clinical results with a good fusion rate. Further prospective studies comparing open C1-C2 stabilization with our minimally invasive technique could confirm the benefits of preserving the occipital-cervical tension band.
CONCLUSIONOur minimally invasive approach, which utilizes a natural anatomical corridor to fuse the atlantoaxial joint with C1 lateral masses and C2 pedicle screws bilaterally, has demonstrated safety and efficacy. We preserve the occipital-cervical tension band to avoid affecting the biomechanical stability of the construct. Based on our results and observed trends, surgical outcomes improve as the surgeon becomes more proficient in the surgical technique. Further prospective studies comparing open C1-C2 stabilization with our minimally invasive technique could confirm the benefits of preserving the occipital-cervical tension band.
NOTESEthical statements The ethical implications of this study center on the well-being and autonomy of the patients who underwent the minimally invasive surgical technique for C1-C2 fixation. It is important to note that the study received approval from the appropriate ethical review board before being conducted, which ensures that the research adhered to ethical standards and regulations. Additionally, the study obtained informed consent from all patients, which indicates that they were fully aware of the risks and benefits of the procedure and willingly agreed to participate. Fig. 1.(A) Muscle anatomy of the cranio-cervical junction; the trapezius and semispinalis capitis muscles were removed, and an anatomical corridor between the rectus capitis posterior major and obliquus capitis inferior muscles is shown. (B) Vertebral artery relationship 3 cm away from the midline while coursing to reach the C1 posterior arch. 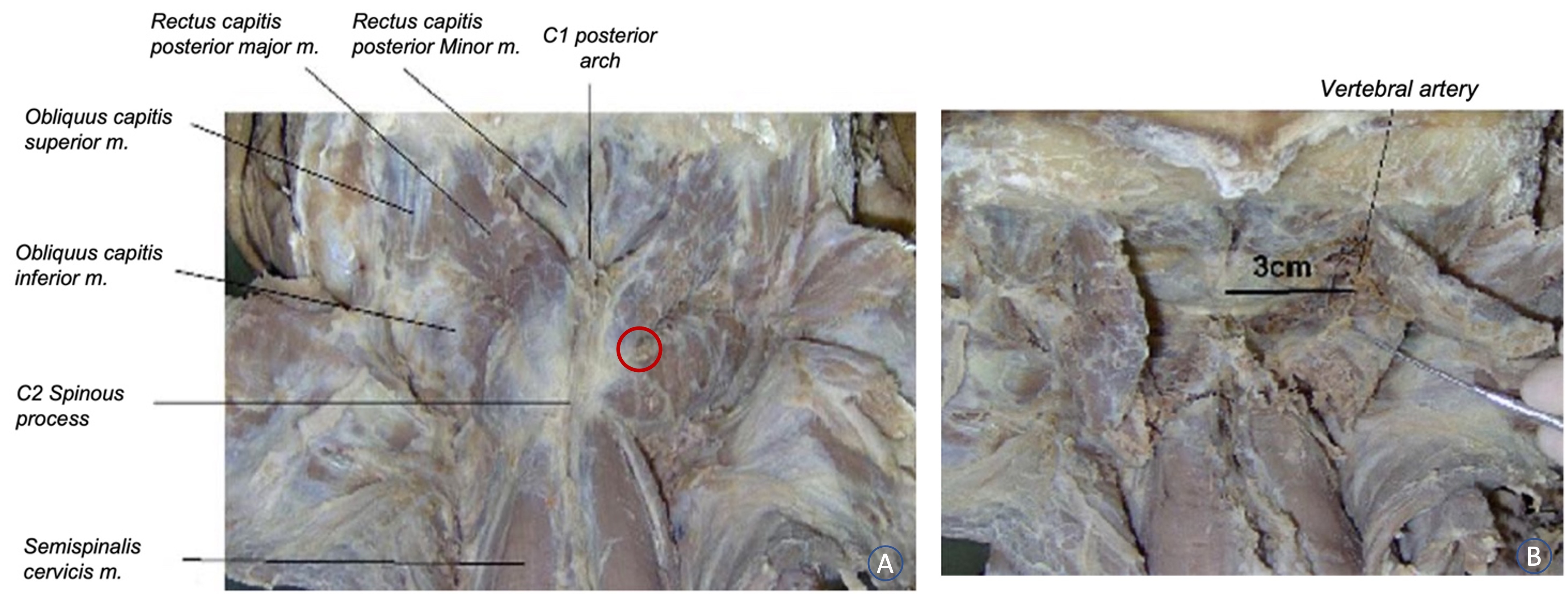
Fig. 2.(A) Patient prone with head fixed to a Mayfield clamp. (B) Two paramedian 30-mm skin mark incisions are made. (C) Intraoperative image of the minimally invasive retractor (microMaxcess II®; Nuvasive Inc., San Diego, CA, USA) placed through the anatomical corridor. (D) Intraoperative X-ray during the preparation of the C1 pedicle using the tap. (E) Intraoperative close-up image of the screws through the retractor. (F) Demineralized bone matrix placed within the joint to achieve a second fusion. 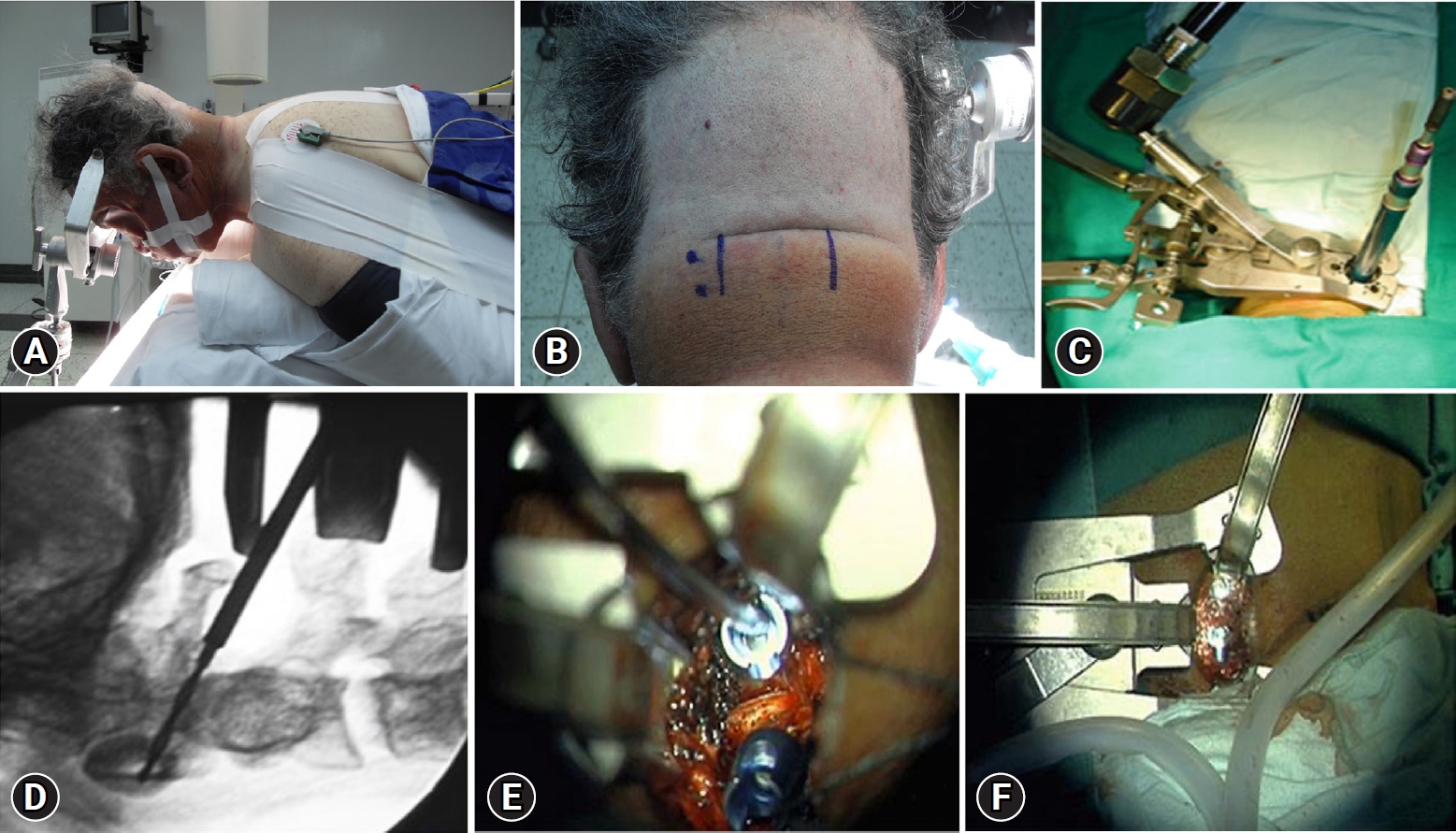
Fig. 3.(A) Entry point of screws using Harm’s technique (red points). (B) Relationship of the screws’ entry point and vertebral artery trajectory, showing a 1-cm distance between the vertebral artery and the screws’ entry point. 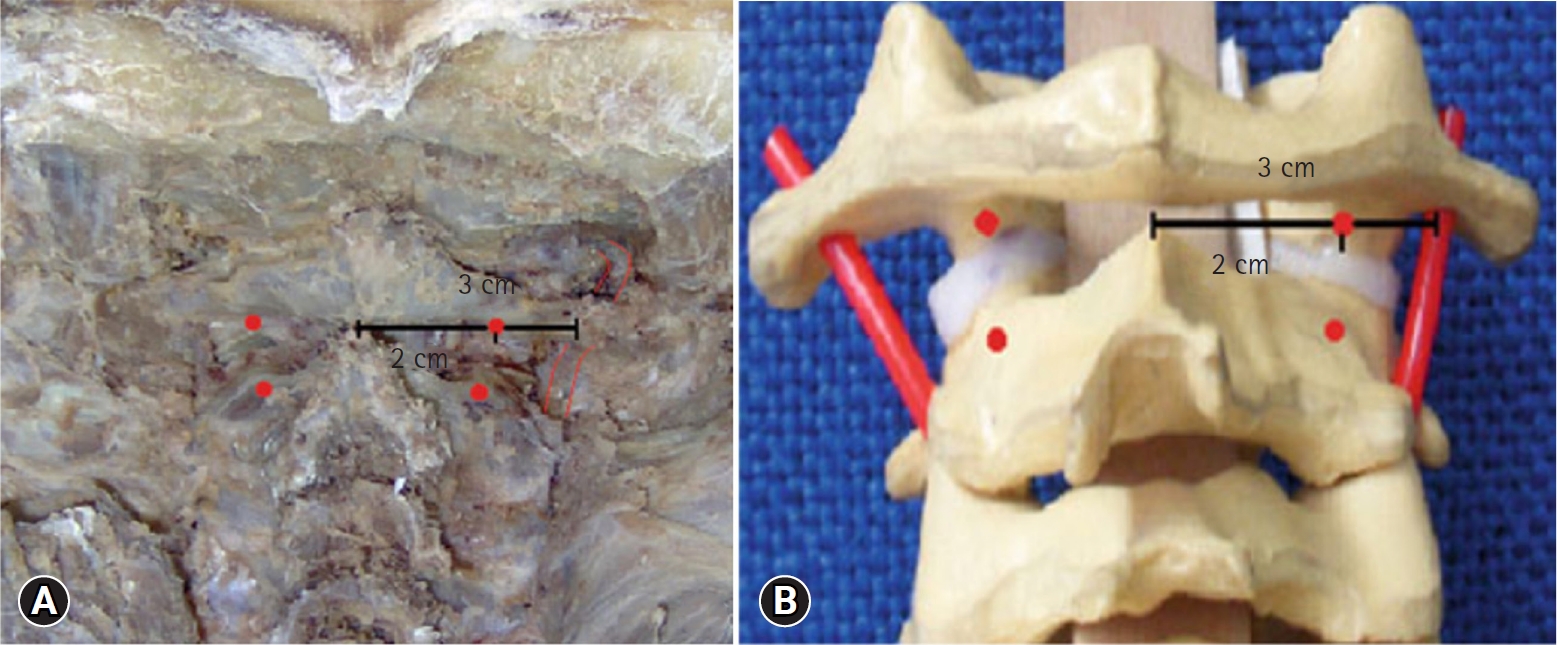
Fig. 4.(A) Lateral X-ray image of C1-C2 subluxation secondary to rheumatoid arthritis. (B) Intraoperative lateral X-ray image shows the implantation of screws at C1-C2 through the retractor. (C) Intraoperative lateral X-ray image of the final C1-C2 construct. 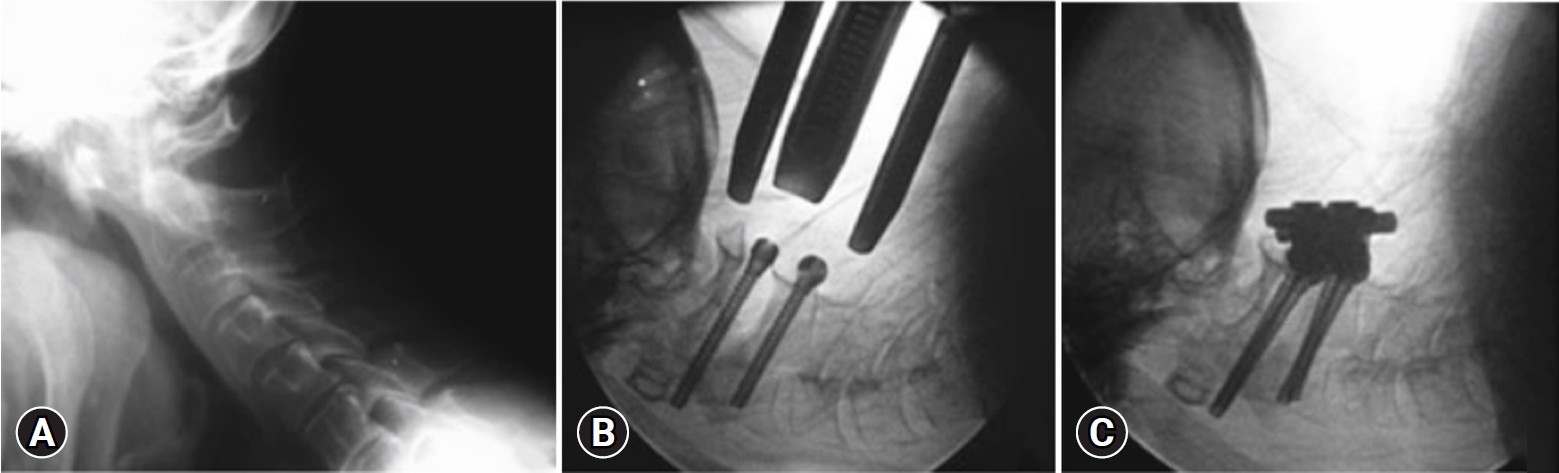
Fig. 5.(A): Preoperative cervical tomography showing type II dens fracture. (B) Postoperative anteroposterior X-ray view shows C1-C2 construction. (C) Postoperative lateral X-ray view of the construction. (D, E). Postoperative coronal and sagittal CT scan showing adequate trajectory and placement of screws. (F) Scar at the surgical incision site at 24 months of follow-up. CT: computed tomography. 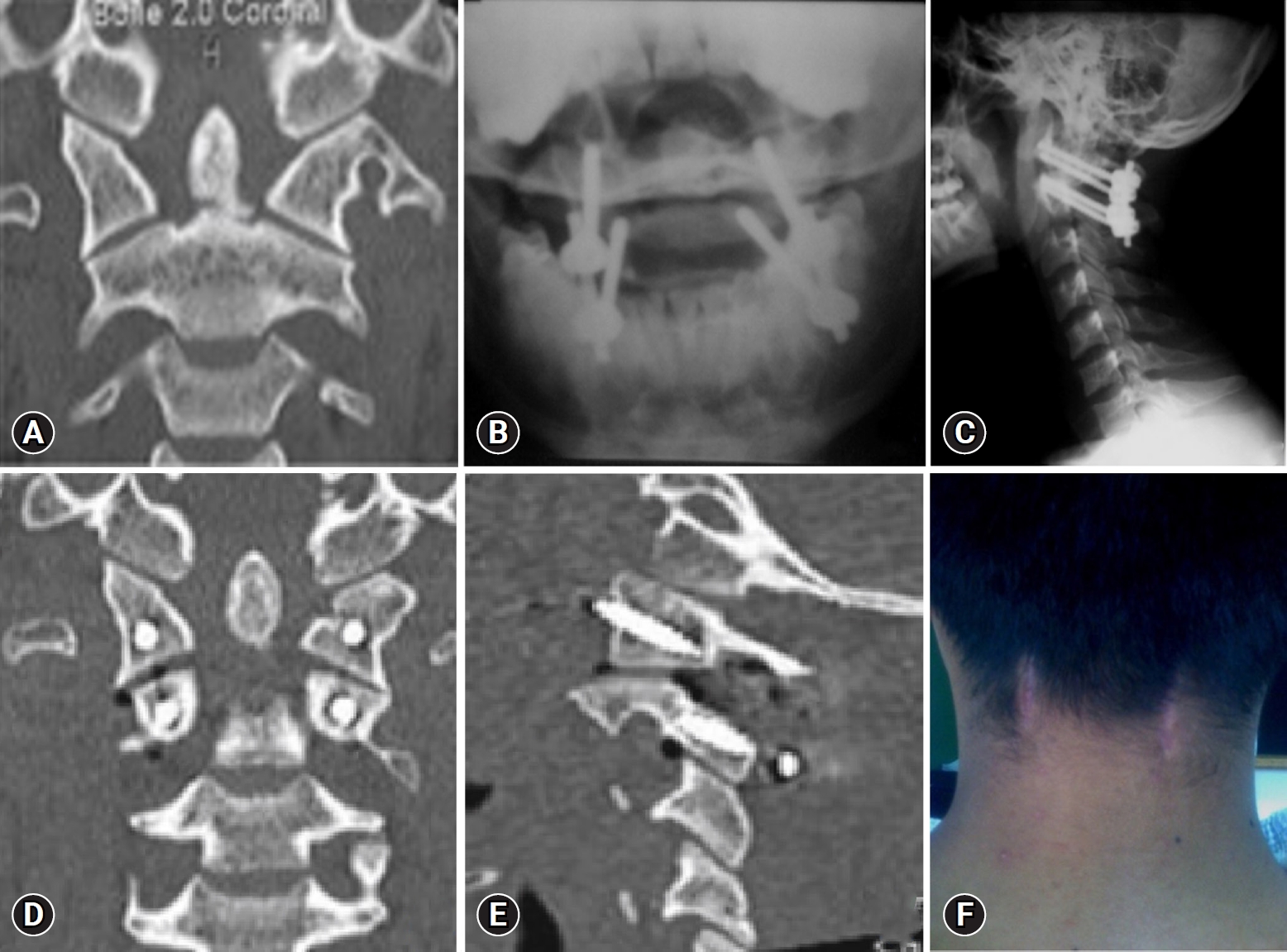
Fig. 6.(A) Average time of surgery (min) between 2012 and 2022. (B) Average blood loss in surgery between 2012 and 2022. (C) Average length of hospital stay (hr) between 2012 and 2022. 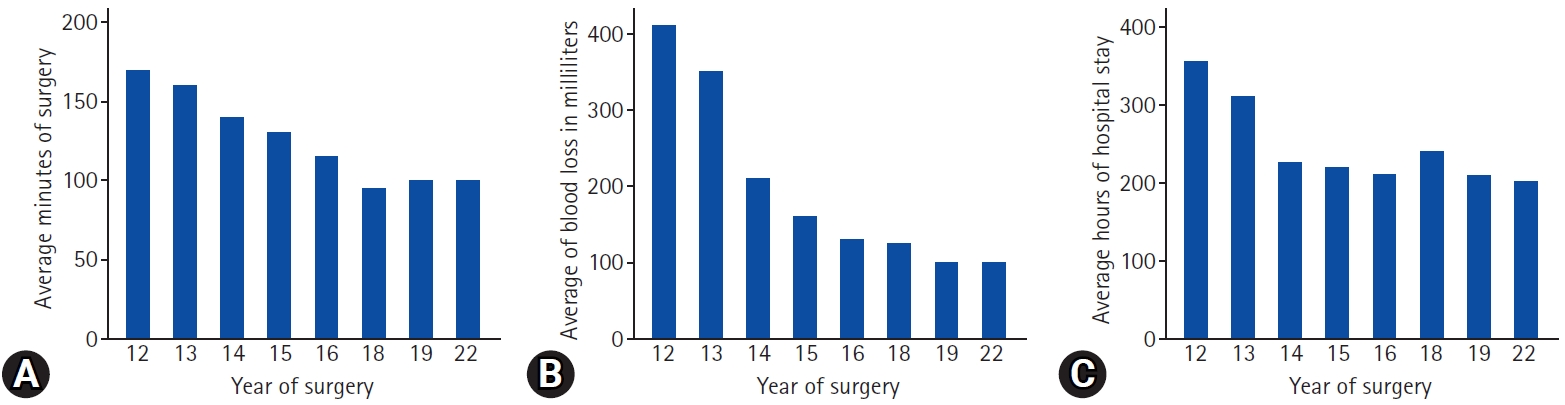
Table 1.Demographic characteristics REFERENCES1. Mimura M, Moriya H, Watanabe T, Takahashi K, Yamagata M, Tamaki T. Three-dimensional motion analysis of the cervical spine with special reference to the axial rotation. Spine (Phila Pa 1976) 1989;14:1135–1139.
2. Sim HB, Lee JW, Park JT, Mindea SA, Lim J, Park J. Biomechanical evaluations of various C1-C2 posterior fixation techniques. Spine (Phila Pa 1976) 2011;36:E401–E407.
3. Jacobson ME, Khan SN, An HS. C1-C2 posterior fixation: indications, technique, and results. Orthop Clin North Am 2012;43:11–18, vii.
4. Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery 2002;51:1351–1356.
5. Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26:2467–2471.
6. Magerl F, Seemann PS. Stable Posterior Fusion of the Atlas and Axis by Transarticular Screw Fixation. In: Kehr P, Weidner A, editors. Cervical Spine I. Vienna: Springer-Verlag; 1987. p. 322–327.
7. Rajinda P, Towiwat S, Chirappapha P. Comparison of outcomes after atlantoaxial fusion with C1 lateral mass-C2 pedicle screws and C1-C2 transarticular screws. Eur Spine J 2017;26:1064–1072.
8. Meyer M, Farah K, Graillon T, Dufour H, Blondel B, Fuentes S. Minimally invasive percutaneous C1-C2 fixation using an intraoperative three-dimensional imaging-based navigation system for management of odontoid fractures. World Neurosurg 2020;137:266–271.
9. Díaz R, Berbeo ME, Villalobos LM, Vergara MF, Osorio E. Minimally invasive posterior trans-muscular C1-C2 screw fixation through an anatomical corridor to preserve occipitocervical tension band: Surgical anatomy and clinical experience. Adv Tech Stand Neurosurg 2014;40:261–271.
10. Diaz R, Berbeo ME. Minimally Invasive Approach to Posterior Occiput to C2. In: Watkins RG, Watkins RG, editors. Surgical Approaches to the Spine 3rd ed. New York: Springer; 2015. p. 269–275.
11. Badiee RK, Chan AK, Rivera J, Molinaro A, Doherty BR, Riew KD, et al. Preoperative narcotic use, impaired ambulation status, and increased intraoperative blood loss are independent risk factors for complications following posterior cervical laminectomy and fusion surgery. Neurospine 2019;16:548–557.
12. Leckie S, Yoon ST, Isaacs R, Radcliff K, Fessler R, Haid R Jr, et al. Perioperative complications of cervical spine surgery: analysis of a prospectively gathered database through the association for collaborative spinal research. Global Spine J 2016;6:640–649.
13. Shamji MF, Cook C, Pietrobon R, Tackett S, Brown C, Isaacs RE. Impact of surgical approach on complications and resource utilization of cervical spine fusion: a nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J 2009;9:31–38.
14. Worley N, Buza J, Jalai CM, Poorman GW, Day LM, Vira S, et al. Diabetes as an independent predictor for extended length of hospital stay and increased adverse post-operative events in patients treated surgically for cervical spondylotic myelopathy. Int J Spine Surg 2017;11:10.
15. Elliott RE, Tanweer O, Boah A, Morsi A, Ma T, Frempong-Boadu A, et al. Atlantoaxial fusion with transarticular screws: meta-analysis and review of the literature. World Neurosurg 2013;80:627–641.
16. Lvov I, Grin A, Kordonskiy A, Sytnik A, Smirnov V, Khushnazarov U, et al. Minimally invasive posterior transarticular stand-alone screw instrumentation of C1-C2 using a transmuscular approach: description of technique, results and comparison with posterior midline exposure. World Neurosurg 2019;128:e796–e805.
|
|
|||||||||||||||||||||||||||||||||||||||