INTRODUCTION
Lumbar spinal stenosis is one of the most prevalent symptomatic spinal diseases in older patients, many of whom present with multilevel lumbar stenosis accompanied by disc herniation. Conservative treatment is not effective, causing many patients to require surgical treatment to relieve their symptoms [1-3].
Some authors favored decompression alone in multilevel lumbar stenosis. Orpen et al. [4] reported unilateral laminotomy for bilateral decompression (ULBD) can be applied to multilevel lumbar stenosis. Haba et al. [5] reported favorable outcomes after ULBD for multilevel lumbar stenosis. Son et al. [6] suggested decompression alone in elderly patients with two-level or more lumbar spinal stenosis without overt instability.
During surgical decompression for multilevel lumbar spinal stenosis, discectomy for disc herniation is taken into consideration. However, calcified disc is challenging to be removed because of severe adhesion between the nerve and the floor of the spinal canal. Excessive retraction is needed for ventral dissection, and dural tear or nerve root injury can be developed [7]. Resection of the protruded annulus fibrosus calcification can also increase the risk of recurrent disc herniation afterward. The vacuum disc in intervertebral space is the instability sign and related to the low back pain [8]. That is not clinical significance [9].
Here, successful cases for only surgical decompression for multiple stenosis with calcified disc protrusion and vacuum disc in the intervertebral space are presented, depicting favorable treatment outcomes and no perioperative complications.
CASE REPORT
1. Case 1
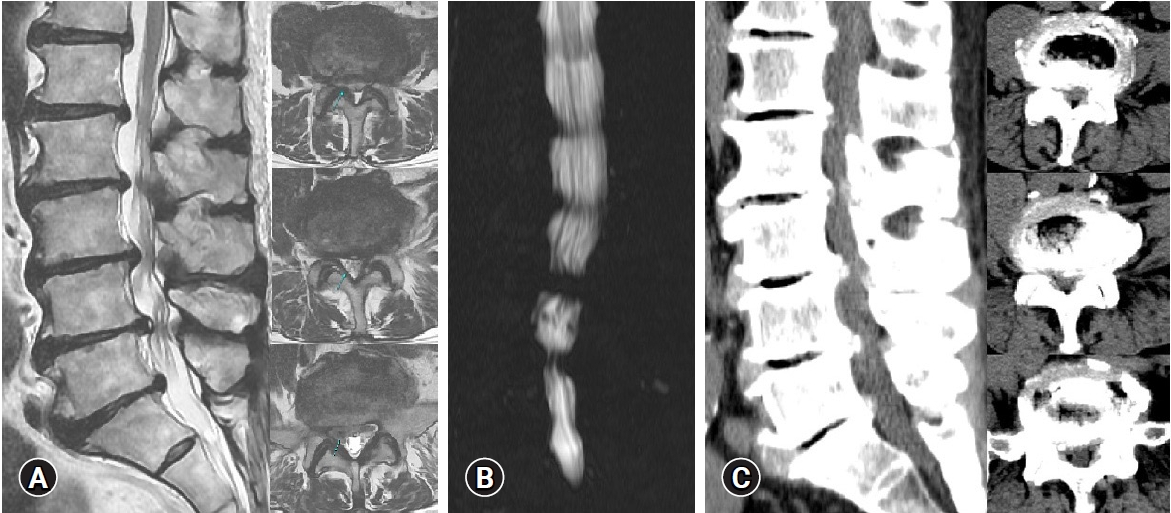
In May 2021, a 60-year-old man complained of severe low back pain and bilateral sciatica which began three months ago, and visited Daegu Wooridul Spine Hospital in Daegu, Korea. The sciatica followed a S1 dermatomal distribution. Several block procedures were performed in other hospitals; however, the symptoms prevailed. The patient’s pain score was assessed by the visual analog scale (VAS). Back VAS was 5, and Leg VAS was 8. He had difficulty walking due to sciatica. Preoperative MRI and CT demonstrated multilevel lumbar spinal stenosis with the protrusion of calcified discs and the vacuum disc in not the spinal canal but the intervertebral space, and preoperative myelogram showed a total signal block on L3-4, 4-5 level (Figure 1). Following a left hip and ankle fracture surgery in 1976, the patient developed motor weakness of the ankle and great toe, which scored Grade 4 on the manual muscle testing.
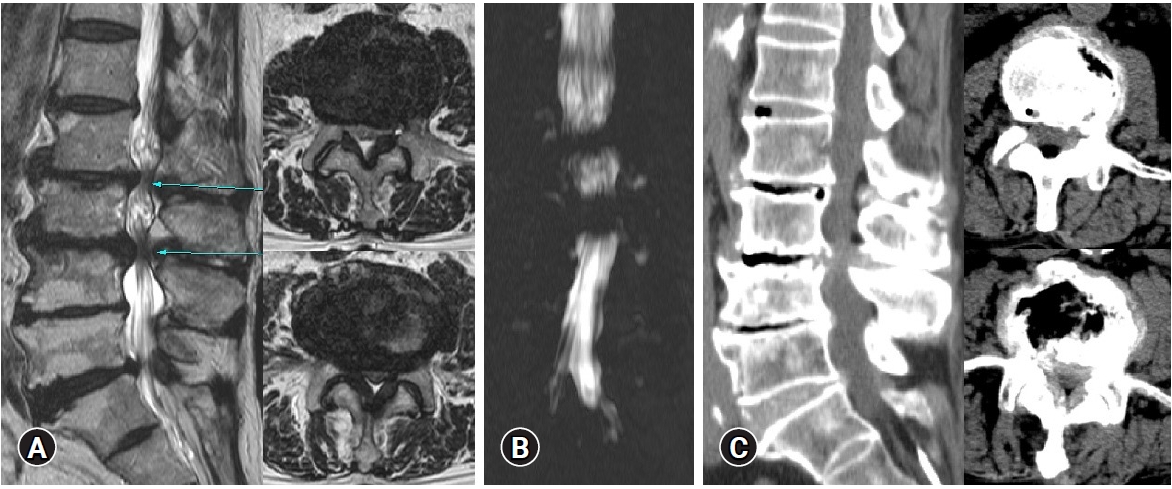
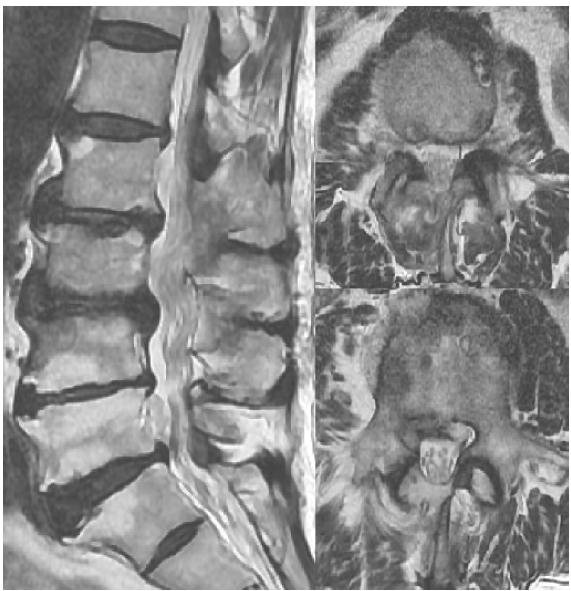
After informed consent was obtained from the patient, surgical decompression was performed. Under general anesthesia, the patient was placed in a prone position. A 90-mm long skin incision was made to target the L3-4, 4-5, 5-S1 disc space level. A Caspar retractor and Counter were inserted through the incision. After microscopic right ULBD on L3-4, 4-5 level, right laminectomy on L5-S1 level, and flavectomy on L3-4. 4-5, 5-S1 level without discectomy, the compressed thecal sac was released sufficiently and severe adhesion between the dura and the bottom of the spinal canal was observed. Ventral dissection was not tried. No injury of the dura and nerve root was reported. On postoperative MRI, the dural sac was released well (Figure 2). The operative time was about 160 minutes. Blood loss was 380 cc. The motor weakness of the ankle and great toe was not improved. However, the patient reported improved low back pain and bilateral sciatica with a reduction in VAS score for back and sciatica (Back VAS=3, Leg VAS=3), and dramatically improved walking ability compared with the preoperative state.
2. Case 2
In March 2021, a 77-year-old man presented with severe low back pain and bilateral sciatica which began two months ago. Several block procedures were conducted in other hospitals; however, the symptoms were not relieved. The pain was evaluated by Back and Leg VAS. Back VAS was 5, and Leg VAS was 8. He had ambulation difficulty due to sciatica. Multilevel lumbar spinal stenosis with the calcified disc protrusion accompanied by the vacuum disc in not the spinal canal but the intervertebral space was demonstrated on preoperative MRI and CT, and a complete block on L2-3, 3-4 level was shown on preoperative myelogram (Figure 3).
After informed consent was obtained from the patient, a right ULBD microscopic surgery without discectomy on L2-3, 3-4 level was applied under general anesthesia. After surgical decompression, the dural sac was released well and serious adhesion between the sac and the floor of the spinal canal appeared. Ventral dissection was not tried. No injury of the dura and nerve root was observed. The thecal sac was decompressed sufficiently on postoperative MRI (Figure 4). The operative time was about 120 minutes. Blood loss was 100 cc. Following the procedure, the patient reported dramatically improved ambulation compared to the preoperative state and improved low back pain and bilateral sciatica with a reduction in VAS score for back and sciatica (Back VAS=3, Leg VAS=3).
DISCUSSION
Lumbar spinal stenoses are often multilevel, but scarcely affect the whole lumbar spine, and can be accompanied by disc herniations, calcified discs, and vacuum discs. When deciding which level to be decompressed, magnetic resonance (MR) myelography using with MRI can be helpful in the exclusion and inclusion of the target levels [10]. In our study, two cases are multilevel lumbar stenosis accompanied by calcified disc protrusion and vacuum disc in the intervertebral space, not in the spinal canal.
Calcification of the disc or the presence of calcium pyrophosphate dehydrate and/or hydroxyapatite in the nucleus pulposus or annulus fibrosus is more common in the elderly population with chronic disc herniation [11,12]. When a chronic and degenerative lesion such as a calcified disc exists, severe adhesion between the dural sac and the bottom of the spinal canal, especially the ventral side of the dura and surrounding soft tissues, is usually observed. Ventral dissection is needed for excessive retraction, can induce complications, including injuries of the dura and nerve root. Discectomy is rarely performed in calcified disc protrusion. In the previous experience of calcified disc, ventral dissection was tried to check the floor of the spinal canal and injury of the ventral dura was developed. If severe dural adhesion is observed in the case of calcified disc protrusion, we will advise against ventral dissection.
A vacuum disc phenomenon on radiologic images frequently appears in lumbar degenerative disease and is regarded as the last stage of disc degeneration. The vacuum consists of about 90% nitrogen and small amounts of oxygen and carbon dioxide [13-15]. The vacuum in intervertebral space is the instability sign and related to the low back pain [8]. That is not clinical significance. However, dynamic foraminal or lateral recess stenosis is induced, or after annulus fibrosus tears, the gas accumulation occurs within spinal canal. Surgical treatment is needed [9,16].
The surgical methods for treating lumbar spinal stenosis are decompression with fusion and decompression alone. However, the choice of appropriated technique remains controversial. Ahmed et al. [17] and Saleh [18] concluded that decompression with fusion had better outcomes than decompression alone, in terms of Oswestry disability index (ODI), VAS, and the Japanese Orthopedic Association score. In contrast to their findings, Shen et al. [19] supported that there were no significant differences in clinical outcomes, considering ODI. Aihara et al. [20] reported that significantly shorter operation time and hospitalization, and significantly less blood loss were observed in the decompression group.
There are numerous factors in the selection between decompression with fusion and decompression alone, including instability, age, general condition, osteoporosis, the number of involved segments, and surgeon’s preference. Overt instability is the most important factor, because fusion is the treatment of choice. However, mild instability can be worrisome in the selection. Longer operation time and more blood loss can be attributed to perioperative morbidities in elderly patients or those with a poor general condition. Also, in patients with osteoporosis, instrument-related complications can be developed, such as cage subsidence, screw failure, and non-union. So, decompression alone can be a better choice for multiple lumbar stenosis in the elderly patients or those with a poor general condition or osteoporosis.
In our study, only surgical decompression was applied to cases of multilevel lumbar stenosis with calcified disc protrusion and vacuum disc in not the spinal canal but the intervertebral space. This method provided favorable treatment outcomes.