INTRODUCTION
Most of the osteoporotic vertebral fractures heal well with conservative management with rest and bracing [1]. However in some patients the fracture healing is impaired which leads to progressive vertebral collapse, fracture non union and spinal cord compression. These fractures if not treated aggressively will lead to significant neurologic deficit and non-ambulatory status [2-4]. Several mechanical factors come into consideration that eventually leads to impingement of neural structures causing devastating neurological compromise [5-7]. Identifying the risk factors for progression at presentation is important. The surgical options in these patients with neurological deficits include vertebral column resection (anterior/posterior) and stabilization. Charlson comorbidity index has shown these patients with advanced age are at risk of prolonged hospital stay and postoperative morbidity with an extensive surgical procedure [8]. Vertebroplasty has shown encouraging results in painful osteoporotic vertebral fractures but has limited role in patients with neurologic deficit.
The purpose of this study is to evaluate the instability signs of osteoporotic compression fractures with neurodeficit and quantify them as an instability score. We also evaluated the efficacy of minimally invasive stabilization and vertebroplasty in these patients.
MATERALS AND METHODS
Between January 2016 and December 2019, thirty patients with thoracolumbar osteoporotic fractures with neurodeficit who underwent minimally invasive percutaneous stabilization (MIPS) combined with percutaneous vertebroplasty (PVP) with or without localized midline decompression. Electronic medical records of these patients were evaluated after approval from the ethical committee (IRB No: KDA01276). Charlson comorbidity index was used to assess the medical risk for a more extensive surgery. All patients were evaluated by computed tomography (CT), magnetic resonance imaging (MRI) and plain radiographs to determine the morphology of the fracture.
1. Patient Demographics and Clinical Data (Table 1)
Clinical evaluation was done using VAS (visual analogue scale), and ASIA score done pre operatively, immediate post operatively, at 3 and 12 months. All patients were non ambulatory due to severe pain and neurologic impairment. They had bone mineral density (BMD) of more than 2.5 SD below the young adult mean (–2.5 SD or lower). Patients less than 65 years in age, patients with pathological fracture, osteomyelitis and patients with normal T score for BMD were excluded from the study.
2. Pre-operative Risk Factor Scoring
Extensive literature search was done to find out factors that predict worsening in osteoporotic fractures. Authors found seven important factors that need to be observed in these patients. All patients were evaluated before the surgery by plain radiographs, CT and MRI to determine the presence of these risk factors. A score of 1 was given for the presence of each of these parameters. After surgery the patients had serial radiographs to assess alignment, screw loosening and implant failure.
2) Vacuum Sign
The condition of affected vertebrae was evaluated for the intravertebral air or intervertebral fluid or both. Intraverterbal fluid was area of hypointensity on the T1 weighted images and hyperintensity on T2 weighted images on MRI. Intervertebral air was area of hypointensity on T1 and T2 weighted images [11-14].
4) Retropulsion/Spinal Canal Encroachment
Migration of the posterior vertebral elements into the spinal canal was categorized as retropulsion of the vertebral body [2,3,9]. Retropulsion further progressed to spinal canal encroachment. This was measured as ratio of the sagittal diameter of the bony fragments into the spinal canal to the sagittal diameter of the spinal canal at one level proximal to the fractured vertebrae. Greater than 25% was regarded as significant compression leading varying degree of neurologic deficits [3,6].
5) Posterior Ligament Injury
Involvement of the posterior interspinous ligaments at initial injury or gradual failure of the posterior ligaments with progressive kyphosis was regarded as tri column involvement. Injury to these structures can lead to progession of deformity [9]. Posterior ligamentous injury was assessed from CT as widening of spinous processes or on MRI from edema of the interspinous ligament.
6) Multiple Wedge Compression Fractures
More than one compression fractures was included as a risk factor. This results in increase in deformity with worsening neurology.
7) Anterior Vertebral Height Loss >50%
The anterior vertebral height of the fractured vertebrae was compared to the normal vertebrae above. This leads to worsening sagittal profile. The height restored after surgery was also measured [16].
The spinal instability was calculated by adding these seven radiographic parameters with a score of one given for presence of each risk sign. These patients had 3 or more risk factors seen radiologically at presentation. Hence authors of this study considered a score of 3 or more as an unstable for this group of patients. Total score was divided into two categories of stability: stable (0–2) and unstable (≥3) (Table 2).
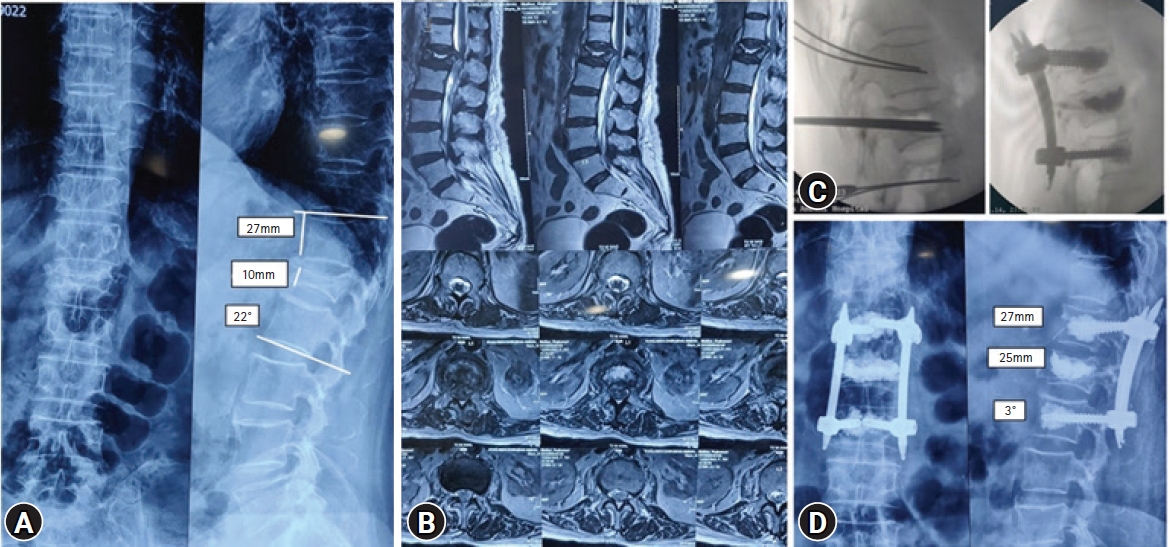
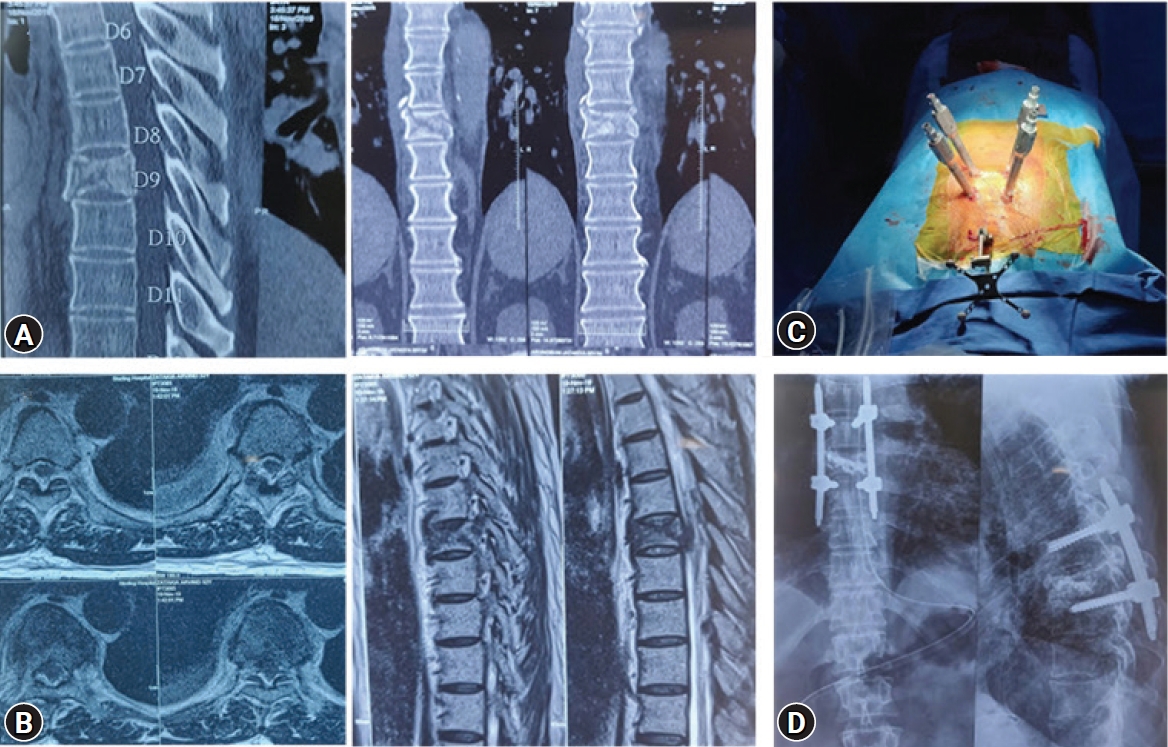
3. Surgical Technique (Figure 1)
Patient is postioned prone on bolsters. This leads to partial correction of kyphosis and restoration of anterior vertebral height. At first the pedicles of the affected segment were identified and skin was marked. The entry points for the percutaneous guide wires were made based on the C arm. Jamshedi needles were passed in to the pedicle after the position was confirmed on the image intensifier. Percutaneous screws were passed one level above and one level below the fracture over guide wire. In patients with higher angle of kyphosis screws were placed 2 levels above and below the fracture. In patients with severe osteoporosis they were augmented with bone cement. Two vertebroplasty needles were also passed in the fractured vertebra (Biportal Vertebroplasty). Position confirmed and about 4–6 mL of vertebroplasty cement was injected under fluoroscopy until cement reached the posterior 1/3rd of the vertebral body. Once the position of the cement was confirmed midline decompression was done at the level of retropulsion if necessary. In the current series midline decompression was done in 6 patients who retropulsion and canal encroachment of >50%. Midline incision was taken, paraspinal muscles retracted to expose the lamina. Partial laminectomy and decompression was done. When we stabilize and correct the kyphosis with rods the retropulsion decreases resulting in indirect decompression. The patients were mobilized on post-operative day one with braces in presence of physiotherapist.
4. Clinical and Radiological Evaluation (Table 3)
The clinical and radiological evaluation were done pre operative, immediate post operative, 3 months and 1 year after surgery. The severity of the neurologic deficits was assessed using ASIA (American spinal injury Association) impairment scale. The pain intensity was recorded using the visual analogue scale (VAS). Focal kyphosis, vertebral body height and hardware loosening or implant failure were assessed at follow up.
RESULTS
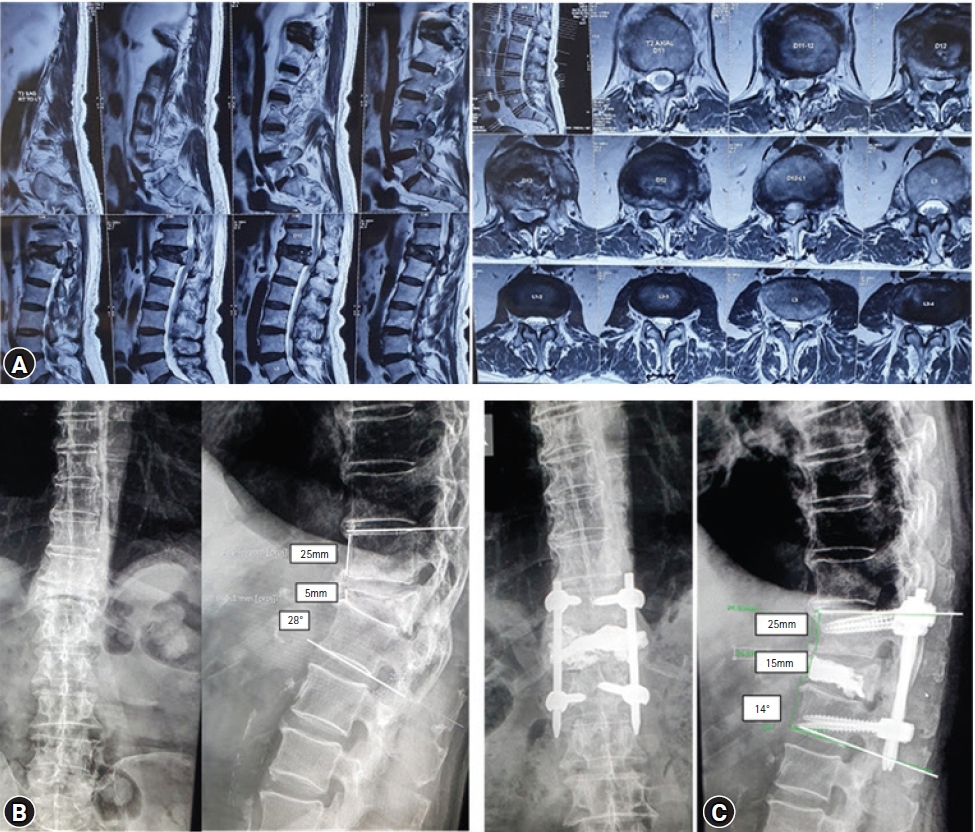
1. Clinical Outcome and Radiological Outcome (Figure 2, 3)
Electronic medical records of a total of 30 patients were evaluated clinically and radiologically. The most common level involved was D12 followed by L1. These patients had failed average conservative trial of 9 weeks (range, 8–14 weeks) before they presented to us with neurodeficit. There were 11 men and 19 women with a mean age of 71 years (range, 61–89 years). The average Charlson comorbidity index was 4 (range, 2–5). The average duration of surgery was 130 minutes (110–180 minutes) and the mean blood loss was 80 mL (range, 60–300 mL). Single level (one above and one below) minimally invasive stabilization was done in 26 patients while two levels (2 above and 2 below) were done in 4 patients with higher degree of kyphosis. In 6 patients cement augmented pedicle screws were used to augment the stabilization. The mean follow up was 28 months (range, 20–36 months) and the average hospital stay was 4 days (3–8 days). There was no perioperative complications, infection or death. The VAS significantly dropped from average pre-operative 9 (range, 7–10) to 2 (range, 1–4) immediately after surgery and 1 (range 0–1) at 1 year follow up (p<0.001). Burst fracture with middle column involvement was seen in 14 patients. Vacuum sign was seen in 26 patients. Retropulsion and more than 25% spinal canal encroachment was seen in 26 patients. The average local angle of kyphosis was 18° pre operatively (range, 12°–30°) which decreased to 6° post operatively (range, 0°–14°) (p<0.001). Single level vertebral collapse was seen in 25 patients, 3 patients had 2 level vertebral collapse and 2 patients has 3 level vertebral collapse. Injury to posterior spinal ligaments was seen in 14 patients. Nine patients had posterior ligament injury at the time of fall. Posterior column injury as a result of stretch injury to posterior ligamentous structures due to progressive increase in kyphosis was seen in 5 patients. Greater than 50% vertebral height loss was seen in 20 patients. The average pre operative anterior vertebral body height was 12 mm (range, 5–20 mm) which increased to average post operative anterior vertebral height of 20 mm (range, 12–27 mm) (p<0.001). In the current series, a varied neurological deficit at presentation was seen. Sixteen patients had ASIA D, 10 had ASIA C and 4 had ASIA B. Improvement in neurological status was observed in all these patients. At 3 months follow up 4 patients improved from ASIA B to ASIA D, 10 improved from ASIA C to ASIA E and 16 patients improved from ASIA D improved to ASIA E. There was loosing of hardware seen in 2 patients at 1 year follow up which required revision to longer instrumentation. The was some loss of correction at one year follow up with angle of kyphosis increasing from average 6° to 12° (range, 0°–16°)at one year follow up.
DISCUSSION
Osteoporotic vertebral fractures lead to debilitating pain necessitating prolonged bed rest and increase in morbidity and mortality [1,2]. From different studies in literature the risk factors leading to progression and neurologic impairment were evaluated. According to Denis [9] damage to all three columns has a greater risk of pseudoarthrosis and progression of vertebral collapse. It is important to identify middle column involvement at presentation in this group of patients. Fourteen patients had middle column involvement (incomplete burst fractures) in this series. Since they were incomplete burst without retropulsion they were initially treated conservatively. There is enough evidence to suggest that involvement of middle column and posterior wall of vertebral body increases the risk of non union and progression [3,7,10]. These patients need a close watch when conservative treatment is recommended. Intervertebral vacuum cleft represents a radiological sign of avascular necrosis of vertebral body will lead to pseudoarthrosis and further vertebral collapse [11-14]. This vacuum sign was present in 26 patients suggestive of spinal instability. Hoshino et al. [3] observed that severity of neurological deficit was related to angular instability of more than 15° and occupation of spinal canal with retropulsed fragments. In the current study the average preoperative angle of kyphosis was 18° which was corrected to 6° (p<0.001). Anterior vertebral height loss was measured as compared to above normal vertebrae. The AVH increased from a average preoperative value of 12 to 20 mm postoperatively (p<0.001). Correction of kyphosis and fairly good restoration of AVH resulted in indirect decompression and vertebroplasty lead to anterior column support. Baba et al. [2] concluded that the dynamic instability with hyper mobility at fractured level leads to gradual retropulsion of bony fragment into spinal canal which causes neurological impairment. Retropulsion of posterior vertebral elements was seen in 26 patients. Progression of retropulsion leads to spinal canal encroachment [3,6,9]. Greater than 25% spinal canal encroachment was seen in 20 patients in the current series. If the canal encroachment was between 25% to 50% authors of this study recommend only MIPS with VP. If the canal encroachment was greater than 50% then midline decompression was necessary. Bilateral decompression with unilateral laminotomy can preserve the midline structures however in these patients authors felt that midline approach would achieve a better decompression. We also evaluated whether there was a involvement of posterior elements and for multiple level wedge compression fractures [5,6,9,15]. Fourteen patients had posterior ligament injury in this study. Nine patients had posterior ligament injury at presentation as seen on MRI (edema of interspinous ligaments) or CT (widening of interspinous distance). Posterior column injury as a result of stretch injury to posterior ligamentous structures due to progressive increase in kyphosis was seen in other five patients. It is important for clinician to watch for posterior ligament injury in these patients at presentation and at follow up. This would also lead to progression of deformity and worsening of neurology. Multiple wedge compression fracture was another factor present in 4 patients. We observed that most of the instability factors are related to each other. Incomplete burst would result in retropulsion and non union and gradual increase in kyphosis. This progressed to stretch injury to posterior elements and multiple fractures. Hence it is necessary to break this cycle of risk factors progression. A score of 1 was given for the presence of each of these parameters. The spinal instability was calculated by adding these seven radiographic parameters. All of these patients had 3 or more risk factors seen on radiology at presentation. So we concluded that 3 or more score as an unstable score for these patients. Total score was divided into two categories of stability: stable (0–2) and unstable (≥3). The patients with instability score of 2 or less can be treated conservatively with medication and bracing. This scoring of instability can help surgeons to predict conservative treatment failure and need for surgical treatment.
As in case of traumatic vertebral fractures in young patients, where treatment is been well established, strategies are unclear for vertebral fractures in elderly population [5,6]. Patients in this study had failed conservative treatment with braces and medications or had gradually progressed despite appropriate precautions and treatment. These patients had a BMD of <2.5 SD along with osteoporotic fracture hence they were categorized as severe osteoporosis [17].These patients were non ambulatory due to severe pain and neurologic impairment. Sixteen patients were ASIA D, 10 patients ASIA C and 4 patients ASIA B at presentation. As most of these patients had significant canal encroachment, angular kyphosis, instability of middle and posterior column, the surgery of vertebral column resection and stabilization would be one option in treating these patients [1,18-20]. They also had 2 or more medical comorbidities like diabetes, history or stroke, myocardial infarction or dementia. The average Charlson comorbidity index was 4 suggesting that they were at risk of prolonged hospital stay and post operative morbidity if extensive anteroposterior decompression was attempted [8]. Considering the age, and morbidity of the procedure, we decided to treat them with a minimally invasive stabilization and anterior column support by vertebroplasty. In this study the fracture was reduced partially by placing the patient prone on bolsters and partially by proper distraction applied between 2 screws as necessary before vertebroplasty. Anterior column support was provided by vertebroplasty cement [1]. Hydroxyappatite vertebroplasty cement was used in all patients. In 6 patients, decompression was done using mini-midline incision however reconstruction of the anterior spine column with cage was not attempted. This surgery was tolerated well in this elderly population [16,20,21]. Single level stabilization was done when the kyphosis was less than 30° while 2 levels above and below stabilization was necessary in 4 patients with kyphosis greater than 30°. Two patients had loosing of the hardware at year follow up and needed revision to long segment stabilization. This could be a result of lack of fusion as no bone graft was used in anterior or posterior column. In the present study, VAS score improved significantly after surgery (p<0.001). Improvement in paraplegia was observed after surgery in all of these patients. Patients with ASIA B at presentation reached ASIA D at 1 year follow up and the rest reached ASIA scale E.
The study is not without limitations. The study has small sample size and is retrospective in nature. The entire scoring system was based on individuals who received a surgical intervention. A prospective study to see the natural progression of the osteoporotic fractures would answer these questions regarding the instability more effectively. It would be ideal to identify these risk factors at the onset and prevent the progression of instability. The scoring system needs to be validated. Through this study the authors wish to highlight the instability factors in osteoporotic vertebral fractures which can potentially risk progression and worsening of neurology.
CONCLUSION
The prediction of late neurologic deficit, progression of kyphotic deformity in vertebral compression fractures is difficult. Prolonged monitoring is necessary in vertebral compression fractures. Minimally invasive stabilization with or without local decompression and vertberoplasty is well tolerated in the elderly population with encouraging results. We concluded that patients with osteoporotic vertebral fractures who had 3 or more risk factors were at a risk of failure of conservative treatment. If the prognosis can be predicted on the early stage more aggressive and better treatment options can be considered to prevent neurological involvement.