INTRODUCTION
Minimally invasive techniques for spinal surgery have emerged as alternatives to the traditional open approach and are associated with a similar efficacy and shorter hospital stays [1]. These techniques are especially beneficial given their ability to prevent damage to the crucial supporting musculature of the spine and to consequently preserve its structural integrity [2]. Additional benefits include a smaller incision, a reduction in intraoperative blood loss, and a reduced need for analgesics when compared to open surgery [3]. However, all surgeries, whether open or minimally invasive, carry an inherent risk of complications.
Open cervical spinal surgery in particular is associated with a variety of complications. From an anterior approach, these include dysphagia after mobilization of the trachea and esophagus during surgical exposure, dysphonia due to nerve injury, and surgical site infections. In addition, retropharyngeal hematomas, esophageal injury, vascular injuries, and damage to the cervical sympathetic change also occur, but are less common [4]. More commonly a concern from a posterior approach, vertebral artery and cervical nerve root injuries can also occur [5,6].
Open thoracic spinal surgery is also traditionally associated with a variety of complications. From an anterior approach, injury to the great vessels is possible leading to hemorrhage as is damage to the thoracic duct leading to chylothorax [7]. Large exposures and lengthy surgeries often with the support of cardiothoracic surgeon can lead to significant post-operative pain, pneumothorax, pulmonary effusion, or pneumonia, all of which may further worsen the pulmonary status of a patient with impaired respiratory function [8]. From the posterior approach, misplaced pedicle screws may also damage the great vessels potentially leading to bleeding, thromboembolism, or pseudoaneurysm formation [9]. Spinal cord ischemia, nerve root injury, dural tear, and hematoma formation are also possible with both the anterior and posterior approaches [7].
Despite the known complications of open surgery involving the cervical and thoracic spine, complications associated with minimally invasive surgery (MIS) techniques remain unanswered. The present review seeks to identify potential complications associated with cervical and thoracic spine surgery using the tubular, endoscopic tubular assisted, uniportal endoscopic, and biportal endoscopic surgical approaches.
MATERIALS AND METHODS
1. Literature Search
Electronic searches were conducted using PubMed, Ovid Medline, and Cochrane Central Register of Controlled Trials (CCTR) from January 2012 until December 2022. In order to maximize the identification of relevant studies, searches were conducted by variably combining the terms: “biportal”, “microendoscopic”, “uniportal”, “cervical”, “thoracic”, “spine”, “surgery”, “complications”, and “minimally invasive” as either medical subject headings (MeSH) or keywords. Additionally, a search of the phrase “minimally-invasive cervical and thoracic spine surgery complications” was performed. The reference lists of all retrieved articles were further reviewed for any relevant studies. The titles and abstracts of the identified articles were then systematically assessed for any mention of minimally invasive tubular, endoscopic tubular-assisted, uniportal endoscopic, or biportal endoscopic surgery to the cervical or thoracic spine. The subsequent texts were then read in full for any mention of complications.
2. Selection Criteria and Data Extraction
Eligible studies for inclusion in the current review were those that included patients who underwent one of the four aforementioned MIS approaches for the treatment of a cervical and/or thoracic spine pathology with mention of complications. When institutions published studies with an overlapping patient population, the study with the larger patient cohort was selected. All publications were limited to those involving human subjects and written in the English language. Case-reports, cohort studies, and randomized control trials were included; abstracts, conference presentations, editorials, expert opinions, and review articles were excluded. All data related to complications following one of the four minimally invasive operative approaches was extracted from article texts and tables.
RESULTS
1. Literature Search
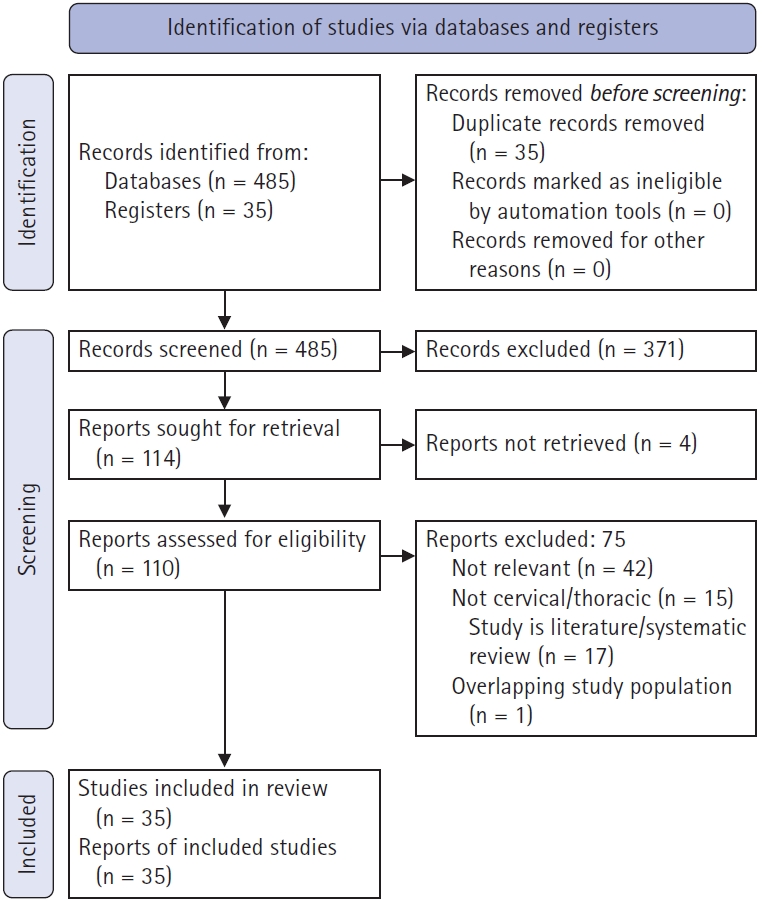
A total of 520 references were identified after an electronic database search through PubMed, Ovid Medline, and CCTR. After exclusion of duplicate references, the titles and abstracts of 485 potentially relevant articles were reviewed, and 371 were excluded based on relevance. Subsequently, 110 reports were retrieved for further analysis and 35 selected based on the aforementioned selection criteria. These 35 articles were thoroughly reviewed and complications were recorded. Of these articles, nine discussed complications from the tubular, six from the endoscopic tubular assisted, eleven from the uniportal, and thirteen from the biportal approaches. Of note, two articles discussed both the uniportal and biportal techniques, and one discussed uniportal, biportal, and tubular. This process is illustrated in Figure 1.
2. Microscopic Tubular Approach
Ross [10], in his retrospective cohort study, analyzed 302 consecutive cases for complications following the treatment of spondylotic diseases, epidural masses, or spinal cord stimulator implantations. These cases were complicated by one durotomy and two transient sensory deficits in the dermatomal distribution of the affected cervical nerve root. Additionally, of the 53 patients who underwent foraminotomy at the C5 level, three patients (5.7%) developed weakness at the corresponding nerve root level following the surgery. Two of these cases were transient, with patients regaining full function within three months, but one case was permanent. In another study of 45 patients treated for the surgical management of intradural-extramedullary spine tumors, 27 patients were treated with the tubular approach, resulting in three complications [11]. One patient developed a CSF leak, another wound dehiscence, and a third pneumonia (for a complication rate of 11.1%). Comparatively, of the 18 patients who underwent open surgical management in the same study, three patients developed a CSF leak and one a troponin elevation (for a complication rate of 22.2%).
Four additional studies, including one involving the surgical management of synovial cysts, two discussing tumors resections, and a fourth evaluating herniated discs were free of complications [12-15]. Balasubramanian et al. [16], studying a cohort of 25 patients undergoing tumor resection in the cervical or thoracic vertebrae, found two cases of post-surgical weakness. Additionally, Gandhi and German [17] reported one instance of wound dehiscence following resection of a meningioma, ventral to the C1 nerve roots. In a larger study of 118 patients who underwent either a microscopic tubular, uniportal, or biportal approach for the treatment of foraminal stenosis, the 50 patients in the tubular group experienced six complications including symptom recurrence (2), hematoma (2), dural tear (1), and a surgical revision (1) [18]. The studies discussing the microscopic tubular approach in the cervicothoracic spine are listed in Table 1.
3. Endoscopic Tubular-assisted
Of the six studies evaluating complications after using the endoscopic tubular-assisted approach, one study of 10 patients undergoing surgical decompression reported no complications [19]. In another paper, Baba et al. [20] described a set of 25 patients undergoing decompression due to ossification of the ligamentum flavum which resulted in thoracic myelopathy. Two complications resulted - one a dural tear which resolved without further treatment, and a second patient developed a postoperative hematoma which required emergent surgical evacuation.
In a larger study of 210 patients undergoing an anterior approach for decompression, one patient sustained an injury to their esophagus, one had C5 root paresis which resolved, two experienced transient dysphagia, two had incomplete decompression, and one had transient voice hoarseness [21]. In two additional studies, one consisting of 31 patients undergoing laminotomy and a second consisting of 38 patients undergoing either foraminotomy or discectomy, the former revealed one incident of C5 nerve root palsy and the latter a CSF leak requiring no intervention [22,23]. A randomized-control trial of 70 patients undergoing open anterior cervical discectomy or cervical micro endoscopic discectomy (33 in the open group, 37 endoscopic) revealed 48% of patients in the open group experienced subjective dysphagia or dysphonia, compared to 16% in the micro endoscopic group [24]. The authors attributed the substantial difference in laryngopharyngeal complications to several factors including the lesser distance the trachea and esophagus need to be retracted using the tubular approach and minimal soft-tissue dissection which subsequently reduces tissue edema. The papers studying the endoscopic tubular-assisted approach in the cervicothoracic spine are listed in Table 2.
4. Uniportal Endoscopic
Eleven studies were identified involving patients who underwent uniportal endoscopic spine surgery, with mention of post-surgical complications. Kim et al. [25], in a study of 254 patients with degenerative spine conditions, reported complications in five patients including a C5 nerve root palsy, infection, drain tip retention, and two cases of inadequate decompression respectively. Lin et al. [26], in a retrospective analysis of 816 patients undergoing decompression or discectomy for thoracic or lumbar disorders, reported a complication rate of 2.57% with 15 patients sustaining inadequate decompression, one a dural injury, two permanent paresthesia, and three a seizure which the authors attributed to irrigation with cefazolin, an antibiotic with potential epileptogenic effects. In three other publications, for patients undergoing discectomy, cyst removal, or foraminotomy respectively, the authors reported complications including two CSF leaks in the first study, one dural leak and one case of transient hypesthesia in the second, and one case of transient hypesthesia in the third [27-29].
In a study of 55 patients undergoing decompression of the thoracic spine, complications including two epidural hematomas (one requiring surgical evacuation), two dural tears, two intercostal neuralgias, two deteriorations of the underlying myelopathy, and one case of leg dysesthesia were observed [30]. In another cohort of 84 patients undergoing either anterior or posterior full-endoscopic cervical discectomy, four surgery-related complications were noted [31]. In the anterior approach group, one patient experienced a transient postoperative headache and another an epidural hematoma requiring evacuation. In the posterior group, one patient had worsening neurologic function in the contralateral lower limb, but these symptoms resolved over three months; a second patient underwent a repeat surgery requiring an anterior approach.
Nie and Liu [32] and Li et al. [33], in patients undergoing spinal decompression reported one instance of post-operative headache (successfully treated with an epidural blood patch) and two dural tears as respective complications. In Kim et al.’s study [18] comparing the microscopic tubular, uniportal endoscopic, and biportal endoscopic approaches, the 38 patients in the uniportal group experienced two complications of a temporary nerve root palsy, and one recurrence of the foraminal stenosis resulting in a complication rate of 7.8%. Finally, in a study where patients underwent either the uniportal or biportal approach for foraminotomy, the 32 patients in the uniportal group experienced three complications of incomplete decompression, durotomy, and transient C5 nerve root palsy [34]. The studies reporting on the uniportal endoscopic approach in the cervicothoracic spine are listed in Table 3.
5. Biportal Endoscopic
A total of thirteen studies examining the biportal endoscopic approach were identified. Of these, six were small studies where patients underwent either decompression or mass excision; these studies reported no complications [35-40]. A larger study of 228 patients reported one instance of a C5 nerve root palsy and another case of incomplete decompression as complications [25]. In a case series of seven patients undergoing foraminotomy for cervical radiculopathy, one patient sustained a dural tear [41].
In a cohort of 643 patients undergoing biportal endoscopic spine surgery for degenerative spinal disease by four experienced surgeons, 29 instances of a dural tear occurred, for an incidence of 4.5% [42]. In another study comparing the uniportal to the biportal approach for foraminotomy, of the 33 patients in the biportal group, one patient’s decompression was incomplete, and there was one instance of each a durotomy, epidural hematoma which did not require operative management, and persistent dysesthesia [34].
Deng et al.’s case control study [43] of 14 patients undergoing decompression for ossification of the ligamentum flavum showed two cases of hyperalgesia, two cases of head and neck pain, and one instance of CSF leakage as complications. In a retrospective review of 109 patients undergoing the biportal technique for the treatment of symptomatic cervical disc herniations, there were no major complications, but one instance of motor weakness of shoulder abduction and elbow flexion secondary to fluid retention in the dorsal epidural space of the patient’s cervical spine which resolved spontaneously over the ensuing month [44]. Finally, in Kim et al.’s study [18] of patients undergoing either the microscopic, uniportal, or biportal approaches for treatment of foraminal stenosis, of the 30 patients in the biportal group, there were two instances of recurrence, one dural tear, and one transient nerve root palsy for a complication rate of 13.3%. The manuscripts that involve the biportal endoscopic approach in the cervicothoracic spine are listed in Table 4.
DISCUSSION
1. Interpretation and Implications
The present review provides a comprehensive list of commonly encountered complications while performing minimally invasive surgery on the cervical or thoracic spine for the treatment of degenerative diseases, neoplasms and cysts. This analysis provides a list of complications surgeons should consider when considering a given minimally-invasive approach for the treatment of a certain spinal pathology in a specific anatomical area. Overall, our review suggests that MIS approaches have less severe complications than open approaches.
Nevertheless, similar complications did occur in all four of the minimally invasive groups. These included dural tears, hematomas, nerve root palsies, and incomplete decompressions or recurrences of the underlying stenosis. Due to the recent and rapid adoption of minimally invasive approaches to the cervical and thoracic spine, associated with continued improvement in equipment design, these procedures involve a substantial learning curve. It is possible that as time evolves, the incidence of these complications will decrease as surgeons become more experienced in the use of these techniques.
2. Limitations
The present review has several limitations. Firstly, a small number of the selected studies contained patients who underwent either cervical, thoracic, or lumbar surgery and did not distinguish between these patient groups when reporting complications. Additionally, one study examining patients undergoing MIS spine surgery included a very small number of open cases in their cohort, introducing the possibility that a small number of the reported complications could have been from open surgery [25]. Some complications, including post-operative headache, were subjective leading to the potential of interviewer bias. Moreover, seeing that many of the included studies were retrospective analyses and not randomized-control trials, the risk of sampling bias and the involuntary exclusion of other complications must be considered.
When considering some of the rates of complications such as dural tear which in one study was reported to be 4.5%, the experience of the surgeon with the technique must be considered; this is especially true for some of the more novel techniques such as the biportal approach. Our review is unable to capture where along the learning curve of various MIS techniques the surgeons were, which may heavily influence complication rates. Finally, many of the contained studies did not provide detailed patient demographic and clinical characteristics which could influence the rate of various complications.