Learning Curve of MIS-TLIF using 22 mm-tubular Retractor in Degenerative Spondylolisthesis (Grade 1-2) - A Review over 100 Cases
Article information
Abstract
Objective
To evaluate the learning curve of MIS-TLIF in degenerative spondylolisthesis with understanding of problems and challenges faced during initial cases.
Methods
After taken approval from institutional review board, first 109 patients who underwent MIS-TLIF for singlelevel low-grade degenerative spondylolisthesis between 2010 to 2015 were evaluated. First 100 cases that formed the study cohort at final follow-up were arranged sequentially in order of date of operation and then grouped in four quartiles. Comprehensive data which included demographics, clinical parameters, surgical parameters, peri-operative incidents (dural tear, technical issues like guide-wire migration, tube docking problems) and complications were assessed.
Results
Median operative time, median blood loss and median radiation exposure gradually decreased as the series progressed, however, showed statistically significant difference between Q1 and Q2 with no significant difference between later quartiles. There was a significant decline in postoperative VAS and ODI scores in all quartiles, however, there was no statistically significant difference in their values on comparison between quartiles. Guide-wire migration, dural tear and tube docking related problems, pedicle screw perforation significantly reduced after 1st quartile.
Conclusion
MIS-TLIF is safe and effective means of treating lumbar spondylolisthesis. The learning curve is achieved between 1st and 2nd quartile (25th to 50th cases). Familiarity with instrumentation, preoperative anatomical planning, better coordination with surgical team and hands-on tissue-training are keys to reduce the learning curve.
INTRODUCTION
Trans-foraminal Lumbar Interbody Fusion (TLIF) has stood the test of time in achieving the aims of reducing the procedure related morbidity as well as fusion rates compared to Posterior Lumbar Interbody Fusion (PLIF). However, drawbacks of open procedure i.e stripping of the para-spinal muscles to far lateral extent for exposure of the entry points for pedicle screw accompany with this technique. Foley first intr oduced Minimally Invasive Surgery-TLIF (MIS-TLIF) in 2002 [1]. It has since then become a popular technique for the treatment of degenerative disc disease with symptoms of radicular pain and canal stenosis with segmental instability because of its advantage over open method of lesser soft tissue injury, unilateral exposure and preservation of contra-lateral structures [2]. On the contrary, it has its own disadvantage like increased operative time, being technically demanding and a steep learning curve [3-5].
Studying the learning curve is important not only to understand the problems faced by a surgeon in initial cases but also to find the way to avoid them, to set guidelines for training and educational purposes, to guide implant-industry for any modifications in instrumentation. Therefore, the effect of learning curve for acquiring a new skill must be considered in order to reach valid conclusions.
The objective of this study was to evaluate the learning curve of MIS-TLIF in large series of lumbar degenerative spondylolisthesis patients with problems and challenges faced during initial cases and some recommendations to reduce them.
MATERIALS AND METHOD
A retrospective evaluation of prospectively collected data of first 109 patients who underwent MIS-TLIF by a fellowship trained spine surgeon for single level low grade degenerative spondylolisthesis (Meyerding grade I or II) between 2010 to 2015 was done.
Subjects with multiple level involvements, revision surgery, spinal deformities, acute spinal fracture, infection or spinal tumor were excluded.
With above strict inclusion and exclusion criteria, we found 100 cases that formed the study cohort. These patients were arranged sequentially in order of date of operation and then grouped in four quartiles (Q1, Q2, Q3 and Q4) of 25 patients each with consecutive each group acting as control to prior.
1. Surgical Procedure
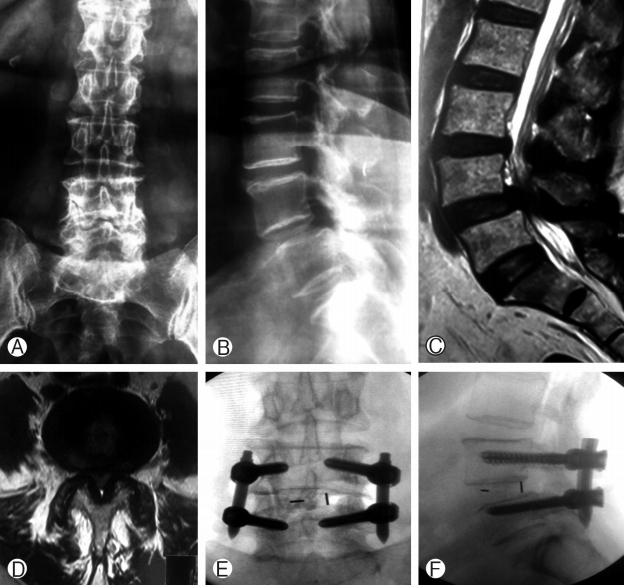
Under general anesthesia, patient was positioned prone on a radiolucent operating table. Under fluroscopic guidance, pedicle images of to be operated vertebrae were confirmed. A 3 cm long paraspinal incision 3-4 cm away from midline was given on the more symptomatic side for decompression utilizing the same for pedicle screw insertion on that side. Sequential dilatation was done and tubular retractor with 22 mm diameter (METRx, Medtronics) was docked over the facet and spino-laminar line. Ipsilateral facetectomy and laminotomy, along with removal of ligamentum flavum were performed under microscope to accomplish adequate neural decompression. Following discectomy and preparation of end plates, appropriate size interbody cage filled with autologous bone was inserted and remaining bone graft was packed into inter-vertebral space medially. Pedicle screws and rods were then inserted through the incisions percutaneously over guide wires on the contra-lateral side followed by ipsilateral side. Bilateral compression was applied before final tightening. Closure in layers was performed following wound hemostasis and copious irrigation.
All the patients were mobilized in-bed on the day of surgery and advised out of bed mobilization depending upon pain on next day by physiotherapist with explained precautions of avoiding bending forward, lifting weight and ground level sitting for 6 weeks. Patients were followed up at 6 weeks, 3 months, 6 months, 1 year and then yearly. CT scan was done at 12 months for evaluating fusion and pedicle perforation.
Comprehensive data which included demographics (age, sex, BMI, co-morbidities, operated level and duration of follow-up), preop and post-operative clinical parameters [Visual Analogue Scale (back and leg), Oswestry Disability Index (ODI)], surgical parameters [operative time, blood loss, radiation exposure (Gy.cm2)], peri-operative incidents (dural tear, technical issues like guide-wire migration, tube docking related problems) and complications [new-onset radiculopathy or neurological deterioration, infection, pedicle screw perforation, implant loosening or pseudo-arthrosis] were compiled and assessed. Dose Area Product (DAP) was used as the measure of radiation exposure as it best correlates with the effective dose [10]. The fusion was evaluated according to modified Bridwell criteria where grade I (fused with remodeling and trabeculae present) and II (Graft intact, not fully incorporated and remodeled but not lucency present) were considered as solid fusion [6,7].
Case 1: 55 year male patient operated by MIS-TLIF for grade 1 degenerative spondylolisthesis (Fig. 1)
2. Statistical Analysis
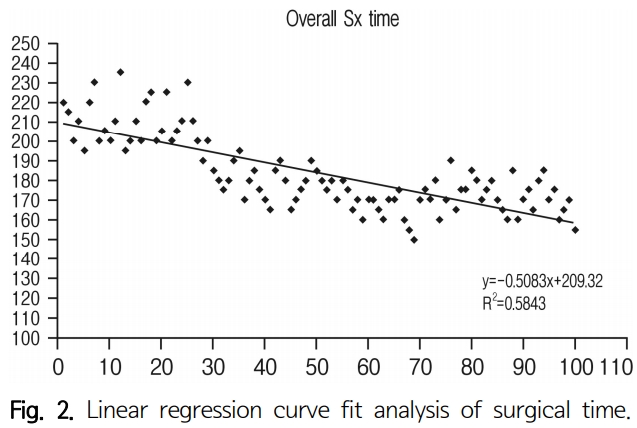
Standard SPSS 20.0 software was used for statistical analysis. Linear regression analysis was used to observe the trend of surgical time and ANOVA test was used to compare each variable in different quartiles. ‘P’ value <0.05 was considered statistically significant.
RESULTS
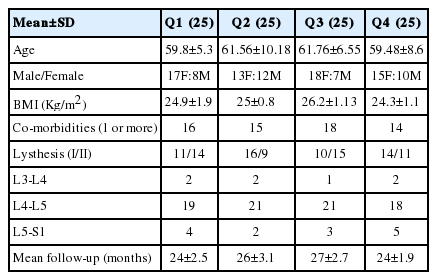
Patients ranged from 37-77 years with average age 60.89 years. The study group comprised 37 men and 63 women. Average BMI of patients in each quartile was comparable (Q1-24.9, Q2-25, Q3-26.2 and Q4-24.3). Number of patients with one or more co-morbidities were 16, 15, 18 and 14 in Q1, Q2, Q3 and Q4 respectively. The cohort of each quartile was thus homogenous and comparable in regards to demographics. Regarding the level of operation, 79 cases were at L4-L5, 14 cases were at L5-S1, and 7 cases were at L3-L4 levels. Mean follow-up of patients was 24±2.5, 26±3.1, 27±2.7 and 24±1.9 months in Q1, Q2, Q3 and Q4 respectively (Table 1).
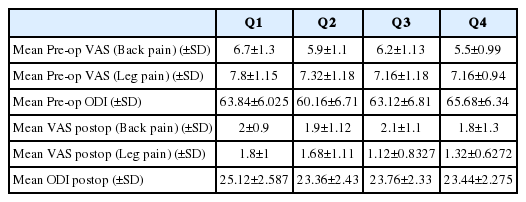
There was a significant decline in post-operative VAS (leg and back) and ODI scores in all quartiles, however, there was no statistically significant difference in their values on comparing between quartiles (Table 2).
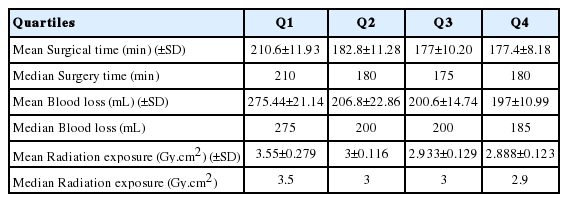
Median operative time (Q-210, Q2-180, Q3-175 and Q4-180 mins), median blood loss (Q1-275, Q2-200, Q3-200 and Q4-185 mL) and median radiation exposure (Q1-3.5, Q2-3, Q3-3 and Q4-2.9 Gy.cm2) gradually decreased as the series progressed, however, showed statistically significant difference between first two quartiles only. There was no significant difference between later quartiles i.e. Q2-Q3 and Q3-Q4 for the above three parameters (Table 3, Fig. 2).
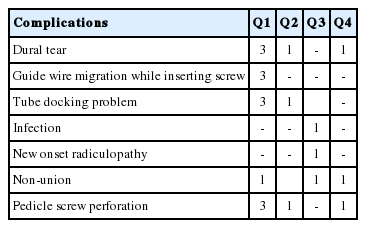
No cases were converted to open surgery. Dural tear occurred in 5 cases- 3 in Q1, 1 in Q2 and 1 in Q4. All cases of dural tear were managed with fibrin sealant (TISSEEL) and water- tight closure of the wound. No delayed CSF leaks or pseudo-meningocele developed.
Guide-wire migration occurred in 3 cases in first quartile and improper tube-docking occurred in 3 patients in Q1 and 1 patient in Q2.
Superficial wound infection was found in 1 case in Q3. The patient recovered with regular dressings and oral antibiotics.
Non-union was found in 3 cases; 1 in Q1, Q3 and Q4 each at 1-year follow-up on CT scan.
Pedicle screw perforation was found in 5 cases: 3 in Q1, Q2, Q4 resp. Out of them, 1 case (case 56) was symptomatic with new onset radicular pain. Perforation was diagnosed on immediate CT scan and posted for revision of screw. The radicular pain subsided immediate postoperatively. There were no cases of neurological worsening or implant loosening at final follow-up (Table 4).
DISCUSSION
Every surgeon performing a new procedure faces certain difficulties that he overcomes over a period of time. Moreover, in MIS procedures it takes greater time for a new surgeon’s psychomotor skills of operating through a narrow channel by viewing under microscope to evolve. This study aims to evaluate the learning curve of MIS-TLIF with problems and challenges faced during initial cases.
Yang et al. retrospectively studied 65 cases of single level MIS-TLIF performed and found asymptote at 21st case [8]. KH Lee reported a prospective cohort study of 90 cases of single level MIS-TLIF and concluded that asymptote lied at 44th case [9]. Pedro et al. retrospectively studied 150 cases and concluded that 90% of learning happened by 30th case [13]. JC Lee et al. studied prospective data of 86 cases with logarithmic curve-fit regression analysis for single level MIS-TLIF and reported asymptote at 22nd case [4]. In our study, we found asymptote around 25th case in 1st quartile. Therefore, novice surgeon has to perform 25 to 50 cases minimum for achieving the mastery in this technique as different surgeon has different learning abilities.
Yang et al. found surgical time, blood loss and fluoroscopy time as the factors correlating with the learning curve [8]. Lee KH demonstrated three variables viz. Surgical time, fluoroscopy time and patient controlled analgesia as the correlating variables [9]. They also found that the clinical parameters at final follow-up in early and late groups were different. JC Lee found in addition to surgical time and blood loss, ambulation recovery time also significantly improved in later cases [4].
The steep decline in operative time and blood loss till 2nd quartile in our study might be attributable to accurate placement of tubular retractor at desired level in shorter period of time. Knowledge of using appropriate size tubular retractor had also led to decreased soft tissue herniation which ultimately lead to decreased operative time and blood loss. We recommend 10 mm longer tube retractor than the actual size measured on tube aiding in a flush to lamina docking preventing muscle creeping.
Radiation exposure also significantly decreased in 2nd quartile as compared to 1st quartile from 3.5 Gy.cm2 to 3 Gy.cm2. Better understanding of taking true AP and Lateral images also helped in reduction of exposures. Also, the perception of the suboptimal images by the surgeon improves over time and maintaining the surgical sequence same aids the technician in knowing the required position of C-arm for the next step.
There was no significant difference in improvement of clinical parameters between the quartiles as extent of decompression was remained the same in all patients.
5 dural tears had occurred in our study, 3 were in Q1, 1 in Q2 and 1 in Q4. Higher incidence in Q1 was mainly due to guide-wire perforation of dura while docking of tube hence discontinued using guide-wire while tube docking after certain cases in Q1.
Guide-wire migration occurred in 3 cases in Q1 in our study at the time of pedicle screw insertion. Passing the guide-wire only until junction of posterior 1/3 to anterior 2/3 of vertebral body as on C-arm, holding the wire tightly by assistant while removing instruments and use of threaded blunt-tipped wires helped in preventing this complication.
Tube docking related problems occurred in 3 patients in Q1 and 1 patient in Q2 which indirectly led to increased operative time and blood loss in initial cases. In Q1, 2 patients had inferior docked tube due to high inclined laminae and 1 patient had superior docked tube led to difficulty in identify the anatomical landmarks. In all cases, we removed the tubes and reinserted it back at correct position. 1 patient in Q2 with severe facet-joint hypertrophy had problem in identifying the spino-laminar line and facet joint. The dissection was carried out until we reached the spino-laminar line with appreciable facet-joint laterally and then tube was re-docked.
Pedicle screw perforation was encountered in 5 cases: 3 in Q1, 1 in Q2 and Q4 respectively. The higher number of screws perforated initially can be attributed to lack of tactile feeling with needle tip and bad selection of optimal entry point with less knowledge of taking true fluoroscopic images while inserting the screws.
Sclafani performed a systematic review for MIS articles and found that for MIS fusion procedures, the most common complications were implant mal-position, neural injury, and nonunion [11]. Overall complication rate for MIS TLIF was 20%. Yung P et al. in their study concluded that the perioperative complications were far more common in early period of surgeons experience with MIS-TLIF [12]. Pedro S et al. found complication rates of 33 % before 50% learning was achieved as compared to 20.51% after 90% learning [13]. In our study, complication rates were comparable to previously mentioned studies, however on contrary, complications happened at any level in all quartiles demonstrating the need for cautious care even after mastering the technique. Guide-wire migration issues and technique related problems were much more in 1st quartile as compared to successive quartiles (Table 5).
LIMITATIONS
Our study include its retrospective nature; however, database was prospectively maintained. Certain non-modifiable confounding factors were present which include- individual surgeons learning ability as some surgeons are slow while some are quick learners and other MIS procedures performed by the surgeon during the study duration.
We recommend certain guidelines to follow by novice surgeon during initial cases and practicing them on bone sawbone models and tissue-training in mentoring programs to reduce the learning curve of this technique -
1. Proper pre-operative planning with best knowledge of anatomical landmarks.
a. Pedicle anatomy, length, diameter congenital abnormality should be studied on preop CT scan.
b. Anatomic landmarks like inclination of laminae, broader/narrow laminae, bulbous spinous process, facet joint hypertrophy should be studied.
2. Appropriate patient selection. Avoid obese patients in initial cases.
3. Proper patient positioning.
4. Always take True-Lateral/AP fluoroscopic image while inserting guidewires and tube docking.
5. Based on the patient size and obesity, skin incision can modify to more lateral position.
6. Use appropriate length of tubular retractors. Longer length can lead to increase in working length of the instruments and shorter to more soft-tissue herniation.
7. Diameter of the tube is utmost important and depends on patient size and facet joint hypertrophy. Larger retractor makes localization and performance better however, in smaller patients, larger tube may impinge on spinous process or laminae limiting the depth of insertion with more soft tissue herniation.
8. Don’t use the guide wire during tube docking
9. Dock the tube exactly at facet joint with spino-laminar line visible and start your first bite of laminotomy at spino-laminar junction followed by facetectomy.
10. Avoid the use of burr while doing laminotomy in initial cases.
11. During facetectomy, ligamentum flavum should remain intact till bony decompression is complete; it reduces the incidence of dural tear.
12. While inserting pedicle screw, spend time to obtain tactile feeling with needle tip and try to palpate the bony junction between lateral facet and transverse process to select optimal entry point and get appropriate medial to lateral trajectory of needle until its tip appears at lateral cortical margin of pedicle in AP view.
13. Guide wire should not be placed anterior to junction of anterior 1/3 and posterior 2/3 of the vertebral body.
14. Avoid driving screws too much deeper than necessary to prevent the screw tulip from resting on facet joint
15. Practice to handle the microscope on models for better eye-hand coordination.
CONCLUSION
MIS-TLIF is very safe and effective means of treating lumbar spondylolisthesis. With the asymptote being at 25th case, familIarity with instrumentation, preoperative anatomical planning, better coordination with surgical team and hands-on tissuetraining with above mentioned guidelines are keys to reduce the learning curve.