Essential Surgical Techniques During Unilateral Biportal Endoscopic Spine Surgery
Article information
Abstract
Unilateral biportal endoscopic spine surgery (UBE) is a popular minimally invasive method for various types of spinal disease. UBE is similar to full percutaneous endoscopic spinal surgery in that it uses endoscopic instruments and similar to microscopic spinal surgery in that it uses a floating technique. UBE is a useful surgical technique in unilateral or bilateral decompression for the treatment of spinal canal stenosis, foraminal stenosis, ossification of the ligament flavum, low-grade spondylolisthesis, and adjacent segment degeneration. This surgical technique has several advantages over conventional spine surgery, including less tissue damage, less blood loss, shorter hospital stays, and faster recovery. In addition, the early clinical outcomes are favorable, despite the potential for complications, such as dura tearing, nerve traction injury, and postoperative hematoma. The essential surgical techniques in UBE are patient positioning, portal creation, endoscopic visualization, decompression, and fusion. Postoperatively, patients may experience less pain, require fewer analgesics, and return to daily activities quicker. We present an overview of the essential surgical techniques used in UBE and the avoidance of complications.
INTRODUCTION
The surgical procedures for spine disease have developed significantly over the last century. Since 1970, conventional spine surgery is performed by dissecting paraspinal muscles using microscopy and special retractors. These open and microscopic spine surgeries are considered standard surgical procedures [1,2]. However, substantial advances have been achieved in surgical procedures using minimally invasive techniques aimed at reducing surgical trauma, improving clinical outcomes, and promoting postoperative recovery.
Unilateral biportal endoscopic spine surgery (UBE) was a pioneering technique, providing a less invasive alternative to conventional spine surgery in various spinal diseases. Forsts and Hausmann were the first to use an arthroscope intradiscally in the early 1980s [3]. At the beginning of the 21st century, several authors introduced various spinal decompression techniques to preserve the posterior midline structures, including endoscopic spine surgery [4-6]. UBE has progressed due to the development of the endoscope and specialized surgical instruments [7]. The development of endoscopic instruments generated a subspecialty of minimally invasive spine surgery that shifts the point of visualization away from the surgeon’s eye or microscope and places it directly at the site of the spine pathology with an endoscope [8]. This technique has been used for various minimally invasive spinal decompression procedures, such as laminotomy for lumbar discectomy, unilateral laminotomy for bilateral decompression, and unilateral foraminotomy. Excellent clinical outcomes have been achieved through these techniques [7,9-11]. Additionally, they allow the visualization of the spinal structures via 2 small incisions on one side of the spine, thus minimizing tissue injury and enhancing postoperative recovery. Due to these advantages, UBE is increasingly widely performed, approximately one hundred UBE cases are performed annually at our institution.
Early endoscopic spine surgery was used generally to treat disc herniation and was less invasive than traditional open techniques. Surgeons now have the surgical instruments and expertise to treat a wide range of spine pathologies beyond lumbar disc herniation. However, the technique requires specialized training and instruments, and there is a steep learning curve for beginners. Furthermore, there are potential risks and complications, including nerve injury, dura tear, postoperative hematoma, and infection. Surgeons need to adhere to established protocols and guidelines to ensure optimal patient outcomes. This article aims to describe in detail, with references to current literature, the essential surgical techniques used during UBE.
INDICATIONS
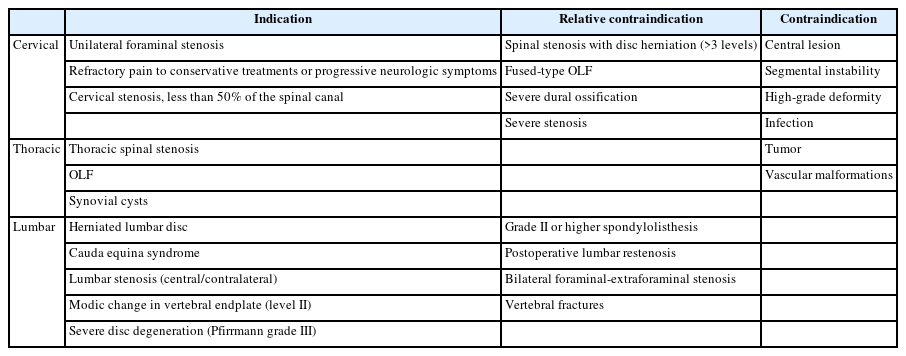
In general, the indications for UBE are similar to those for conventional open and microscopic spinal surgery. When conservative treatment is ineffective or the neurologic symptoms of the patient worsen, a surgical procedure by UBE is recommended. The following describes the indications and contraindications for a surgical procedure by UBE: (1) spinal stenosis or foraminal stenosis; (2) hypertrophied ligamentum flavum (LF), ossification of ligamentum flavum (OLF) involving less than 50% of the spinal canal; (3) low-grade spondylolisthesis (I or II). The following are contraindications for a surgical procedure by UBE: (1) central lesion on the level of the spinal cord; (2) high-grade deformity; (3) tumor or vascular malformations; (4) severe dural ossification or severe stenosis; (5) high-grade spondylolisthesis (III or IV); (6) bilateral symptomatic foraminal-extraforaminal stenosis; (7) instability of the spinal column; (8) vertebral fractures or pathologic conditions because of the risk and technical challenge (Table 1).
SURGICAL TECHNIQUE
1. Anesthesia and Patient Positioning
UBE is performed under general, epidural, or spinal anesthesia. However, in cervical surgery, it is performed under general anesthesia. General anesthesia is preferred in most cases, as it allows greater muscle relaxations, facilitates patient positioning, and reduces the risk of unintended patient movement during surgery. Careful consultation with an anesthesiologist is required before performing surgery at the spinal cord level, as intraoperative neurophysiological monitoring may be necessary.
Most UBE spine surgeries are performed in the prone position using a Wilson frame or Jackson table, although it is possible to change position depending on the surgical approach. It is important to reduce lumbar lordosis and increase the foraminal space by flexing the hip and knee joints. Also, an important key in patient positioning is to reduce abdominal pressure to prevent epidural bleeding.
Even cervical surgery is performed mostly using the prone position. To reduce the pressure on the abdomen, an H-shape pillow should be used to relax it. The neck should be flexed, and the upper back should slope downward. This improves venous return, reducing bleeding during surgery. To check the C6–7 level or lower, the head should be fixed by head fixation, and the shoulder should be pulled down using a plaster. During surgery, mean arterial pressure must be maintained below 80 mmHg to reduce intraoperative bleeding.
2. Localization and Portal Creation
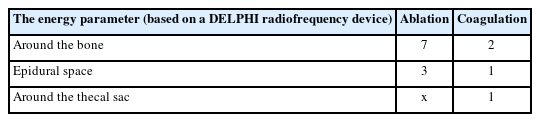
When performing UBE lumbar spine surgery, the C-arm is used to check the target level and set it parallel to the endplate. At the junction of the medial pedicle line and the points 1 cm above and below the target disc space, 2 skin incisions are made. The appropriate distance between the 2 skin incisions is 2 to 3 cm apart, and the skin incisions are approximately located in the lower margin of the proximal pedicle and the midpoint of the distal pedicle (Figure 1A). The docking point for the discectomy and decompressive laminectomy is the inferior margin of the upper lamina. Obviously, in cases of obesity, a high-level disc, or hyperlordosis, it should be appropriately modified according to the patient. Since it is also different depending on the disc space angle, the angle must be determined using a preoperative radiologic image. The endoscopic portal size should be 7 mm or larger, and the working scope should be 9–10 mm or larger, so that the endoscope and instrument can be inserted properly, and the saline flow can be maintained smoothly. The direction of the skin incision can be either horizontal or transverse. To decompress the exiting nerve root or to remove up-migrated disc herniation and foraminal disc herniation on the contralateral side, 2 portals should be placed slightly below the routine portal. However, to decompress the traversing root or to remove the down-migrated disc on the contralateral side, 2 portals should be placed slightly above the routine portal. Modification of these portals can reduce unnecessary bone work.
(A) Skin incisions for unilateral biportal endoscopic spinal surgery (UBE) in discectomy and laminectomy. Routine portal skin incisions for a left-sided approach. At the junction where the line of the medial border of pedicles and the line of the intervertebral disc space meet, 2 skin incisions are made at a point 1 cm from the top and bottom. The docking point is the inferior margin of the cranial lamina. (B) Paraspinal skin incisions for the left-sided. The scope portal, instrumental portal, and isthmus docking point are illustrated on the x-ray anteroposterior (AP) view. The portal is made at the junction of the lateral margin of the transverse process (TP) and the points 1 cm above and 1 cm below the target disc space. (C) Paraspinal skin incisions at the L5/S1 level for approaches from both sides. For the left-sided approach, the scope portal is the same as the routine paraspinal approach portal and the instrumental portal is 1 cm to the medial side from the routine portal. For the right-sided approach, skin incisions are made 1 cm proximal to the routine incision placement. Both docking points are the L5 isthmus. (D) UBE lumbar interbody fusion (ULIF) skin incisions for the left-sided approach. At the junction where the midline of the pedicle and the line of the intervertebral disc space meet, 2 skin incisions are made 1 cm from the top and bottom. The docking point is the inferior margin of the cranial lamina. (E) Modified far-lateral transforaminal lumbar interbody fusion using UBE skin incisions for the left-sided approach. At the junction where the lateral border of the pedicle and the line of the intervertebral disc space meet, 2 skin incisions are made 1 cm from the top and bottom. The docking point is the inferior margin of the upper lamina. (F) The skin incision points of posterior cervical foraminotomy are marked on the upper and lower pedicles around the target level. Two skin incisions for the scope portal and the instrumental portal are illustrated in the figure. The blue line indicates the medial border of the pedicle. The docking point is the “V” point between the upper and lower lamina.
In a paraspinal approach, the upper and lower pedicles and the transverse process of the level are indicated using the C-arm. After adjusting the angle of the C-arm parallel to the endplate of the target level, the portal is made at the junction of the lateral margin of the transverse processes and the points 1 cm above and 1 cm below the target disc space (Figure 1B). The docking point is the isthmus. There is also a method to make skin incisions at an angle of about 30°–40° and check the preoperative computed tomography or magnetic resonance imaging (MRI) in advance to determine the distance of the skin incision from the midline before performing surgery (Figure 2). After a skin incision is made, the docking point of the endoscope and the working instrument is set to the isthmus. However, at the L5/S1 level, a different location is required for the portal placement because of the iliac crest. In the L5/S1 Left side approach, the scope portal is the same as the routine portal and the working portal is 1 cm from the routine portal on the medial side. Each skin incision is made at the lateral margin of the L5 transverse process and the lateral margin of the sacral alar, and the distance between the incisions is approximately 2–3 cm. On the L5/S1 right side approach, the incision is made 1 cm from the routine portal placement on the proximal side (Figure 1C). Unlike other levels, the paraspinal approach at the L5/S1 level has a very restricted surgical field because of the prominent iliac crest, oblique pedicles, and more coronally oriented facet joint. The docking point of the endoscope and instrument is determined by the lateral border of the superior articular process (SAP), the lateral border of the sacral alar, and the osseous triangle at the base of the L5 transverse process.

The appropriate trajectory for the paraspinal approach (white line) is 30° to 40°. Skin incisions should be different according to the degree of obesity or anatomical features.
In far-out syndrome decompression, the skin incision is made 1–2 cm lateral to the lateral margin of the vertebral body under C-arm fluoroscopy anteroposterior view confirmation. A skin incision is made 1 cm above and 1 cm below the intervertebral level, and the distance between the 2 skin incisions is about 2–2.5 cm. The landing point of the first dilator is very important. The aim in far-out syndrome decompression surgery is to remove the transverse process and pseudo-articulation of the sacral alar. It is important to place the first dilator through the working portal aiming at the junction of the SAP of S1 and the sacral alar and to place the endoscopic portal near the sacral alar or sacral notch for triangulation. Meticulous dissection and detachment should be performed around the bony structure, and saline flow should be maintained between the bony structure and soft tissue. The lateral aspect of the SAP, sacral alar, and even the lower border of the transverse process must be confirmed.
In revision surgery, it is important to make an incision that is slightly more lateral than when using a previous wound. Due to the characteristics of revision surgery, it is easy to lose orientation as a consequence of peridural scar tissue when entered through a previous incision; therefore, approaching from the lateral side and operating on the facet joint and lamina can be a safe procedure.
The skin incision for fusion using an endoscope is slightly different from the incision for decompression. After placing the C-arm parallel to the endplate, 2 skin incisions are made on the midline of the proximal and distal pedicle. Using the carinal lamina itself and the inferior margin as a docking point, a working and endoscopic portal is made approximately 3 cm away (Figure 1D). Pedicle screws are inserted using the previously made skin incisions. When performing modified far-lateral transforaminal lumbar interbody fusion, 2 skin incisions are made at the lateral border of the pedicle (Figure 1E).
In posterior cervical surgery, a skin incision is made vertically in the midline of the pedicle under C-arm fluoroscopic confirmation. It is made near the upper pedicle and lower pedicle, about 2 cm apart (Figure 1F). The operative angle is approximately 20°–25°. If the patient is obese, the 2 incisions should be wider and placed laterally from the midline. A #10 blade is used to make a deeper incision into the fascia until it touches the bone, with the guidance of the C-arm. Unlike lumbar, cervical surgery requires a deep enough incision because there are several layers of fascia and muscle. A wide blade is used because the dissection is safer with wider blades and can be performed without penetrating the interlaminar space.
3. Endoscopic Visualization
The initial docking point of the endoscope and the serial dilator is the location between the pathologic level of the spino-laminar junction and the inferior margin of the caudal lamina. Using the first serial dilator or muscle dissector, the paraspinal muscle should be sufficiently dissected on the lamina around the docking point. This is to guarantee sufficient saline patency. Muscle detachment should be performed from the lower border of the cranial lamina at the pathologic level to the upper border of the caudal lamina. It is performed by using the ablation mode of a radiofrequency (RF) probe and removing soft tissue with a muscle shaver; the endoscope and surgical instruments are triangulated. The outer layer of LF and bulky soft tissue should be removed using a Kerrison punch or pituitary forceps to confirm the landmark of laminectomy.
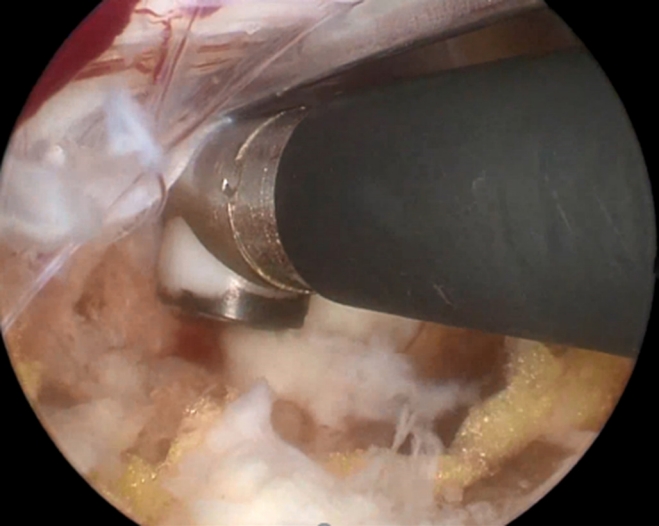
It is necessary to check whether the saline patency is smooth before laminectomy. A 3,000-mL saline bag is placed 80–100 cm above the patient’s back (100 cmH2O injection pressure) or an automatic pressure pump is used. Water pressure should not exceed 30 mmHg if possible [12]. The use of working sheaths or cannulas to maintain smooth water flow during surgery in patients with excessive muscle mass or who are obese is also an essential surgical technique (Figure 3). This allows the irrigation fluid to create a working space in the UBE. If a dura tear occurs, the intracranial pressure (ICP) can increase, and this increase is higher the closer it is to the cord level. Increased ICP can cause postoperative headaches, neck stiffness, seizures, and retroperitoneal fluid collection [13]. Even if there is no dura tear, high water pressure can cause postoperative back pain and neck pain, so low water pressure is recommended during UBE spine surgery (Supplementary video clip 1).

(A) Intraoperative field image of adequate saline flow. (B) Using working sheaths or cannulas helps to maintain a smooth saline flow during surgery.
The docking point in the paraspinal approach is the lateral edge of the isthmus. Under C-arm guidance, a guide pin and instruments are placed on the isthmus and the exit of the foramen. Using a Cobb elevator, the muscles attached to the lateral edge of the isthmus, the SAP of the facet joint, and the transverse process should be dissected to create a sufficient surgical field. Radicular arteries are distributed around the facet joint; it is therefore important to prevent bleeding by adequately coagulating the area with an RF probe before performing bone work. In far-out syndrome decompression, because the radicular artery runs over the sacral notch, greater caution is necessary when dissecting muscle around the sacral notch. When bleeding is unexpectedly severe, it is necessary to control the bleeding after confirming the bleeding site by placing the endoscope close to it. Occasionally, if the hypertrophy of the facet joint is extremely severe or if access to the lateral edge of the isthmus is challenging due to a decrease in intervertebral disc height, the isthmus can be reached by approaching the lateral edge of the SAP of the lower facet joint. The next step is to check the upper and lower transverse process.
In revision surgery, anatomical landmarks are often unclear due to overgrowth by scar tissue. The caudal border of the superior lamina, medial border of the facet joint, and upper border of the caudal lamina are undercut and dissected using a diamond drill, chisel, or small-head curve curette until the healthy dura of the traversing root is exposed. When the lateral margin of the traversing root is exposed, the outer annulus of the intervertebral disc is exposed by careful medial retraction. During the process of exposure, if there is adhesion between the dura and the disc space, a blunt dissector or a small nerve hook is used carefully to dissect the scar tissue and enable safe access.
In posterior cervical surgery, the surgical field is created by dissecting neck muscle using serial dilators. Endoscope and instrument insertion require intraoperative fluoroscopic confirmation because the interlaminar space can be penetrated and cause cord injury. First, surgeons should insert a 0° endoscope and a working instrument and check the saline flow patency. Using a natural drainage or pump system, it is safe to set water pressure below 30 mmHg. Next, the V-point where the superior lamina, inferior lamina, and medial aspects of the facet joint intersect should be checked with the endoscope and instrument after triangulation. Then the surgical field can be created by removing the remnant soft tissue around the V-point. Before bone drilling, it is recommended to expose the entire lamina using an RF probe.
4. Decompression
The anatomical landmark is checked by soft tissue dissection, and then a laminectomy is performed. The laminectomy is started from the lower border of the cranial lamina, using a drill or osteotome until a free margin of LF is obtained. Then, the V-shaped central fissure of the LF is distinguished from the lower border of the cranial lamina, bone work is performed until the cranial, lateral, and caudal sides are freely detached. To prevent fracture of the isthmus or inferior articular process, the proximal edge of the LF can be detached using curved curettes when the laminar isthmic space is narrow. The lateral margin of the nerve root and the dural sac are checked while removing the LF. Sufficient bone work and removal of the LF are done to reduce unnecessary traction. If additional bone work is required after LF, a drill can cause a dura tear; therefore, a small osteotome can be used as an alternative.
In the contralateral sublaminar approach, the LF on the contralateral side and the ventral side of the lamina should be detached using a freer or curette before contralateral decompression. Contralateral sublaminoplasty should be performed until the edge of the contralateral LF is free, and is performed generally until the medial side of the contralateral facet joint is exposed. Because a dura tear can occur as a result of a central portion defect of the LF, the base of the spinous process should be removed carefully. When the contralateral lamina is undercut using an osteotome or endoscopic drill, the LF is not removed to protect the neural structure. It is recommended to proceed between the LF and the ventral side of the lamina. When a lateral recess has a calcified lesion or bony structure, a straight or curved osteotome is used for decompression rather than a Kerrison punch. However, when removing the lesion or down-migrated disc around the exiting root of the contralateral side, the laminotomy area on the ipsilateral side of the lesion can be minimal (Figure 4A), but the upper portion of the lower lamina needs sufficient bone work for easy access. It is helpful to remove the upper portion of the contralateral lamina and the SAP. By removing the contralateral LF, the contralateral traversing nerve root can be identified, and by removing the foraminal ligament, the exiting nerve root can also be identified. The endpoint of decompression is the exposure of the medial border of the contralateral pedicle and restoration of dural pulsation. Adequate decompression may not be obtained if the medial side of the SAP is not exposed (Figure 4B). Furthermore, the authors advocate decompressing over 3 mm laterally from the lateral margin of the dural sac during continuous irrigation, because the dura shrinks under hydrostatic pressure. In contrast to the endoscopic view, the true lateral margin of the dura in its natural state may be located further laterally.
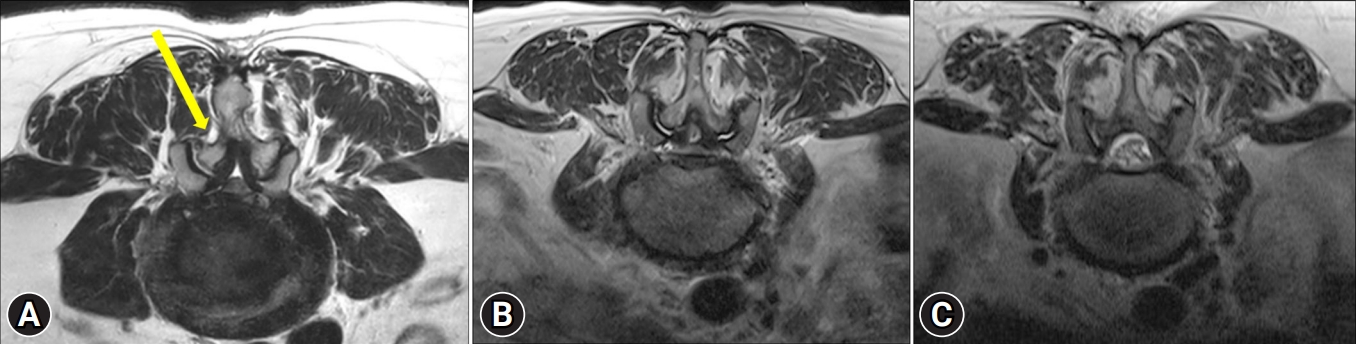
(A) Compared to conventional open surgery, bilateral decompression through the contralateral sublaminar approach (yellow arrow) in unilateral biportal endoscopic spinal surgery is a method to minimize the laminectomy area (yellow area). Compared to the preoperative magnetic resonance imaging (MRI) (B), the postoperative MRI (C) showed that the neural structure was well decompressed with minimal laminectomy. Adequate decompression may be obtained after the medial side of the superior articular process is exposed.
In a paraspinal approach, the lateral edge of the isthmus and the SAP tip are key structures. Using a Kerrison punch and drill, foraminoplasty is performed to decompress the neural structure and remove surrounding tissue. Then, the LF is detached and removed using an angled curette to expose the exiting nerve root and perform discectomy and additional bone work to decompress the neural structure. When soft tissue is dissected, the transverse process, isthmus, and facet joint are exposed. In the case of a hypertrophic facet joint, removing the SAP cranial tip with a diamond drill or osteotome to create sufficient space facilitates safe surgery. If the SAP tip is not removed sufficiently because of concerns regarding instability, the surgery becomes more difficult; therefore, it must be removed adequately. Even if the SAP tip is removed sufficiently, instability is not caused generally, but further study is required to confirm this. Discectomy is performed using a pituitary rongeur, curette, etc. Additional discectomy, often from the axilla region of the exiting root, may now be performed if the offending pathology is a herniated lumbar disc. In the approach at the L5/S1 level, drilling is first performed on the base of the L5 transverse process and the cranial and lateral sides of the SAP. If the SAP is too deep and too steep, it is difficult to access with a drill, so an angled instrument, such as a hockey stick chisel and an angled pituitary clamp can be useful. In obese patients, a 30° scope may be helpful rather than a 0° scope. Depending on the conditions, removing the sacral alar can be an important procedure for creating sufficient surgical space. To perform an L5 exiting root decompression and discectomy safely, sufficient space must be obtained. When the bone work is done, remove the LF using a Kerrison punch or curette. When anatomy is confused, discography can help to identify the anatomy. Some surgeons do not perform enough SAP resection because of the concern that excessive SAP removal could lead to instability in patients. However, this may lead to insufficient neural decompression and continued symptoms. According to biomechanical studies, resections of less than 75% do not result in segmental instability [14,15].
In far-out syndrome decompression, an endoscopic drill is used after exposing the lateral aspect of the SAP, the sacral alar, and the lower border of the transverse process. Bleeding occurs as the cancellous bone is exposed at times and bleeding should be controlled using an RF probe or bone wax. During the procedure, pseudo-articulation is identified and should be removed laterally as much as possible. After removal, the foraminal ligament covering the exiting nerve root must be checked and sufficiently removed. The LF attached under the transverse process should be detached and safely removed using a small Kerrison punch, angled curette, etc., and the exiting nerve root below this is checked. The annulus of the intervertebral disc can be identified and, if necessary, ventral decompression can be performed through discectomy.
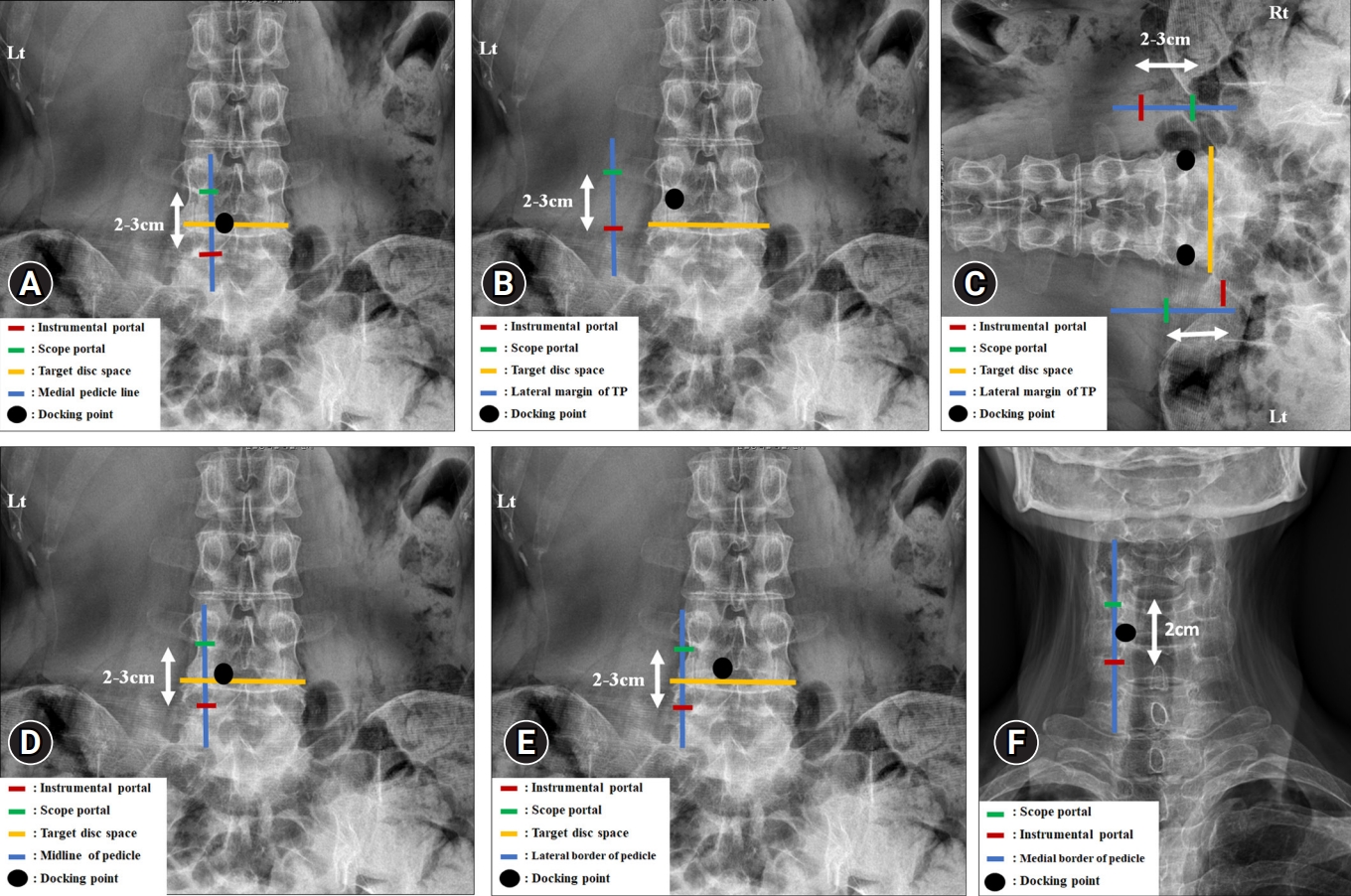
Discectomy varies slightly depending on the location of the lesion and the characteristics of the disc. Generally, a retractor is used to sufficiently protect the root during discectomy, then an annulotomy is performed using an Indian knife, etc., and removal of the disc using pituitary forceps. Calcified discs are removed using a Kerrison punch or osteotome. During a discectomy, the nerve should be protected continuously, and it is also helpful to use scope retractors and assistant retractors. Expose the disc space by carefully performing dura retraction on the disc on the contralateral side as well as the ipsilateral side, and remove it using an angled hook, small pituitary forceps, and an angled upbite pituitary. Epidural bleeding control and annuloplasty should be performed using an RF probe, and the power of the RF probe must be lowered near the dura (Table 2) [16-18]. Also, to reduce traction injury, it is important to perform root release intermittently. To reduce recurrence, internal disc decompression and nucleus pulposus must be adequately removed using an RF probe and annuloplasty is also performed.
Decompression in posterior thoracic surgery is comparable to decompression in lumbar surgery. The difference is that cord injuries must be avoided. The thoracic spinal canal is narrower than the lumbar spinal canal, the lamina is short and thick and overlaps the cranial and caudal lamina. Therefore, when bilateral decompression is performed through the unilateral approach, there is a high risk that the endoscope and working instruments excessively compress the cord, resulting in a thoracic cord injury. Therefore, it is necessary to sufficiently remove and undercut the base of the spinous process to expand the working space more than when performing lumbar surgery. To avoid neural injury during thoracic surgery by UBE, the LF is left in place as protection until all bone work is complete. Until the lateral edge of the thecal sac is checked out, which is naturally confirmed through epidural fat tissue, the remaining medial border of SAP (ipsilateral and contralateral) can be removed. The medial side of the facet joint, with as much remaining as possible for stability, overlaps the lateral end of the laminectomy. The 3 key steps in thoracic OLF removal are thinning, detaching, and removal. OLF is difficult and risky to remove with a Kerrison punch. When removing the OLF, it is important not to apply unintentional compression to the spinal cord. After exposing the OLF, the operator grinds until it is thin and translucent using a diamond drill. The thinned OLF should be detached from the thecal sac using a freer elevator and gently removed. If necessary, remove it piece by piece using a 1-mm Kerrison punch or small-sized pituitary forceps. If OLF removal fails due to dural ossification or severe adhesions, the floating method is a good alternative, leaving the OLF on the thecal sac. Above all, an important surgical tip is to experience sufficient lumbar spine surgery before thoracic spine surgery with UBE.
In posterior cervical foraminotomy surgery, partial laminectomy and facetectomy are performed at the V-point using a 3.5-mm diamond burr. Before using a drill, the V-point of the targeted lamina should be checked. The drill is used in the craniolateral direction from the inferolateral portion of the cranial lamina until the LF is detached. From the superolateral part of the caudal lamina, the bone is made thin in the caudolateral direction and is drilled until the dura is identified. According to the size and height of the pathologic lesion and level, the area of the foraminotomy can be extended to the lateral or craniocaudal side. It is possible to remove one-third to one-half of the medial side of the facet joint. However, if more than 50% of facet joint is removed, there is a substantial risk of instability. After flavectomy, the medial border of the pedicle and the dura and exiting nerve root should be checked. Once the exiting nerve root is identified, foraminal decompression is performed using a 1-mm Kerrison punch. If a protruded disc is visible around the nerve root, it is removed gently. If the workspace is narrow, a pediculectomy can be used to create enough space while reducing nerve root manipulation. Finally, the lateral edge of the pedicle should be checked to ensure appropriate foraminal decompression via the neural foramen using a ball-tip type hook. All surgical procedures should be performed safely to prevent spinal cord injury.
5. Unilateral Biportal Endoscopic Lumbar Interbody Fusion
In contrast to general decompression, it is not recommended to perform laminectomy using a drill during unilateral biportal endoscopic lumbar interbody fusion (ULIF). Local autobone can be collected for bone grafting by laminectomy using a Kerrison punch or osteotome. The inferior articular process is also removed and should be resected in several pieces because it may be difficult to remove through the working portal if it is resected in large pieces. Contralateral facetectomy performed across the base of the spinous process is helpful for spondylolisthesis reduction or correction of a lordotic curve. If the contralateral facet joint osteophyte is larger or to achieve greater reduction or greater lordotic curve in spondylolisthesis, a total facetectomy is performed by additionally making incisions on the contralateral side. These skin incisions are necessary even for percutaneous screw insertion on the contralateral side (Figure 5).
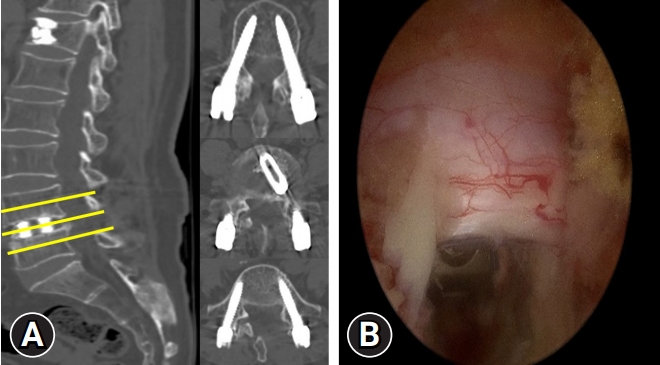
Postoperative sagittal and axial computed tomography images (A) and intraoperative endoscopic images (B). One transforaminal lumbar interbody fusion cage was inserted through the left side only, and percutaneous pedicle screws were inserted through 4 incisions, including 2 portal incisions.
The medial aspect of the SAP should be removed sufficiently to enable interbody cage insertion. If it is not sufficiently removed, excessive neural structure retraction may occur during cage insertion. A space of at least 8 mm from the lateral margin of the thecal sac must be maintained to insert the cage safely. The ipsilateral exiting nerve root should not be fully exposed before cage insertion to protect it during cage insertion. Angled endplate removers and pituitary forceps are used to remove the nucleus pulposus and cartilaginous endplate. Endplate preparation is completed on both the ipsilateral and contralateral sides using an angled endplate remover, which is essential for fusion. It is helpful to use a 30 degrees endoscope for endplate preparation to the contralateral side. During surgery on patients with high-grade spondylolisthesis or significant disc narrowing, the upper edge of the caudal vertebral body is removed with an osteotome to make a larger entry. By magnifying the endoscopic view, surgeons can determine when the endplate preparation is complete. To prevent bone graft loss during cage insertion, continuous irrigation should be paused. Before cage insertion, dilate the paraspinal muscles with a bar dilator to make it easier for cage insertion. Anchor to the caudal vertebral body edge with a specialized root retractor, and insert the cage into the annulotomy site with gelfoam to reduce bone graft loss and bleeding. After cage insertion, a foraminal decompression is performed by removing the foraminal ligament around the exiting nerve root on the ipsilateral and contralateral sides. If good pulsation of the nerve root and thecal sac is identified, it can be regarded as the endpoint of decompression. Perform percutaneous pedicle screw fixation using 2 ipsilateral and contralateral skin incisions. The distance between the exiting nerve root and the traversing nerve root on the ipsilateral side is measured by preoperative MRI. If it is more than 16 mm, a large-sized cage can be safely inserted without neural injury. However, if it is less than 16 mm, a smaller cage may be needed.
Modified ULIF is similar to routine ULIF. A skin incision is slightly more lateral than in routine ULIF and uses 2 short posterior lumbar interbody fusion (PLIF) cages rather than one long transforaminal lumbar interbody fusion cage. Two PLIF cages are inserted into the unilateral laminectomy and facetectomy area. After adequately retracting the dura toward the medial side, the first cage is inserted into the medial or contralateral side. Using the cage pusher, after pressing slightly further to the contralateral side the second cage is inserted into the empty space remaining. A fusion material such as a bone chip is pushed between the 2 cages.
6. Closure and Postoperative Care
During surgical drain insertion, the drain is inserted blindly or under endoscopic guidance. If adequate bleeding control is completed, surgical drain insertion may be skipped. Because maintaining adequate saline flow during the drain insertion is important for the instrumental portal patency, a drain line should be inserted via the instrument rather than the endoscopic portal for a clearer surgical view. Compression around the portal before suturing may help to minimize soft tissue water retention. After the appropriate surgery has been completed, the muscle is approximated and the skin incision is closed with absorbable sutures or a sterile strip. The wound is covered with a sterile dressing, and the patient is sent to the recovery room. Patients are observed in a recovery room for several hours before being moved to a general ward. Provide analgesics as required and encourage patients to walk as soon as possible. Pain usually subsides within 24 to 48 hours.
COMPLICATION AVOIDANCE
1. Postoperative Hematoma
The most common cause of postoperative hematoma is inadequate hemostasis, which leads to an unsatisfactory clinical outcome after surgery. Postoperative hematoma may occur as epidural fibrosis, which can interfere with the expansion of the dural sac [19]. In addition to inadequate hemostasis, other risk factors for postoperative hematoma include sex (female > male), age (>70 years), history of anticoagulation medication, and usage in other preceding studies. It was found that the type of operation and water infusion pump (pressure: 30 mmHg, masking of epidural venous bleeding) had a significant effect [20].
Initial working space, bone bleeding, epidural vessels, and intramuscular bleeding are 4 key factors to consider when preventing postoperative hematoma. First, the possibility of postoperative hematoma is low when the initial working space maintains a clear view. To maintain a clear view, it is necessary to check prompt meticulous bleeding control and fluid output. Maintaining a systolic blood pressure between 90 and 110 mmHg during surgery is also helpful, as increased intra-abdominal pressure leads to increased bleeding. One of the major causes of postoperative hematoma is bone bleeding, which is common in patients with osteoporosis. Bone bleeding seems to be reduced due to hydrostatic pressure, but when the hydrostatic pressure decreases, bone bleeding appears. Therefore, bone wax and an RF probe should be used carefully to control the bleeding. In a previous study comparing UBE and conventional discectomy, a postoperative epidural hematoma was reported in 8.5% of UBE and 1.4% of conventional surgery, which is due to hydrostatic pressure caused by the masking of bleeding [21]. The routine application of bone wax to the spinous process base, cranial and ipsilateral sides is recommended. However, areas where bone work has been performed using an osteotome and Kerrison punch are not flat; therefore, bone wax cannot be applied well in these areas. After flattening with a burr, the application of bone wax can be helpful [22].
RF is used to control bleeding in patients with highly abundant epidural vessels. When controlling bleeding, always create a space between the dura and the epidural vessel and coagulate in the opposite direction with the neural structure at the rear (Figure 6). In focal bleeding, a hook-type RF is used, and in epidural bleeding where the focus is not visible, gelfoam and Gelatin-Thrombin Sealants (Floseal, Baxter Healthcare Corp., Fremont, CA, USA) are used. To control the bleeding that occurs when LF is removed, en bloc should be used. Before removing LF, the margin can be coagulated with RF and then removed with en bloc. Occasionally, if there is bleeding from the endoscope portal rather than bleeding within the surgical field, there may be artery bleeding of the muscle, which should be confirmed and coagulated. When bleeding occurs at the endplate during ULIF, cage insertion is a method to prevent bleeding. If bleeding is so severe as to interfere with the surgery, the endoscope can be advanced as close as possible to the suspected bleeding focus. To find the bleeding focus, the hydrostatic pressure is increased temporarily to wash out and coagulate the bleeding using a small-size RF probe. A drain after surgery is another effective method of preventing postoperative hematoma. If bleeding from the extraforaminal area is not controlled, inserting a drainage catheter into the foraminal space can prevent postoperative hematoma and retroperitoneal hematoma [23] (Supplementary video clip 2).
The neural structure is located on the back of a radiofrequency (RF) device to protect the nerve during coagulation. If RF is used for a long time, the likelihood of nerve damage is increased. Therefore, completing bleeding control in a short time can prevent neural injury.
In a paraspinal approach, hematoma and irrigation fluid may accumulate in the abdominal space after surgery, so the procedure should be performed without using an infusion pump or using a working sheath (Figure 3). In addition, the transverse process should not be removed excessively; hematoma and irrigation fluid will infiltrate the abdominal space if the transverse process is removed more than necessary. In L5/S1, the lower sacral alar is resected instead of the transverse process, and the upper pathologic foraminal ligament should be removed finally to prevent hematoma and irrigation fluid from entering the abdominal cavity. Occasionally, radicular arterial bleeding can cause many difficulties in performing surgery by obscuring the endoscopic visual field due to massive bleeding. The best way to prevent this is to coagulate the small vessels using the RF probe before bleeding occurs.
An important key to preventing bleeding in posterior cervical surgery is the position of the patient. By sloping the upper back downward, the venous return can be decreased. Using this technique can significantly reduce intraoperative bleeding. When the vertebral artery is medially located during cervical foraminotomy, extreme RF power may cause injury to the vertebral artery. Gelfoam or Gelatin-Thrombin Sealants should be used if bleeding occurs during foraminotomy. Since there are many vessels in the periradicular fibrous sheath, it must be removed while coagulating with a hook RF [24]. In cervical surgery, the en bloc removal of LF can help prevent postoperative hematoma, and even if postoperative hematoma occurs, it can be removed under local anesthesia.
2. Dura Tear and Traction Injury
A dura tear is the most common complication (1.9%–8.6%) in UBE and occurs most frequently in the thecal sac, axillar, traversing root [25]. The causes of dura tear are unpracticed handling, lack of understanding about water dynamics, adhesion, massive bleeding (blurred vision), blind procedure, Hemovac-drain tip irritation, repeated damage by a sharply facetectomized site (remaining bone edge), etc. (Supplementary video clip 3). In endoscopic spine surgery, hydrostatic pressure causes central folding, and beginners have a high risk of tearing the dura because the working space is frequently restricted in inexperienced surgery [26]. In addition, dura tears often occur on the dural sleeve, and to solve this problem, the working space should be expanded through sufficient bone work and dura repair should be attempted. A dura tear can occur when experts perform blind techniques carelessly or when additional bone work is performed close to the exposed dura after the LF has been removed. The meningovertebral ligament is responsible for pulling the dura back, so this is not confirmed and there is a high possibility of making a dura tear during the removal of various epidural tissue (Supplementary video clip 4).
In incomplete decompression, the facet joint remains sharp (remaining bone edge), which is the reason for delayed dura tear after surgery. Therefore, the medial facet joint should be wide decompressed and the surface should not be sharpened. Unlike conventional surgery, the Hemovac drain is inserted vertically. Elderly patients may have a dura tear due to thin dura, or drainage catheter withdrawal after imaging because it can cause nerve root compression and cause radiculopathy. When a dura tear occurs, water pressure should be decreased to prevent increased ICP and simple observation with absolute bed rest is recommended for injuries less than 4 mm. For large dura tears of more than 12 mm, conversion to microscopic direct repair is recommended [25,27].
When a dura tear occurs, a surgical clip is used instead of a suture to perform a direct dura repair. In case of excessive tearing, a direct suture and repair are essential. When water and fibrin sealant come into contact, glue immediately becomes ineffective and hardens. Before delivering fibrin sealant, it is recommended that the Hemovac drainage catheter be opened and all irrigation fluid drained [28]. Removing the LF with enbloc rather than with piecemeal helps to reduce dura tears because unnecessary procedures on the dura can be reduced. When performing bone work after removing the entire LF, it is better not to use drilling, but to use a small osteotome or an angled Kerrison punch. A blurred surgical field can cause neural structure injury, so it is important to maintain a clear view of the surgical field, such as active bleeding control, and since the RF probe can cause neural tissue injury, its use should be reduced around the neural structures as much as possible.
CONCLUSION
The field of UBE has achieved remarkable advancements in recent years, and endoscopic techniques have become common essential spinal surgery procedures. This literature review describes essential surgical techniques during UBE, not only for beginners but also for those with established skills.
Notes
Conflicts of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Supplementary Material
Supplementary video clips 1-4 can be found via https://doi.org/10.21182/jmisst.2023.00871
Supplementary video clip 1.
Smooth saline flow created by using working sheaths.
Supplementary video clip 2.
Bleeding control techniques during unilateral biportal endoscopic spinal surgery. Radiofrequency (RF) device, bone wax with or without RF, Gelatin-Thrombin Sealants (Floseal, Baxter Healthcare Corp., Fremont, CA, USA), and Hemovac insertion.
Supplementary video clip 3.
A dura tear caused by using a cutting instrument without sufficient dissection.
Supplementary video clip 4.
The meningovertebral ligament is responsible for pulling the dura back, so meningovertebral ligament is not confirmed and there is a high possibility of tearing the dura during the removal of various epidural tissue.