Nerve Root Herniation With Entrapment After Endoscopic Spine Decompression
Article information
Abstract
Incidental dural tears are common complications of endoscopic lumbar spine surgery. Postoperative nerve root herniation with entrapment is a rare consequence. We report our experience of postoperative nerve root herniation with an incidental dural tear as a cause of sudden sciatic pain. If a dural tear is not amenable to repair using an endoscopic method, open conversion with microscopic duroplasty should be considered as the initial approach given its prognosis. Additionally, if a patient suddenly develops unexplained sciatica after lumbar spine surgery, nerve root herniation with entrapment should be considered in the differential diagnosis.
INTRODUCTION
Incidental dural tear is a common complication of a lumbar spine surgery. It has been reported that the incidence of dural tears is much higher in endoscopic procedures [1]. However, nerve root herniation with entrapment that causes severe radiating pain through incidental dural tear is a relatively rare phenomenon [2]. We report a rare case of nerve root herniation with entrapment as the cause of postoperative sciatica without showing any signs of cerebrospinal fluid (CSF) leakage after endoscopic lumbar spine surgery.
CASE REPORT
A 75-year-old woman presented with neurogenic claudication, experiencing a maximum walking distance of approximately 500 m. Additionally, she reported radiating pain from the buttock region to the lateral thigh on the right side that had been present for the past 6 months. She had previously received several epidural blocks at private clinics but saw no improvement. Physical examination showed mild weakness in ankle dorsiflexion and knee extension. She had a medical history of hypertension and dyslipidemia and underwent microdiscectomy of the L5–S1 level on the right side 4 years ago. Magnetic resonance imaging (MRI) showed lumbar central stenosis at L3–4 and L4–5 levels with L5 lumbarization and stable degenerative spondylolisthesis (Figure 1).
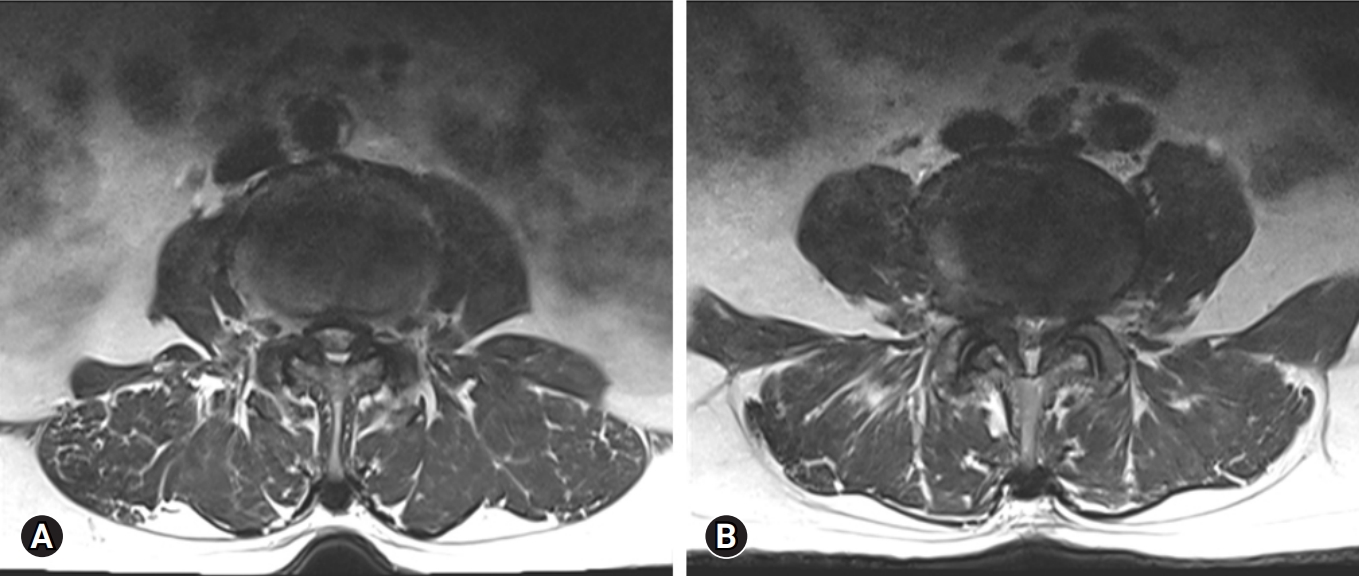
Axial magnetic resonance imaging taken preoperatively, demonstrating central canal stenosis with ligamentum flavum hypertrophy at L3–4 (A) and L4–5 (B).
The patient underwent an endoscopic unilateral laminectomy with bilateral decompression at L3–4 and L4–5 levels using a left-sided approach. The hypertrophied ligamentum flavum at each level was identified and removed. During the operative procedure, dural tearing or CSF leakage was not detected on endoscopic view. Postoperative lumbar MRI showed no evidence of CSF leakage (Figure 2). The patient showed improvement without neurological deficits after the operation. She was discharged in a tolerable state.
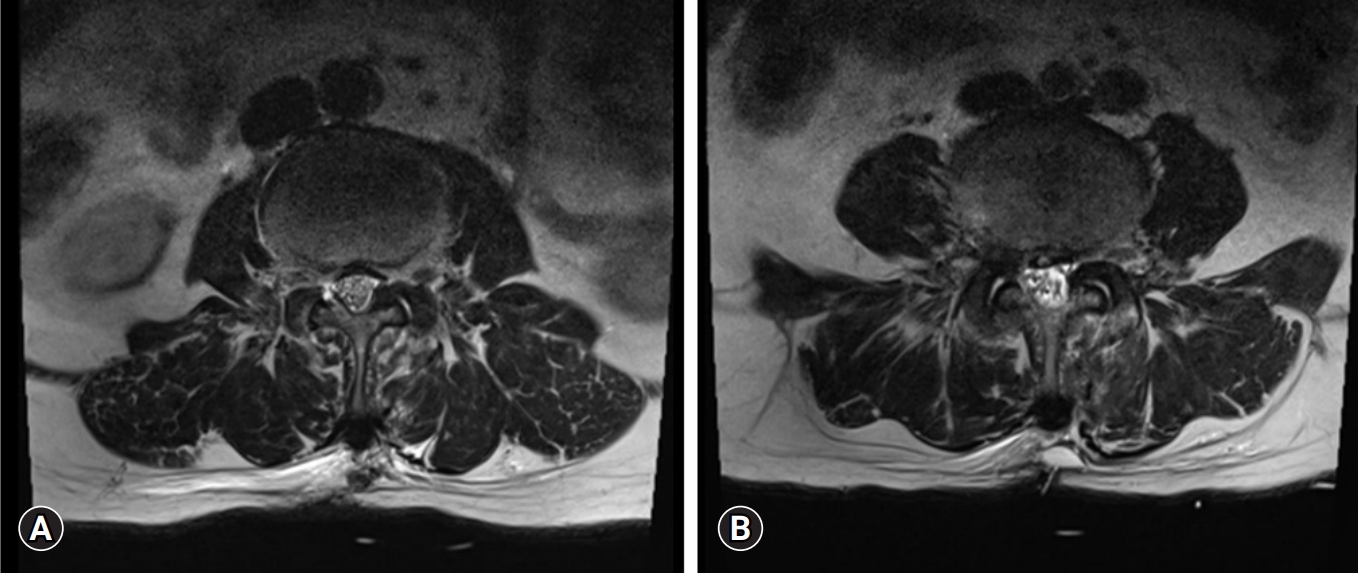
Axial magnetic resonance imaging taken postoperatively, showing a decompressed thecal sac without evidence of cerebrospinal fluid leakage at L3–4 (A) or L4–5 (B).
Seven days after discharge, she experienced a sudden onset of severe sciatica in her right lateral thigh. An MRI revealed a moderate epidural fluid collection at L3–4 and L4–5 levels without evidence of an epidural hematoma (Figure 3). The pain was intractable and unresponsive to any painkillers. Thus, we decided to perform an operative site exploration using an endoscope. During the operation, a dorsal dura tear was observed along with nerve root entrapment at the L3–4 level. We then pushed the herniated nerve root into the thecal sac and patched the dura defect with a fibrin sealant patch (Tachosil, Nycomed, Zurich, Switzerland) (Figure 4). Following the second operation, the patient reported a significant improvement in the preoperative right leg pain.
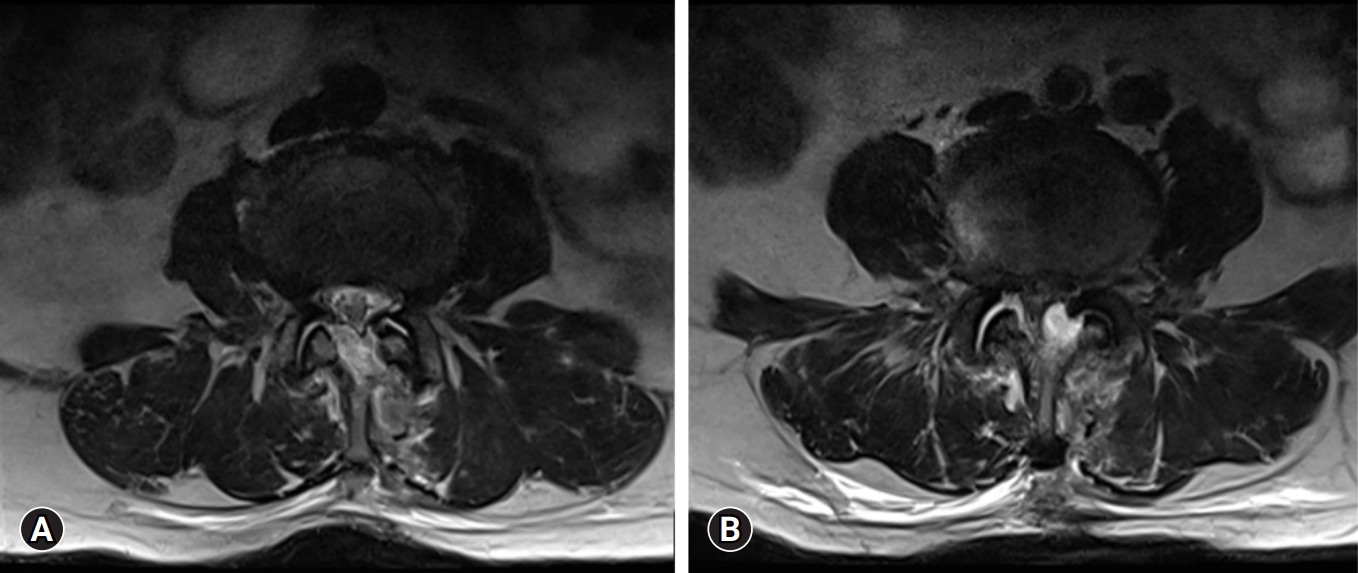
Axial T2 magnetic resonance imaging, showing epidural fluid collection at both L3–4 (A) and L4–5 (B), suspicious for cerebrospinal fluid leakage.
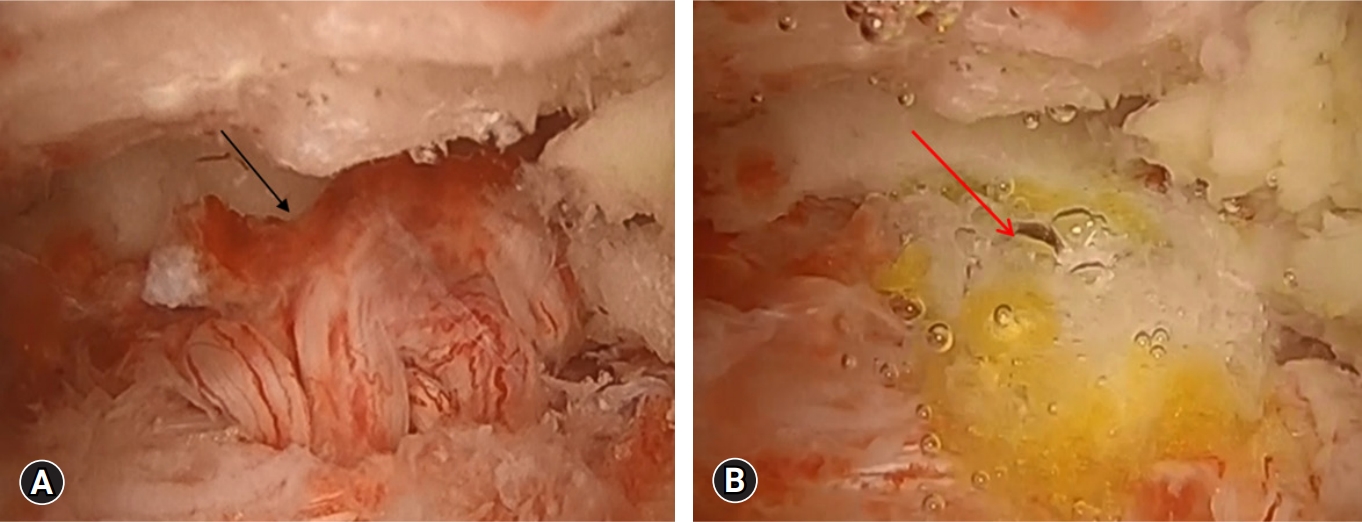
Endoscopic view of the spinal canal. (A) Dura tear with nerve root herniation (black arrow). (B) Tachosil (Nycomed, Zurich, Switzerland) is inserted through the dural defect (red arrow).
Fourteen days after the endoscopic exploration, the patient experienced a sudden onset of sciatic pain throughout her entire right leg. An MRI was performed, which showed recurrent epidural fluid collection at L3–4 and L4–5 levels (Figure 5). Initially, an epidural block was performed. However, it did not result in significant improvement. We suspected that nerve root herniation had recurred. Therefore, a microscopic exploration was necessary. The third operation involved an extended hemilaminectomy at L3. Since a consistent dura tear and nerve root herniation with entrapment were found at the L3–4 level, the entrapped nerve root was repositioned, and a duroplasty was performed via primary closure. Postoperatively, the patient's sciatica was immediately relieved. There was no recurrence during the 6-month follow-up period.
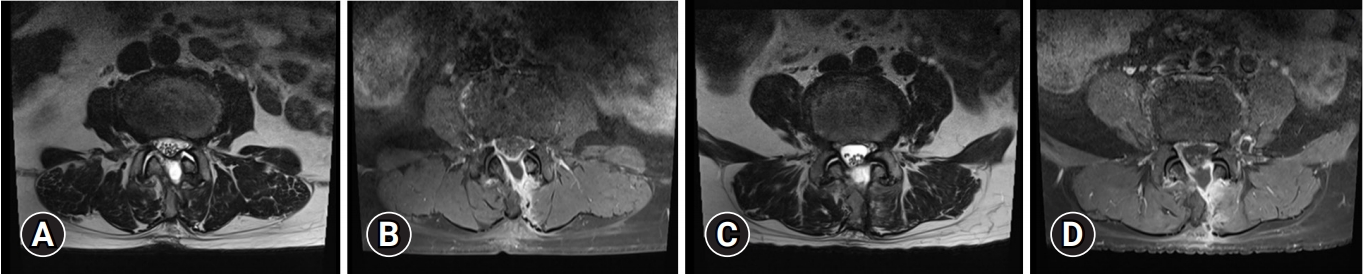
T2 axial (A) and T1 axial contrast-enhanced (B) magnetic resonance imaging at the level of L3–4, and T2 axial (C) and T1 contrast-enhanced axial (D) magnetic resonance imaging at the level of L4–5 showing epidural fluid collection suspicious for cerebrospinal fluid leakage. The nerve root herniation does not seem unclear in these images.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
DISCUSSION
With rapid evolution of surgical techniques and materials, endoscopic spine surgery is already moving toward becoming the standard in the treatment of degenerative pathologies [3]. Since spinal dura includes nerves and CSF with 2 layers (inner and outer membranes), it is prone to tear [4]. Especially when performing an endoscopic spine surgery, endoscopic repair of dura tear is challenging for spine surgeons because of its limited operative field [5]. Several articles have introduced management of dura tear using an autologous muscle graft or fibrin-sealed collagen sponge after endoscopic lumbar surgery including studies of Müller et al. [1] and Oertel and Burkhardt [6].
There are many reasons for recurrence of sciatic pain after a spine decompression surgery. Postoperative epidural hematoma and insufficient decompression are common reasons [7]. However, unrecognized incidental dural tear should be considered for its potential associated symptoms and complications [2]. In case of incidental dural tear during operation, many surgeons usually pay attention to symptoms for intracranial hypotension due to CSF leakage (i.e., postural headache, nausea, and so on). However, a less known complication of such a dural tear represents a postoperative nerve root herniation. In many cases described by several authors, the clinical course of nerve root herniation shows a temporary improvement after surgery and a sudden onset of intractable radiating pain. Popadic et al. [2] have reported a similar case with postoperative nerve root herniation.
When patients experience sudden recurrence of severe radiating pain after decompression surgery, physicians should consider postoperative nerve root herniation with entrapment regardless of the presence of dura tear, as well as postoperative hematoma or nerve compression. Whether dural tear requires surgical treatment during endoscopic spine surgery is still debatable.
Whether dural tear requires surgical treatment is still debatable. Park et al. [7] have reported that when intraoperative dural tearing occurs during endoscopic procedure, size estimation should be performed and dural defect less than 12 mm can be solved by application of fibrin sealant patch. However, dural defect more than 12 mm should be solved with nonpentrating titanium clip or primary suture. As we can see in our case, when large dural defect occurs, it is not feasible to manage the defect with an endoscopic method, with conversion to open-spine surgery being a better option.
CONCLUSION
We report a complicated dural injury case that caused postoperative sciatica. When sudden sciatica recurs after endoscopic spine surgery, unrecognized incidental dural tear followed by postoperative nerve root herniation with entrapment should be considered as well as postoperative hematoma or nerve compression. In such case, open conversion with microscopic duroplasty should be considered first rather than endoscopic procedure considering prognosis.
Notes
Conflicts of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
