Overview and Prevention of Complications During Biportal Endoscopic Cervical Spine Surgery
Article information
Abstract
Purpose
Biportal endoscopic spine surgery is becoming popular for various spinal pathologies, including cervical and thoracic spine diseases. However, the safety of biportal endoscopic cervical spine surgery (BECSS) has not been fully investigated, and inexperienced surgeons can cause serious complications. The study aimed to evaluate the complications of BECSS and identify tips for preventing them through a literature review and retrospective analysis of case series.
Methods
Articles on BECSS were electronically retrieved from multiple databases, with inclusion criteria including controlled and case series designs, detailed reporting of complications and/or reoperations, and the use of BECSS. The study excluded simple review articles and case reports. The clinical data of 45 patients who underwent BECSS at our institution were collected, and information was extracted on demographic features, surgery type, surgical level, surgery-related complications, and reoperations and their reasons.
Results
The study retrieved a total of 67 studies from 5 databases, of which 6 were included after screening. In total, 227 cases of BECSS were identified, and the overall complication rate was 0%–14.3%. Complications included dura tearing, symptom recurrence, incomplete decompression, postoperative epidural hematoma, and transient paralysis. Reoperation was performed in 3 cases.
Conclusion
BECSS has similar complication rates to those of other surgical techniques. It is important to provide extensive education, share knowledge and experience, and conduct further research to minimize complications and improve outcomes for patients, as is the case with other spinal surgical procedures.
INTRODUCTION
Biportal endoscopic spine surgery is rapidly gaining its popularity among spine surgeons all around the world and expanding its application to various spinal pathologies [1]. In the early days, relatively easy and common lumbar decompressive surgery and discectomy were mostly performed, but with the experience of spine surgeons and technical advancements, it is being applied to more challenging and technically demanding cases, such as cervical and thoracic spine diseases [1-3]. However, the safety and efficacy of biportal endoscopic spine surgery in the cervical spine have not yet been fully investigated, and careless attempts by inexperienced and unprepared spine surgeons can cause catastrophic complications. According to our experience, biportal endoscopic cervical spine surgery (BECSS) was not easy at first, even for experienced spine surgeons. It was difficult to determine the exact anatomical orientation and location and achieve complete epidural bleeding control during surgery.
The aim of this study is to evaluate complications of BECSS via available literature reviews and retrospective analysis of our case series. Additionally, the authors aim to identify tips for preventing complications by reviewing literature.
MATERIALS AND METHODS
1. Literature Search
Electronic retrieval of articles from PubMed, Embase, Web of Science, Scopus, and EBSCO was performed to identify scientific studies on BECSS. A full-text search of all studies was performed using the following string: “biportal endoscopic cervical spine surgery.” In addition, all reference lists of the included studies were reviewed to identify potentially relevant articles.
2. Inclusion and Exclusion Criteria of Literatures
The inclusion criteria for this study were as follows: randomized or nonrandomized controlled and case series design, surgical intervention with BECSS, and detailed reporting of complications and/or reoperation. The exclusion criteria were as follows: simple review articles without mentioning specific complications and simple case reports. If several articles were identified from the same institution, the most recent one was included, and the remaining were excluded.
3. Our Case Series
A total of 45 patients underwent BECSS in our institute. With approval from the Institutional Review Board of Yeouido St. Mary’s Hospital, the clinical data of these patients were collected (SC23RISI0042).
4. Data Extraction
The following data were extracted in selected literatures and our cases: (1) demographic features of patients; (2) surgery type; (3) surgical level; (4) surgery-related complications; (5) reoperations and their reasons.
RESULTS
1. Literature Search Results
According to the search criteria, a total of 67 studies were retrieved from 5 databases. After removing duplicates, 35 duplicate studies were excluded. Of the remaining 32 studies, 17 were excluded after the initial title and abstract screening. The full texts of the remaining 15 articles were evaluated in detail, and 9 articles were excluded according to the exclusion criteria. Finally, 6 articles related to complications of BECSS were included in this study. All studies were the retrospective studies, and there was no randomized controlled or prospective study.
2. Clinical Data
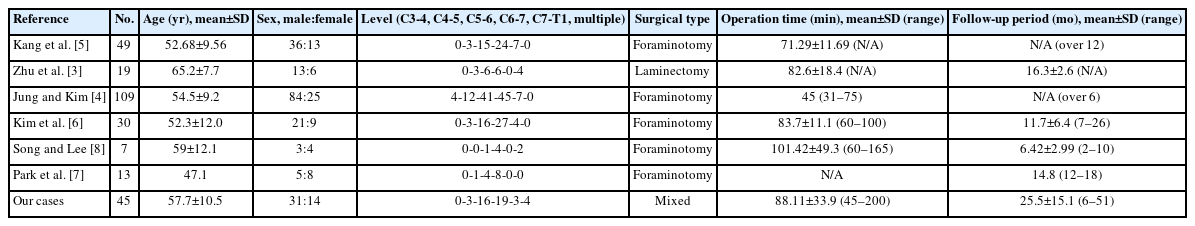
A total of 227 cases of BECSS were identified in 6 articles. Among them, laminectomy for cord decompression was performed in 19 cases and foraminotomy for nerve root decompression was performed in 208 cases. In 157 cases, discectomy was performed during foraminotomy. In our series, laminectomy for cord decompression was performed in a case, and foraminotomy was performed in the remaining 44 cases. Among the patients who underwent foraminotomy, 21 cases underwent discectomy. The demographic data of the patients are summarized in Table 1.
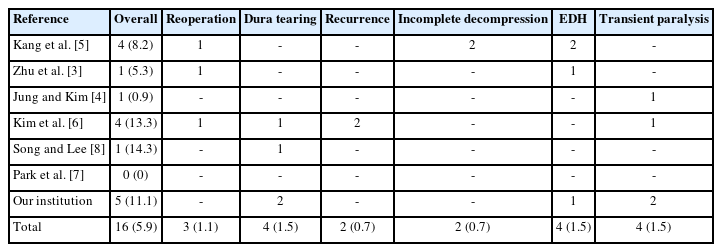
3. Complications
Among 272 cases of BECSS in previous articles and our cases, 16 complications were reported, thus the overall complication rate was 5.9%. The types of complications reported in previous articles and our cases were dura tearing, symptom recurrence, incomplete decompression, postoperative epidural hematoma, and transient paralysis. As a result, reoperation was performed in 3 cases due to incomplete decompression, symptom recurrence and symptomatic postoperative epidural hematoma (Table 2).
DISCUSSION
Currently, when searching the literature, BECSS is performed only with a posterior approach and decompression [3-8]. Similar minimally invasive techniques included the microscopic surgery and the full-endoscopic surgery [6,9,10]. Complications of these surgical techniques are well known via previous articles. Wu et al. [9] reported a complication rate of 0%–18.2% in the full-endoscopic surgery, and reported complication types such as dural tear, transient root palsy, and wound infection. In another article, reported complications included paresthesia, transient motor weakness, palsy, superficial wound infection, postoperative hematoma, and dura tear. And, the complication rate of full-endoscopic surgery was reported to be lower than that of anterior cervical discectomy and fusion [11]. Even in minimally invasive microscopic surgery, a complication rate of 0%–14.3% has been reported, and types of complications were reported as symptom recurrence, paresthesia, and wound infection [10]. Compared with other surgical techniques, the overall complications of BECSS are thought to be similar. Kim et al. [6] directly compared these 3 techniques, and reported that there was no significant difference in frequency or type of complications.
There are several causes of neurological deficit such as hypesthesia, paresthesia or paralysis after the endoscopic spine surgery. It may be a 'normal' postoperative change resulting from revascularization of decompressed nerves [12,13]. However, these symptoms do not last very long. Therefore, reimaging is warranted if these symptoms persist for more than 72 hours [14]. There were some reports that these neurological deficits are related to thermal injury that occurred during surgery [9,15]. To prevent this, care must be taken during coagulation around the nerve [14]. In addition, direct contusion on the nerve during surgery can also cause these neurological deficits, so careful manipulation is always needed [14]. Unlike lumbar spine, there was a very rare case report in which paralysis occurred due to spinal cord injury during endoscopic cervical spine surgery [15]. If excessive force is used in the process of inserting a dilator or tubular retractor, shock can be caused between the lamina. Therefore, when inserting a dilator or tubular retractor, be sure to incise the fascia and perform blunt dissection so as not to apply excessive force [14].
To prevent incomplete decompression during foraminotomy, after sufficient drilling bone, the ligament flavum must be sufficiently removed before disectomy [14]. Similar to other surgical techniques, dura tearing occurs often, but there is no clear way to prevent it [9,16]. In endoscopic spine surgery, dura tearing is usually a small punctate lesion, and it is recommended to use sealants such as fibrin glue [14,16,17]. On the other hand, large dura tearing that causes symptoms requires repairing dura, which usually requires a change into the open surgery [16,17]. However, since there were several technical reports on how to repair dura under the endoscopic environment, it would be necessary to apply it depending on the situation [16-18].
There is a lot of interest in long-term complications such as cervical kyphosis and segmental instability after cervical posterior approach surgery [14,19]. However, nothing has been confirmed about BECSS. Therefore, it is thought that long-term follow-up data will be needed in the future. Maintaining a facet joint of 50% or more, a well-known technique to prevent cervical spine instability, will be important in preventing such complication [14,20].
There are several limitations to this article. Following review only 6 studies were included that met inclusion/exclusion criteria. And, relatively short follow-up time and small cohort size were additionally limited. In order to determine more accurate and specific complications of BECSS and to prevent them, continuously large and prospective research will be needed in the future.
CONCLUSION
Complications of BECSS did not show a significant difference compared to other surgical techniques. In order to prevent these complications as much as possible, extensive education and sharing of knowledge and experience will be required, as in other spinal surgeries. And, a lot of research by all endoscopic spine surgeons will be needed to present good results to patients.
Notes
Conflicts of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.