Essential Surgical Techniques During Fully Endoscopic Spine Surgery: A Historical Review and Future Perspectives
Article information
Abstract
Full-endoscopic spine surgery (FESS) offers minimally invasive techniques for treating spinal lesions with smaller incisions, leading to reduced tissue damage and consequently more rapid patient recovery. The essential techniques in FESS—namely, the transforaminal and interlaminar approaches—have evolved with technological advances in endoscopic systems and surgeon expertise. The transforaminal approach consists of “inside-out” and “outside-in” techniques that have distinct applications depending on the patient’s condition. The interlaminar approach, similar to traditional spinal surgery techniques, is gaining wider acceptance due to its efficacy in addressing unique anatomical challenges. Advanced procedures, such as endoscopic laminectomy and interbody fusion surgery, coupled with navigation systems, have broadened the scope of endoscopic spine surgery, making it an increasingly vital tool in modern spinal surgery.
INTRODUCTION
Modern society has been characterized by an increasingly aging population and a more complex lifestyle. Thus, the quality of life has become of paramount importance. The invasiveness and efficiency of treatments have become primary issues for patients with degenerative spinal diseases.
Minimally invasive spine surgery (MISS) has become a central concept in spinal procedures. Axial pain with radiculopathy is one of the prime reasons patients opt for extensive or radical treatment. Conventional surgical treatment options for spinal disc disease or stenosis include open spinal decompression with or without fusion surgery. However, perioperative morbidities and prolonged recovery duration have emphasized the need for MISS [1,2]. The goal is to minimize normal tissue injury during the surgical approach while providing the relevant therapeutic effect. Owing to MISS, the patient can return to ordinary life earlier with less adverse impact and maintain a high quality of life.
Endoscopic technology in spine surgery may provide a muscle-preserving, percutaneous approach rather than wide-open surgical exposure [3,4]. It may also give an excellent and selective visualization of the pathology. In this viewpoint, endoscopic spine surgery can utilize the essential concept of MISS.
This review aims to describe the essential techniques of current full-endoscopic spine surgery (FESS) and to discuss the benefits, limitations, and future perspectives of this MISS technique.
AN INTRODUCTION TO FESS
FESS has revolutionized the field of spine surgery, introducing a new approach that utilizes an endoscope equipped with advanced features like a 20°–30° rod-lens camera system, a light source, a working channel, and an irrigation channel. This endoscopic procedure is typically characterized by the following [5,6]: (1) use of a working channel endoscope with the working channel and the optics in the same tubular device; (2) complete percutaneous approach with a stab skin incision, and (3) utilization of a monoportal approach with continuous saline irrigation. The endoscopic approach offers several advantages over traditional open surgery by removing the need for additional incisions or traditional surgical pathways. The central premise of FESS is that it enables the surgeon to access and remove targeted lesions using minimally invasive techniques.
Key benefits of FESS include smaller incision sites and reduced tissue damage, contributing to a less traumatic surgical experience for patients. Studies have shown that patients undergoing FESS typically experience less blood loss during the procedure, translating into less postoperative pain and quicker recovery times. These positive patient outcomes mean that patients are generally able to leave the hospital sooner and resume their daily activities more quickly, reducing the overall impact of surgery on their lives [7-10].
And, the direct visualization provided by the endoscope offers a significant advantage in protecting the surrounding tissues and spinal structures during surgery. This improved visibility reduces the risk of inadvertent damage to the surrounding tissue, lowering the overall risk of complications and improving the chances of a successful surgical outcome. This critical benefit is driving an increase in the use of endoscopic surgical techniques in clinical practice, further advancing the field of spine surgery.
The main techniques of FESS have developed over time with the development of camera lenses that provide a better view, the development of rimers and electronic drills that enable active bone work, and the experiences of spinal surgeons.
EVOLUTION OF FESS TECHNIQUES
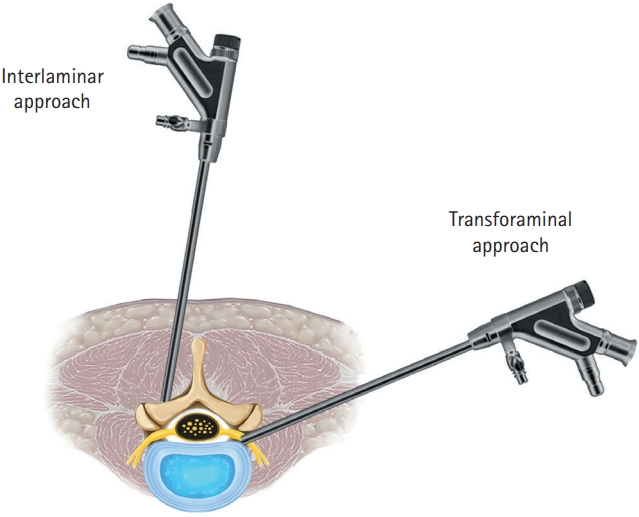
Since its introduction in the 1970s, FESS has evolved significantly, thanks to advancements in science, technology, and the collective experience of spine surgeons worldwide. This continuous evolution and refinement of the procedure have led to the development of 2 primary surgical approaches: the transforaminal approach and the interlaminar approach (Figure 1).
TRANSFORAMINAL APPROACH AND ITS EVOLUTION
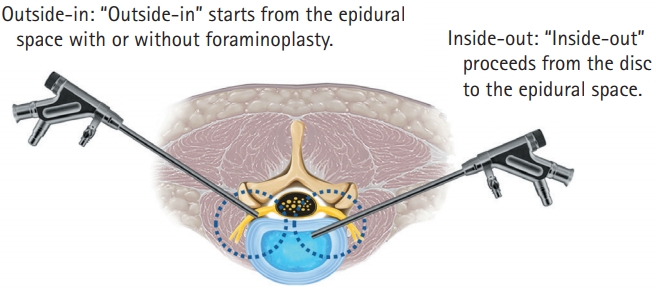
The Transforaminal approach in FESS can be technically divided into 2 main techniques: the 'inside-out' and the 'outside-in' methods. While the distinction between these 2 methods driven by the initial placement of the endoscopic working cannula either inside the intervertebral disc (inside-out) or into the neuroforamen (outside-in) seems somewhat trivial on the surface [11].
The transforaminal approach was pioneered by Kambin and Sampson [4] and Hijikata [3], who independently performed discectomies for contained disc conditions using fluoroscopy guidance. The transforaminal approach during spinal endoscopic surgery was inherently an inside-out technique through a “triangular safe zone.” The inside-out technique begins with the insertion of an endoscope into the disc space. The surgeon then removes a part of the nucleus pulposus and related tissues, effectively decompressing the tissues pressing on the nerve [12].
In the early days of spinal endoscopic surgery, the inside-out technique of the transforaminal approach was preferred due to its simplicity and the fact that it did not require the use of complex tools like drills or radiofrequency (RF) devices. Early endoscopic systems had limited visualization capabilities, typically providing less clarity and a narrower field of view than the more advanced systems available today.
As technology improved, so too did the capabilities of the endoscopic systems used in spinal surgery. Developments in camera lens technology allowed for more precise visualization, making it possible to use a range of instruments, including various rimer and electronic drills, to access and treat spinal lesions directly. This gave rise to the outside-in technique, which starts outside the foramen in the epidural space [13].
OUTSIDE-IN TECHNIQUE
The outside-in technique is an evolution of the transforaminal approach that allows for less damage to the disc annulus while providing better access for the removal of uncontained discs. Unlike the inside-out technique, the outside-in method may maintain the integrity of the disc annulus and improves the removal of uncontained discs. However, it often necessitates additional bone work, such as foraminoplasty, to create sufficient space for the surgeon to access and treat the spinal lesion directly.
The 'outside-in' technique in FESS is particularly beneficial when the neural foramen itself is a lesion or when the intervertebral disc height is narrow. It provides improved access and visibility, allowing surgeons to effectively address these challenging conditions. Conversely, for younger patients or those with a wide neural foramen, the 'inside-out' technique might be preferable. Performing foraminoplasty in such cases may require additional time and could introduce unnecessary risks. Therefore, the 'inside-out' technique, which is less invasive and less complex, may be sufficient in these situations. The choice between these 2 techniques highlights the importance of individualized surgical planning based on the patient's specific condition and anatomy.
Currently, the 2 techniques have different strengths and weaknesses, and are appropriately selected according to the patient's condition and pathology environment (Figure 2).
INTERLAMINAR APPROACH: ADOPTING TRADITIONAL SPINAL SURGERY TECHNIQUE
In transforaminal approach, for certain areas of the spine, such as the L5/S1 level, which present unique anatomical challenges, the interlaminar approach could be a highly effective strategy. This region of the spine is often problematic for surgeons due to its high iliac crest, small intertransverse space, and relatively narrow foramen, which collectively can limit surgical access [14,15].
The interlaminar approach addresses these challenges by allowing the surgeon to enter the spine between the laminae. This space is typically larger than other spaces in the spine, offering a less obstructed pathway for the insertion of the endoscope and surgical instruments. Importantly, this approach aims to minimize trauma to the surrounding structures and tissues as it doesn't require bone removal, making it a less invasive procedure... [16,17].
As medical technology continues to advance, the interlaminar approach has seen substantial enhancements. Developments in endoscopic equipment, including more sophisticated scopes, drill systems, and RF devices, have greatly improved the versatility and efficacy of this technique.
One significant advantage of the interlaminar approach is its familiarity to spinal surgeons. Many surgeons have been trained in traditional open or microscope-assisted surgery techniques, which share similarities with the interlaminar approach. This familiarity can ease the transition for surgeons moving to endoscopic procedures, thereby facilitating wider adoption of these techniques in clinical practice.
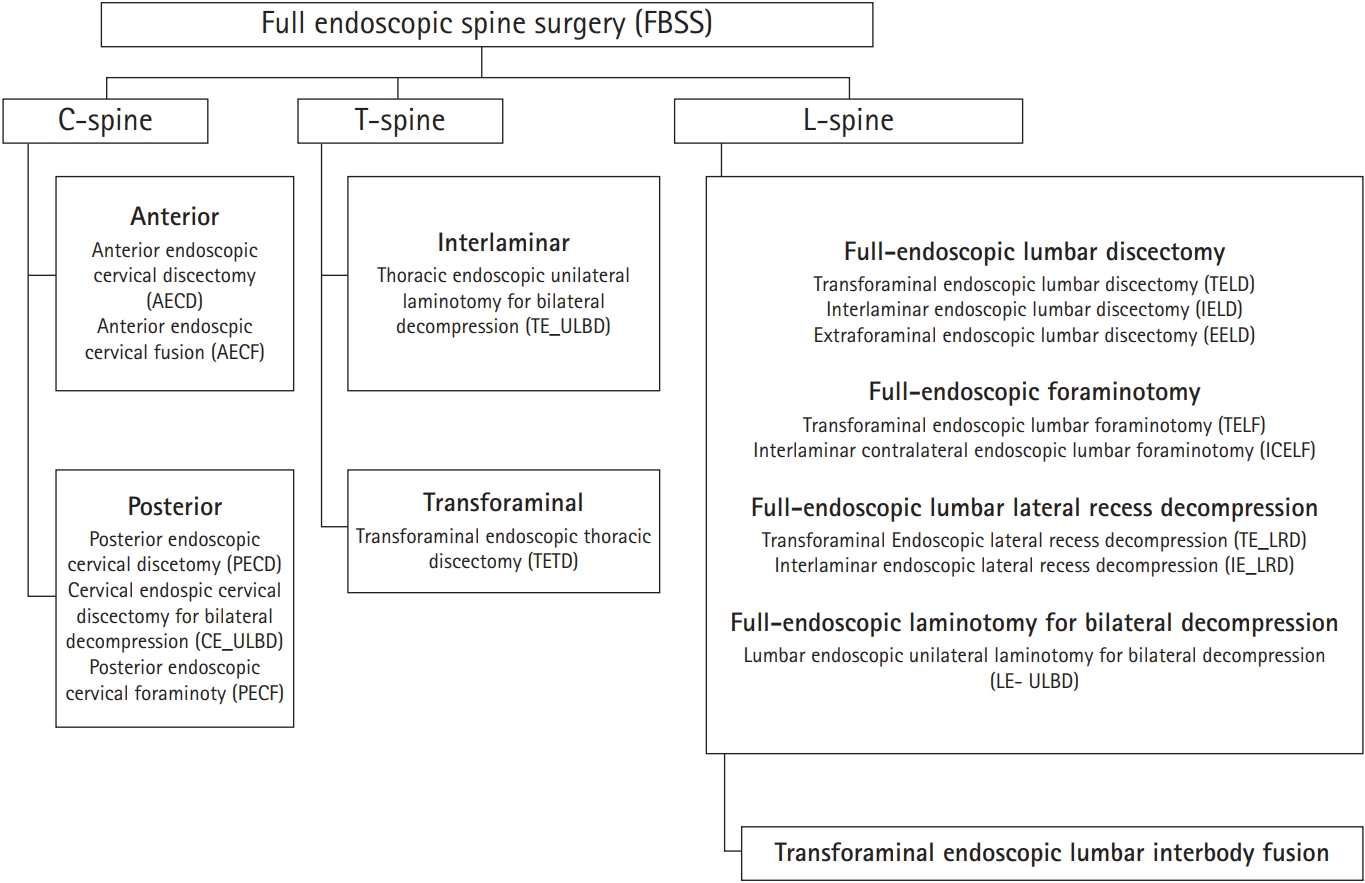
As the interlaminar approach has become more widely used in endoscopic spine surgery, the surgical approach corridors, or the paths surgeons take to access the spinal column, have indeed become more diverse. Various endoscopic procedures are adopted in Figure 3 [18].
Through the interlaminar approach, endoscopic surgery has been included as an indication for effective treatment of spinal stenosis.
In addition, advancements in surgical technology have enabled the application of the interlaminar approach beyond the lumbar spine. It can now be used in cervical and thoracic spine surgeries as well, broadening the range of spinal conditions that can be treated using this minimally invasive method.
EXPANDING THE HORIZONS: ADVANCED TECHNIQUES IN FESS
Over time, as surgeons' expertise in endoscopic spine surgery has grown, a broader range of procedures have been developed. These include complex procedures like endoscopic laminectomy, which decompresses the spinal cord and is performed in the cervical and thoracic regions [19-21].
Moreover, advancements in technology have made endoscopic interbody fusion surgery for the lumbar spine increasingly viable and more common. With these advancements, it's now possible to target the lesion more precisely during surgery, leading to more successful procedures with less tissue damage.
Notably, the development of sophisticated navigation systems has been crucial in this regard. These systems allow surgeons to precisely target the area to be treated during surgery, contributing to safer procedures and better patient outcomes. As a result, these advancements have greatly expanded the scope of endoscopic spine surgery, making it an increasingly important tool in modern spinal surgery.
Notes
Conflicts of Interest
The authors have nothing to disclose.
Funding/Support
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (no. 2021R1F1A1063590).