A Narrative Review of Biportal Endoscopic Spine Surgery in the Cervical and Thoracic Spine: Insights into Its Capabilities, Limitations, and Possibilities
Article information
Abstract
Biportal spinal endoscopy has been successfully utilized for the surgical treatment of common spinal conditions, mainly in the lumbar spine. Surgeons recently have translated this technique to the cervical and thoracic spine. Little is known regarding the clinical effectiveness and safety profile of the biportal endoscopic technique in the cervical and thoracic spine. This is a narrative review of the applications of biportal spinal endoscopy in the cervical and thoracic spine, discussing its current capabilities, limitations, and possible future applications.
INTRODUCTION
Biportal spinal endoscopy is an emerging minimally invasive technique in spine surgery with mounting evidence of clinical effectiveness and safety, mainly in the lumbar spine [1-4]. Biportal spinal endoscopy utilizes a water-based endoscope that is separated from the surgical instruments, in contrast to full endoscopy (uniportal), which incorporates the camera with the working channel altogether. Both techniques incorporate water-based irrigation systems that allow for enhanced visualization using endoscopic cameras. However, by separating the endoscope from the surgical instruments through separate incisions, the biportal technique allows for greater freedom and flexibility, allowing for greater applicability in the spine.
The potential benefit of the biportal endoscopic technique includes reducing the soft tissue trauma from surgical dissection, thereby improving postoperative pain and recovery, and optimizing visualization of the surgical anatomy to reduce iatrogenic injury to the spinal and neural structures. This safety aspect is extremely important given the potential risk to the spinal cord in the cervical and thoracic spine. Thus far, the biportal technique has been applied to posterior cervical and thoracic approaches for treatment of cervical disc herniations, foraminal stenosis, cervical central stenosis, cervical extradural cysts, and calcified thoracic ligamentum flavum causing spinal cord compression. We will provide a narrative review of the application of the biportal technique to the cervical and thoracic spine and consider the inherent capabilities and limitations and discuss the possible applications of the technique.
CERVICAL DISC HERNIATION AND FORAMINAL STENOSIS
Cervical disc herniations and foraminal stenosis can be successfully treated in a myriad of different ways from anterior cervical discectomy and fusion (ACDF), cervical disc replacement (CDR), and posterior laminoforaminotomy with discectomy. Posterior laminoforaminotomy can be successfully performed using the biportal endoscopic technique without the complete removal of the intervertebral disc that would be required with ACDF and CDR. Much of the available studies on biportal endoscopy in the cervical spine is centered on cervical disc herniations and foraminal stenosis, likely due to the relative safety of the technique given the anatomic location of disc herniations and foraminal stenosis.
Park et al. [5] published one of the earliest reports of utilizing the biportal endoscopic technique for cervical disc herniations in 2017. The authors described the short-term results of 13 patients with mean follow up of 14.8 months. In this study, clinical outcome scores improved significantly with Visual Analog Score (VAS) neck, VAS upper arm, and Neck Disability Index (NDI) scores (p<0.05), using biportal endoscopy for cervical discectomies (Table 1). The authors commented that the procedure may be an alternative procedure for the treatment of cervical disc herniations but larger studies with longer follow-up was required.
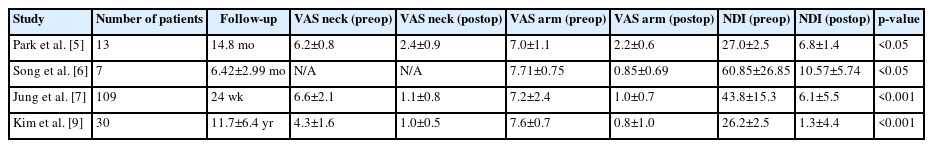
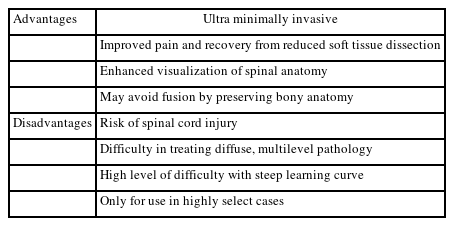
Summary of the published studies depicting the clinical outcomes of biportal spinal endoscopy for cervical disc herniations and foraminal stenosis
A technical note was published by Song and Lee [6] with preliminary results of 7 patients who underwent biportal endoscopic posterior cervical inclinatory foraminotomy for cervical radiculopathy. The authors utilized the technique of posterior cervical inclinatory foraminotomy to preserve the facet joint and prevent iatrogenic instability. The diagnoses included cervical disc herniation as well as foraminal stenosis. The mean follow-up was short at 6.42±2.99 months. Postoperative MRI and CT scans demonstrated successful removal of disc herniations and neural decompression in all the treated segments without any significant change in the cervical alignment, segmental dynamic angle, or disc space height. VAS scores and NDI scores improved significantly from preoperative visit to the final follow-up visit, p<0.05 (Table 1). There was 1 dural tear that was successfully treated with gelfoam and fibrin sealant patch and no instances of neurological complications including dysesthesia or motor weakness in their small series (Table 2).
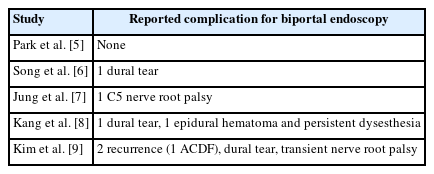
Summary of the published studies depicting the complication profiles of biportal spinal endoscopy for cervical disc herniation and foraminal stenosis
Jung and Kim [7] published the largest case series to date of utilizing biportal spinal endoscopy for single level cervical disc herniations. Their study included 109 consecutive patients, 84 males and 25 females with mean age of 54.5 years. C5-6 and C6-7 were the most common operated levels (n=41, n=45, respectively). Clinical follow-up was performed up to 24 weeks post-operatively and clinical outcome scores improved significantly (Table 1). Patient satisfaction using the Macnab criteria was 86.2% “good to excellent” at 24 weeks after surgery. There were no major complications other than 1 case of C5 nerve root palsy with longitudinal fluid retention in the dorsal epidural space on the postoperative MRI (Table 2). The palsy improved over 4 weeks with conservative management. There were no recurrences or reoperations during the follow-up period. The authors commented on the favorable outcomes with few complications, but the procedure is challenging to master due to the steep learning curve.
The study with the longest follow-up to date was published by Kang et al. [8] who performed a retrospective review of 65 consecutive patients with cervical foraminal stenosis causing cervical radiculopathy with 1 year follow-up. In addition, the authors compared the results of full endoscopy to biportal endoscopy with 32 patients undergoing full endoscopy versus 33 patients with biportal endoscopy. All patients in the study had significant improvement of VAS neck and arm scores as well as NDI scores, and no difference of clinical outcomes scores between the 2 endoscopic techniques. Patient satisfaction using the modified Macnab criteria was good to excellent in 91.7% of patients in the full endoscopy cohort versus 87.9% in the biportal cohort.
One case in each cohort required reoperation due to incomplete decompression with the patient who underwent full endoscopy revised to ACDF and the biportal patient revised with another biportal procedure. There was one case of incidental durotomy in each cohort and one case with C5 nerve root palsy in the full endoscopy cohort (Table 2). There was one case of epidural hematoma as well as persistent dysesthesia in the biportal cohort (Table 2). These patients improved with conservative management. The authors concluded that both endoscopic techniques were successful in clinical outcomes and relatively safe with low complication rates.
Another comparative study was published by Kim et al. [9] who compared radiologic and clinical outcomes for full endoscopy, biportal endoscopy, and microsurgery for posterior cervical foraminotomy for foraminal stenosis. Clinical outcome scores improved significantly in the biportal group from preoperative to final follow-up (Table 1). The authors found that the biportal technique had a low complication profile that was comparable to the other techniques (Table 2).
The safety of the posterior laminoforaminotomy for treatment of cervical disc herniations and cervical foraminal stenosis is favorable from these studies given the location of the compressive lesions away from the central spinal canal and spinal cord and closer to the foramen and nerve root. Thus far in the literature, this is the ideal indication for biportal endoscopy in the cervical spine.
CERVICAL CENTRAL STENOSIS
Only a few case reports have been published thus far in the scientific literature on performing biportal endoscopy for decompression of cervical central stenosis. Typically, cervical stenosis causing spinal cord compression is treated with ACDF, anterior cervical corpectomy and fusion, cervical laminectomy and fusion or cervical laminoplasty. The posterior approaches with cervical laminectomy and fusion and cervical laminoplasty are associated with significant neck pain and disability in open surgery due to posterior cervical muscle stripping and dissection with retraction of the musculature that is required for visualization. Biportal endoscopy may provide a minimally invasive option to decompress the spinal cord while preserving the posterior cervical musculoligamentous structures, potentially reducing post-operative pain and disability. However, there are significant safety concerns with this technique due to risks to the spinal cord especially in the setting of pre-existing spinal cord compression.
A description of the biportal technique for unilateral laminotomy and bilateral decompression for the treatment of cervical spondylotic myelopathy was published by Kim et al. [10]. The authors presented a case of C5-6, C6-7 central stenosis with compression of the spinal cord due to ligamentum flavum hypertrophy and disc protrusions seen on MRI. CT imaging demonstrated ossification of the posterior longitudinal ligament at C5-6. Unilateral laminotomy and bilateral decompression was performed at C5-6 and C6-7 to decompress the spinal cord at these levels. The patient improved with motor weakness and radiating pain in the bilateral upper extremities and postoperative MRI demonstrated complete decompression of the central canal. The authors commented that this technique can be used in highly selective cases of cervical stenosis with myelopathy due to hypertrophied ligamentum flavum, cervical stenosis with concomitant foraminal stenosis, and cervical stenosis with OPLL. They reserved the technique to select patients who are poor candidates to conventional surgeries due to medical conditions since the surgery is technically difficult with a steep learning curve, as well as the risk for spinal cord injury. The authors recommended en-bloc resection of the lamina and ligamentum flavum to reduce the risk of spinal cord injury.
Zhu et al. [11] published a technical note on adding a third portal for biportal endoscopic decompression for cervical spondylotic myelopathy (CSM). The purpose of the third portal was to assist the decompression of the contralateral side of the spinal canal. The biportal technique was utilized on the ipsilateral side while the third portal was placed on the contralateral side. After completing the decompression on the ipsilateral side, the endoscopic camera and the radiofrequency probe were taken to the contralateral side through the interspinous ligament. The third portal was then utilized to perform the decompression on the contralateral side.
The study cohort consisted of 6 patients with single level cervical stenosis causing CSM with mean follow-up of 6.2±3.3 months. Postoperative MRI demonstrated complete decompression in all cases. There was one case of transient hypoesthesia of the contralateral hand that resolved over time. The mean Japanese Orthopaedic Association (JOA) score improved from 7.5±3.8 preoperatively to 12.1±5.2 at the final follow-up (p>0.05). All 6 patients reported excellent satisfaction based on the modified Macnab criteria. The authors purport that the use of the third portal makes the procedure easier and safer to decompress the contralateral spinal canal.
Zhu et al. [12] also published a case report of performing bilateral biportal endoscopic open door laminoplasty that was stabilized with suture anchors. Biportal endoscopy was performed on one side for placement of the suture anchors and the creating the partial laminoplasty trough for the hinge side. Suture anchors were placed at the center of the lateral mass and spinous process at C4, C5, and C6. Biportal endoscopy was then performed on the contralateral side to create the full laminoplasty trough and to raise the lamina. The endoscopic equipment was then passed over the lamina through the interspinous ligament to the hinge side and a third portal was utilized to secure the suture anchors. Postoperative CT and MRI were performed to verify enlargement of the cervical canal and complete decompression. JOA and NDI scores improved clinically from the authors’ report.
In addition to the biportal endoscopic laminoplasty with suture anchors, Zhu et al. [13] described using biportal endoscopy to perform unilateral biportal endoscopic laminectomy with lateral mass screw fixation in a case report. After biportal endoscopic exposure of the left laminae of C4, C5, and C6, separate portals for the right side were made to expose the lamina and lateral masses on the right side. The start point for the lateral mass screws were identified with a 2-mm diamond burr and fluoroscopy, then two 3.5-mm polyaxial screws were inserted through the screw portals. After screw placement, a rod and set screws were placed into the lateral mass screws. At this point, the remnant spinous processes were removed with a grinding drill and the laminae were thinned down to the ventral cortex, which was removed with a 1-mm Kerrison rongeur. Postoperative CT and MRI imaging verified correct placement of the implants and complete decompression at C4-5. The patient had significant improvement of the numbness and gait dysfunction post-operatively. The authors recommended that surgery should be converted to open procedure if the endoscopic visualization or screw trajectory became difficult.
The biportal endoscopic technique can also be used for removal of cervical extradural cysts causing cervical central stenosis. Kim et al. [14] presented 2 cases of using biportal endoscopy to address weakness and cervical radiculopathy from intraspinal, extradural cysts compressing the spinal cord and cervical nerve roots. After placement of the biportal endoscopic equipment and exposing the lamina, a laminotomy was performed with an endoscopic diamond drill. The drilling proceeded until there was free epidural space surrounding the cyst. The ligamentum flavum was carefully dissected off the cyst and the cyst were carefully dissected off the dura to be removed en bloc. Postoperatively, the neurological deficits and symptoms of cervical myeloradiculopathy improved with no recurrence of symptoms at 10–12 months post-operatively. Postoperative MRI and CT demonstrated complete removal of the cyst and decompression of the spinal cord. The authors contended that the endoscopic camera under continuous irrigation provides a clear magnified surgical view that enabled them to manipulate the anatomy to remove the cyst successfully and safely. They acknowledged that the steep learning curve is an impediment to widespread implementation of the technique and the technique should be reserved for select patients with experienced surgeons only.
THORACIC STENOSIS
Little has been published in the use of biportal endoscopy for thoracic stenosis. The earliest study of utilizing biportal endoscopy in the thoracic spine was published by Osman et al. [15] in 2012 and was a case series of 15 consecutive patients with symptomatic thoracic disc herniations. He described the use of arthroscopic equipment to triangulate into the posterolateral aspect of the thoracic disc through the foramen from the lateral to medial direction. After exposure of the posterolateral annulus, an annulotomy was performed under endoscopic visualization and a discectomy is performed with decompression of the epidural space. The authors then described placement of bicortico-cancellous bone dowels from the iliac crest into the disc space for thoracic interbody fusion. The VAS back score improved significantly and 11 out of 15 patients were satisfied with their quality of life post-operatively as compared to 1 patient preoperatively. Postoperative CT scans demonstrated successful fusion in all patients and there were no complications in this study. The hospital costs averaged $8,208.20 as compared to $15,849.69 for thoracotomy surgery. The authors contended that this biportal technique is less invasive, cost-effective, and clinically effective method to address thoracic disc herniation.
Other applications of biportal endoscopy in the thoracic spine include resection of ossified ligamentum flavum (OLF) causing spinal cord compression. Kang et al. [16] published a technical report and described the technique for unilateral laminotomy with an endoscopic drill with a diamond head tip. Once the laminotomy was complete and the dura was exposed, the boundaries of the OLF were identified. The drill was utilized to make a paper-think plate of the OLF in contact with the dura and the adhesions were released with a small nerve probe. The remnant of the OLF was then resected and confirmed by pulsation of the dura. The authors recommended that the biportal technique be utilized only in select patients depending on the morphology of the OLF. Certain large types may require open laminectomy and dural reconstruction depending on the size and characteristics of the OLF.
The largest case series on the use of biportal endoscopy for the treatment of OLF was published by Deng et al. [17], who compared the biportal cohort with open surgery. The biportal cohort consisted of 14 patients for a mean follow-up of 15.4 months vs the open cohort, which had 45 patients and a mean follow-up of 37 months. Surgical time and hospital stays were significantly less with the biportal cohort as compared to the open cohort with significant improvements in clinical outcomes scores, p<0.001 (Table 3). Postoperative CT and MRI showed decompression of spinal cord and complete resection of OLF lesions. There was no neurological deterioration seen in the biportal cohort at the one-year follow-up. The authors found that the biportal cohort had few complications but had 2 cases of headache and neck and back pain, which may be due to excessive epidural pressure from the endoscopic irrigation. These authors also excluded large OLF types from the biportal cohort, shifting bias against the open cohort as more difficult and complex cases were completed open while the smaller lesions were addressed with the biportal technique. Nevertheless, the authors contended that the biportal technique is safe and effective for the treating OLF in the thoracic spine.
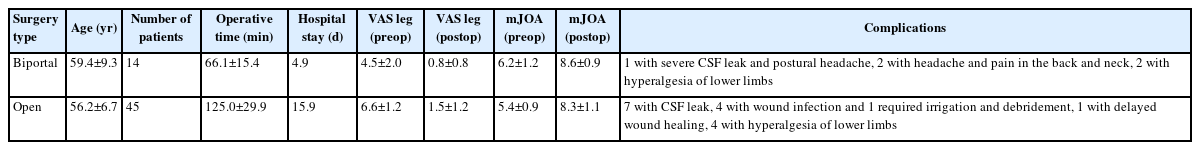
Summary of the clinical results by Deng et al. [17] comparing biportal spinal endoscopy and open surgery for ossification of ligamentum flavum causing thoracic stenosis
Jing et al. [18] published a case report describing a “cave-in” decompression with biportal endoscopy for upper thoracic ossification of posterior longitudinal ligament (OPLL). The authors presented a case of T1-3 OPLL causing spinal cord compression leading to gait disturbance and lower extremity motor weakness. The decompression was carried out in 2 stages with the first stage consisting of excision of the ipsilateral lamina, facet joint, partial transverse process, and pedicles of T2 and T3 with exposure of the dural sac margin using biportal endoscopy. The second stage consisted of removal of OPLL and decompression of the spinal cord after creating 2 additional portals using incisions that were more far lateral in an approach that mirrors a costotransversectomy approach. The OPLL and posterior vertebral bodies were partially resected with a high-speed drill and a cave within the posterior vertebral body was created from one side to the other until the OPLL was separated from the body completely. An eggshell layer of OPLL that was adherent to the dura was released and the remnants of the OPLL were excised. There was no CSF leak or worsening motor strength postoperatively and the patient recovered significant lower limb function. The postoperative modified JOA score was 7 as compared to 5 preoperatively. Postoperative CT and MRI images demonstrated removal of the OPLL and decompression of the spinal cord.
Much work is required for biportal endoscopy to become a viable treatment option for thoracic stenosis. Well-designed clinical studies with long term follow-up are necessary to demonstrate clinical effectiveness with the biportal technique in the thoracic spine. The biportal technique can reduce the morbidity of the surgery as compared to open techniques due to the very minimally invasive nature of the biportal endoscopy. Patients may avoid larger surgery such as open laminectomy, partial thoracic corpectomy and fusion to address thoracic spine pathology and may improve with pain and function expeditiously after surgery. Table 4 summarizes the advantages and disadvantages of the biportal technique for both cervical and thoracic cases.
SAFETY CONSIDERATIONS FOR CERVICAL AND THORACIC CASES
The application of biportal endoscopy for cervical and thoracic central stenosis is limited by the increased risk of spinal cord injury, especially since the spinal cord is already compromised from the stenosis. Significant care should be taken with introducing surgical instruments into the endoscopic field. An important balance should be made with the inflow and outflow of the endoscopic fluid and particular attention should be paid to the status of the inflow and outflow throughout biportal endoscopic surgery. On one hand, the hydrostatic pressure of the endoscopic fluid can reduce bleeding in the epidural space by gently compressing the epidural veins and maintain a clear visual endoscopic field. On the other hand, excessive epidural pressure into the spinal canal can cause iatrogenic spinal cord compression if there is high inflow or insufficient outflow of endoscopic fluid. Many authors recommend keeping the irrigation fluid pressure below 30 mmHg for this very reason.
There is some concern of thermal injury to the neurological structures with the radiofrequency probe and the radiofrequency generator should be set at the lowest setting. Extreme care should be placed on bringing the radiofrequency probe too close to the dura and spinal cord. Utilizing small hook tip radiofrequency probes can precisely deliver the hemostatic energy to a very specific location of the epidural veins, which may reduce the risk of thermal injury to the surrounding neurological structures. Although this is a theoretical risk, no case reports or complications have been described in the published literature to date. Hydrostatic agents such as gelfoam powder soaked in thrombin, Floseal hemostatic matrix, etc can aid in the hemostasis of the epidural veins within the spinal canal.
Intraoperative neuromonitoring should be utilized for these cases. Post-surgical drains should be employed to remove bleeding that could develop into compressive post-operative epidural hematomas, leading to spinal cord compression and neurological deterioration. Furthermore, the technique should be used in select patients and by surgeons who have mastered the biportal technique in the lumbar spine. Traditional open techniques should be the mainstay of treatment until the safety and clinical effectiveness of biportal endoscopy is fully demonstrated with well-designed clinical studies.
POSSIBLE APPLICATIONS
Other uses of biportal endoscopy in the cervical and thoracic spine that have yet to be reported in the literature include evacuation of epidural hematoma and epidural abscess, surgical debridement of osteomyelitis and discitis, surgical decompression of metastatic tumors to the spine, and applications in spine trauma. The treatment of epidural hematoma and epidural abscess with biportal endoscopy would require that the pathology is limited in nature and not diffuse over multiple levels, which would then necessitate open laminectomy and evacuation. Ideally, the lesions are at 1 or 2 levels, localized to the disc space. Computer navigation may assist in localizing the lesions relative to the surrounding more normal spinal anatomy, which can optimize the chances for the success of the surgery.
Kim and Jung [19] published a case report of successfully implementing biportal spinal endoscopy to treat multilevel spontaneous lumbar epidural hematoma but there are no reports of using the technique for cervical and thoracic instances. Biportal endoscopy with intravenous antibiotic therapy was used to successfully treat 13 patients for lumbar epidural abscesses by Kang et al. [20]. Five patients were infected with Staphylococcus aureus with 3 of the 5 having the methicillin-resistant strain. Eight patients reported excellent outcomes using the modified Macnab criteria and 5 patients reported good outcomes. There were no instances of recurrence of infection or perioperative complications with full resolution of the infection. Hsu et al. [21] published a case report on treating Salmonella spondylodiscitis and epidural abscess that extended from T12 to S1 using biportal discectomy and debridement at the L1-2 and L4-5 levels, then introducing a drainage catheter into the epidural space in the intervening levels. However, no reports have been published to date on the use of biportal endoscopy for treatment of epidural abscess in the cervical or thoracic spine.
Treatment of cervical and thoracic metastatic lesions with biportal endoscopy may be a viable option if there is limited spinal cord compression with more localized tumor that was accessible to the endoscope. Tumors that may be more amenable to biportal endoscopy would be those located dorsally or along the lateral borders of the spinal canal and pedicles rather than circumferentially around the spinal cord. Severe circumferential spinal cord compression should be avoided with this technique. Perhaps the far lateral “cave-in” technique described by Jing et al. [18] for thoracic OPLL may be utilized for thoracic metastatic tumors to access the ventral aspect of the spinal canal for mild to moderate circumferential spinal cord decompression. Significant consideration must be made on the vascularity of the tumor since vascularized tumors such as renal cell carcinoma can lead to significant intraoperative bleeding, which would completely obstruct the visualization with the endoscope. Preoperative angiography and embolization may be necessary for certain tumor types to reduce the intraoperative bleeding. Even in tumor types that do not have such vascularity, metastatic tumors can induce a hyperemic state to allow further growth of the tumor. This hyperemic environment can cause enough bleeding intraoperatively to obscure visualization using the biportal endoscopic technique. In addition, the risk of spinal cord injury would still need to be mitigated for biportal endoscopy to be a feasible treatment option. Only highly select cases would be amenable to the biportal technique.
In the trauma setting, utilizing biportal endoscopy for spinal canal decompression in lieu of an open laminectomy may preserve what stability may be left by the traumatized posterior ligamentous complex. Retropulsed fragments in thoracolumbar burst fractures may be reduced in the acute setting using biportal endoscopic visualization. Traumatic epidural hematomas that are limited in size and extent may also be amenable to biportal endoscopy. Although no studies have yet been published on these topics, an opportunity exists to translate the biportal technique to these pathologies in the cervical and thoracic spine.
Recommendations for Risk Reduction
1. Avoid excessive irrigation fluid pressure by maintaining irrigation pressure < 30 mmHg and ensuring ample outflow.
2. Use particular care when inserting surgical instruments into the endoscopic field.
3. Use specialized small hook tip radiofrequency probes to precisely deliver hemostatic energy to reduce thermal injury to the spinal cord and neurological structures.
4. Use radiofrequency generator at the lowest setting once in the spinal canal.
5. Utilize intraoperative electrophysiological neuromonitoring with somatosensory evoked potentials, motor evoked potentials, and EMG
6. Use post-operative drains for all cases.
7. Perform cervical and thoracic cases only after mastering the biportal endoscopic technique in the lumbar spine in select cases only.
CONCLUSIONS
Applications of biportal spinal endoscopy has recently progressed from the lumbar spine to the cervical and thoracic spine. To perform the technique safely in the cervical and thoracic spine, surgeons must first master the technique in the lumbar spine, where there is more room for error. The learning curve is steep for biportal endoscopy as it is for full uniportal endoscopy, however the flexibility, adaptability, and maneuverability may be greater in biportal endoscopy due to the separate viewing and working portals. This may allow for the successful use of biportal endoscopy in the cervical and thoracic spine. Due to the risk of spinal cord injury in the cervical and thoracic spine, measures should be implemented to reduce this risk, such as proper irrigation fluid management, proper insertion and manipulation of surgical instruments to the endoscopic field, meticulous hemostatic technique, intraoperative neuromonitoring, and postoperative drain management. By first mastering the biportal technique with posterior cervical laminoforaminotomy for cervical disc herniations and foraminal stenosis, surgeons can then gradually progress to spinal cord decompression in the cervical and thoracic spine as their skills advance. More extensive research is necessary with well-designed comparative studies with long term follow-up to determine the factors necessary for the safe and effective use of the biportal endoscopic technique in the cervical and thoracic spine. The biportal endoscopic technique is a viable alternative to full endoscopy and other minimally invasive techniques, now with applications in the cervical and thoracic spine.
Notes
Ethical statements
Not applicable.
Conflicts of interest
Dong Hwa Heo is the Editor of the Journal of Minimally Invasive Spine Surgery and Technique and was not involved in the review process of this article. All authors have no other potential conflicts of interest to declare relevant to this article.