Contralateral Lower Limb Radiculopathy Following Minimally Invasive Oblique Lumbar Interbody Fusion in Treatment of Degenerative Lumbar Spine Disease
Article information
Abstract
Objective
To understand the etiology and solution for postoperative contralateral radiculopathy following Minimally Invasive oblique Lumbar Interbody Fusion (MIS OLIF) performed in degenerative lumbar spine disorders. There is lack of sufficient data on contralateral radiculopathy occurring after MIS OLIF. OLIF is an increasingly used procedure performed for degenerative lumbar spine disorders. So, it is important to understand the etiology and solution of potentially avoidable complication.
Methods
Retrospective analysis of 74 consecutive patients with total 97 segments operated was done from May 2016 to December 2019 in whom minimal access oblique lumbar interbody fusion was carried out. All the perioperative complications were noted and patients with contralateral radiculopathy were analyzed clinically and radiologically and etiology for this complication. All these patients followed up at 1, 3, 6 and 12 months postoperatively.
Results
Contralateral radiculopathy was noted in 6 patients (8.1%). Four patients had only pain in opposite limb, 1 patient had partial sensory loss and 1 patient had partial motor loss in addition to pain. Direct decompression was performed in 3 patients whereas 3 patients were managed conservatively. All the patients had complete resolution of pain at 3 months follow-up and there was partial motor and sensory recovery in affected patients.
Conclusion
Contralateral radiculopathy is a potential complication of MIS OLIF. It can be avoided with proper execution of surgical steps especially during cage preparation and proper patient selection is an important key too. Management can be surgical or non-surgical depending upon the etiology of this complication (design of study: retrospective study).
INTRODUCTION
Lumbar interbody fusion is one of the most commonly performed procedure to address degenerative lumbar spine disorders. Various approaches have been described in literature. In past few years anterior and lateral approaches are becoming popular with various advantages like less blood loss, lesser bony resection and muscle damage, shorter hospital stay, avoidance of complications like dural leaks or nerve root injuries; all in comparison to posterior approaches. Minimal access anterior retroperitoneal (anterior to psoas)/Minimally Invasive Oblique Lumbar Interbody Fusion (MIS OLIF) approach was first described in 1997 by Mayer [1].
It is an anterior to psoas approach so unlike LLIF (Lateral Lumbar Interbody Fusion) or transpsoas approach it has less chances of developing complications like anterior thigh pain, paraesthesia over thigh and groin region, hip flexor weakness; all associated with lumbar sympathetic plexus injury [2-5]. It has less chances of vascular injuries as compared to ALIF (Anterior Lumbar Interbody Fusion). However, this approach does have several perioperative complications. Literature has described its various complications including, vascular injuries, lower extremity symptoms like anterior thigh pain/weakness secondary to psoas muscle involvement, peritoneal breach and ileus [6-8].
However, there is limited data on developing contralateral radiculopathy with or without sensorimotor deficits after MIS OLIF or LLIF procedure. Zeng et al. [9] have described this complication in one patient in retrospective analysis of complications following MIS OLIF in 235 patients. Kraiwattanapong et al. [10] also have described this complication following oblique placement of the cage in MIS OLIF. Taher et al. [11] have described incidence of this complication in 7 patients in their series of 244 patients following LLIF. Papanastassiou et al. [12] have reported 2 patients with contralateral motor deficits after LLIF and Son et al. [13] described this complication in a case report following LLIF secondary to oblique placement of the cage.
The aim of this retrospective study was to analyse this complication following MIS OLIF and to understand it’s underlying mechanism and thereby to infer possible ways to avoid it and raise awareness regarding this unusual complication.
MATERIALS AND METHODS
Retrospective analysis of 74 consecutive patients with total 97 segments operated was done from May 2016 to December 2019 in whom minimal access oblique lumbar interbody fusion was carried out.
Inclusion criteria were failed conservative line of management for low back pain with or without radicular pain and neurogenic claudication in lower limbs, which got relieved with rest. Clinically all the patients had neurogenic claudication, no rest pain; with or without back pain. On examination all the patients had negative SLR. Radiologically patients had changes of degenerative lumbar spine disease and instability up to Meyerding grade 2 on dynamic X-rays. MRI criteria was central and lateral lumbar canal stenosis up to Schizas grade C. Exclusion criteria were rest pain, infection, trauma, spondylolisthesis more than grade 3 and acute lumbar disc prolapse.
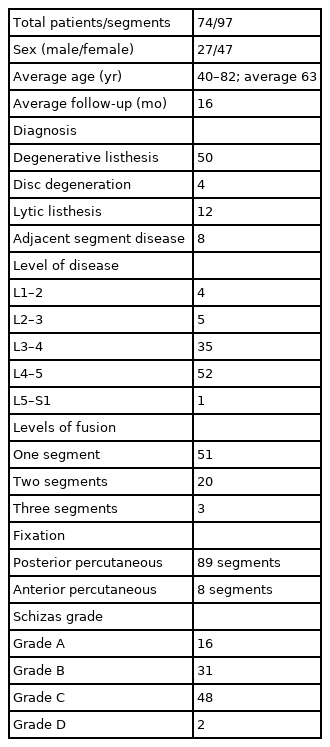
Table 1 shows demographic characteristics, clinical and radiological features of the patients included in the study.
Clinical and neurological assessment of all the patients was done pre operatively and post operatively. Radiological analysis was done using standardized plain AP & Lateral X-rays and MRI of lumbosacral spine. All the patients were operated from left side for OLIF. Autograft was used in 21 patients and artificial bone graft (hydroxyapatite crystals with bone marrow aspirate) was used in 53 patients. After cage insertion, fixation of the lumbar segment was done in the same stage. Posterior percutaneous fixation was done in 89 whereas anterior fixation was done in 8 segments. No direct decompression was done. Neuro-monitoring was not carried out in any patient. Perioperative complications were noted and follow-up was done at 1, 3, and 6 months and then at 1 year.
Among perioperative complications, patients with contralateral radiculopathy with or without sensorimotor deficits were specifically analyzed clinically as well as radiologically.
1. OLIF Procedure
1) The patient was positioned in a true right lateral decubitus position. A 4- to 5-cm skin incision 3–4 cm anterior to the desired disc space after marking under IITV parallel to the fibers of the external oblique muscle was put. The approach was usually performed from the left side.
2) The external oblique, internal oblique and transverse abdominal muscles were then dissected along the direction of their fibers.
The retroperitoneal space was accessed by blunt dissection, and the peritoneal content was mobilized anteriorly. The psoas muscle and genitofemoral nerve were identified, and the intervertebral disc was exposed through an open corridor between the psoas muscle posteriorly and great vessels anteriorly.
3) First dilator was now put over the disc space at junction of anterior 1/3rd and posterior 2/3rd. K-wire was now introduced through the first dilator into the disc space. First dilator was now slightly hammered into the disc space and checked under fluoroscopy. Now the K-wire was removed and serial dilators are introduced over the first dilator. Final tubular retractor was introduced and position checked under fluoroscopy. Once the final position was checked a distractor pin was used to retain the dilator in place.
4) After making a portal, rectangular annulotomy was done by excising the annulus fibrosis. All the instruments which were now used to do discectomy were used by orthogonal maneuver. The disc material including the cartilaginous endplate was excised sequentially, and the annulus fibrosis at the opposite side was released completely with caution using Cobb elevator under fluoroscopic viewing. The psoas muscle was automatically retracted temporally during the orthogonal maneuver.
5) Cage size was determined by appropriate sizers, which were inserted into disc space and confirmed on IITV images.
6) An appropriate-sized cage was filled with autologous bone graft from the iliac crest or synthetic bone substitute as required, and was inserted orthogonally in a press-fit fashion into the disc spaces.
Upon completion of the anterior procedure, the patient was turned to the prone position, and supplemental posterior instrumentation was then placed percutaneously or fixation was done anteriorly. Compression was done.
RESULTS
Ninety-seven segments of 74 consecutive patients were operated with 19 of them male and 55 females. Average age was 63 years. Minimum follow-up was for 4 months and maximum follow-up was for 24 months with average of 14 months. Fifty-six patients had degenerative listhesis, 11 had lytic listhesis, and 7 had adjacent segment disease. Single segment fusion was done in 54 patients, double level fusion done in 17 patients whereas 3 segment fusion done in 3 patients. Average estimated duration for single segment cage placement was 40 minutes
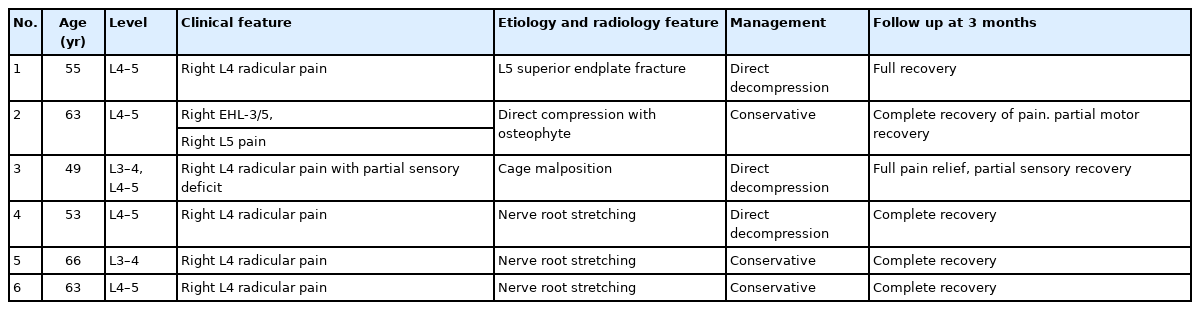
All perioperative complications were noted. Among them contralateral radiculopathy was present in 6 patients (8.1%). All the patients with contralateral radiculopathy were further evaluated clinically as well as by X-rays, CT scan and MRI. The characteristics of those patients have been described in Table 1.
Symptomatically out of 6 patients, 4 patients presented with only radicular pain in the opposite limb without any sensory or motor deficits. One patient developed partial sensory deficits in addition to pain and one patient had motor as well as sensory deficits along with pain. Among all patients, only one patient had double level fusion done whereas rest of them underwent single level fusion. Two patients were managed conservatively whereas 4 patients underwent direct decompression. All the patients had complete resolution of pain at the follow up of 3 months. The patient with sensory deficit had partial recovery of sensory symptoms. The patient who had motor deficit was advised surgery. However, we lost the patient to follow-up for 3 months and when patient showed up for consultation, she had complete resolution of pain and partial recovery of motor weakness.
DISCUSSION
There is minimum literature available till now which discusses contralateral radiculopathy following Minimal access Oblique Lumbar Interbody Fusion (OLIF) in degenerative Lumbar spine disorders. As the application of this approach is gradually being used as means of indirect decompression in such disorders [14-17], it is imperative to understand the possible mechanisms and solutions to contralateral radiculopathy. However, this complication has been widely discussed when it occurs following TLIF [18-20]. In this series authors have analyzed all the patients with this complication clinico-radiologically. Also, the possible ways to avoid has been discussed.
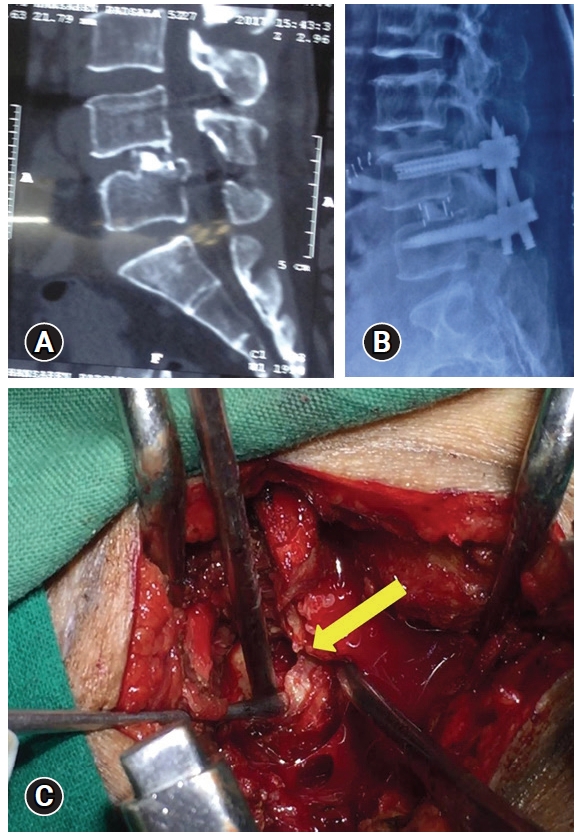
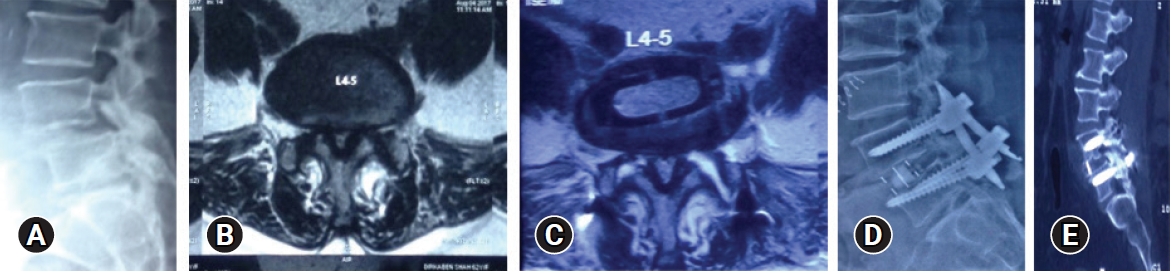
Out of total 6 patients (in the sequence as described in Table 2), patient 1 had fracture of the posterior and superior endplate of L5 vertebra on opposite side and the cage position was also in posterior 1/3rd of the disc space (Figure 1). This might have occurred during disc preparation when Cobbs elevator is used to break annulus on opposite side. If the instrument is not in parallel plane to the endplate and not completely orthogonal, the force to break the annulus can cause fracture of the endplate. In this patient, removal of the offending fragment was done. The patient was pain free at the follow-up of 3 months. In patient 2 with contralateral radiculopathy, there was motor deficit as well in form of EHL grade 3/5. In this patient, postoperative CT scan showed presence of osteophyte over superior facet of L5 on right side (Figure 2). This osteophyte compressed the nerve root while translational correction of the listhesis. It is important to get a pre-operative CT scan to evaluate the facet joints and find out whether there is bony compression by osteophytes. These osteophytes may impinge the nerve roots post operatively. This patient was advised surgery in form of direct decompression. However, we lost the patient to follow-up for 3 months and when patient showed up for consultation, she had complete resolution of pain and partial recovery of motor weakness. Patient 3 with double level fusion who presented with contralateral radiculopathy had cage malposition at L4–5 level (Figure 3). The cage was compressing on the exiting nerve root of L4 on right side. In this patient also direct decompression was done. The oblique position of the cage can be because of the inappropriate execution of the orthogonal maneuver. This patient had complete resolution of the pain. However, there was some persistent sensory paraesthesia.
(A, B) CT scan and X-ray image showing fractured fragment on postero-superior corner of L5 vertebra. (C) Per-operative image showing offending fragment (arrow) compressing the L4 nerve root.
(A, B) Pre-operative images showing Grade 1 listhesis at L4–5 with axial MRI showing subluxated facet joints with foraminal stenosis. (C, D) Post-operative X-ray and MRI showing well positioned cage and pedicle screws. (E) Post-operative CT scan shows facetal osteophyte causing impingement on the foramen.
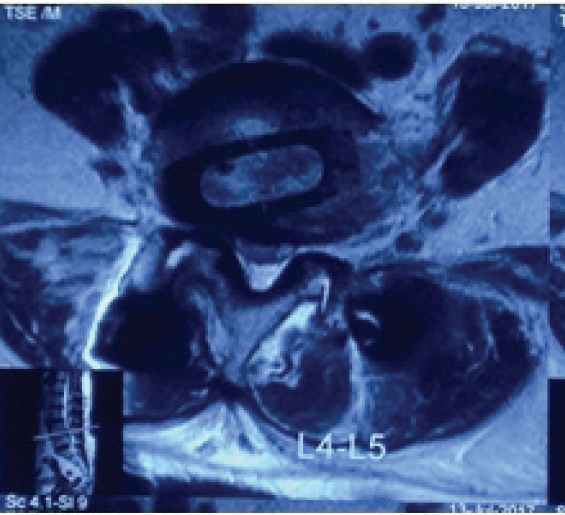
Post-operative axial MRI showing Oblique placement of the cage causing impingement of the nerve root on the opposite side.
In all these three patients the cause of the contralateral radiculopathy was inferred radiologically and could be solved with direct decompression of the involved nerve root. In rest of the three patients (patient 4, 5, 6), no definite cause could be established on imaging studies. Possible mechanism can be, stretching of the nerve root due to larger size cage leading to neuropraxia and thus leading to radicular pain or the cage preparation instruments which may overshoot the opposite side and produce opposite psoas irritation or hematoma giving rise to opposite side pain. Amongst these 3 patients, direct decompression was performed in one patient as there was no relief with the conservative management. Rest of the cases showed complete resolution of the symptoms with conservative management with average follow-up of 6 weeks.
We also compared our results with other studies. In a study by Zeng et al. [9], they analyzed complications in 235 patients and found single case of contralateral radiculopathy (0.4%). It was secondary to abnormal cage position compressing the nerve root. The patient underwent revision surgery for proper placement of the cage. Kraiwattanapong et al. [10] described a case report of this complication. It was again because of the oblique and more posterior placement of the cage leading to contralateral neve root compression. Improper docking and orthogonal maneuver was the cause of oblique cage placement. The authors did revision surgery and repositioned the cage. Taher et al. [11] analyzed 244 patients of LLIF and found out the incidence of this complication to be 2.9% (7 patients) in their series. All these patients had motor deficits apart from contralateral radicular pain. On follow-up, 3 patients had complete resolution of the symptoms, 3 patients had residual deficit and 1 patient was lost to follow-up. Authors have elaborated the possible mechanisms leading to this complication. One of them is neuropraxia secondary to larger size of cage placement leading to nerve root stretching. Also, translational correction of spondylolisthesis can cause entrapment of the nerve root in foramen. Cage malposition and contralateral nerve plexus injury while breaking opposite annulus are other important mechanisms.
From these observations, we can infer some guidelines to avoid this complication which are: Docking at junction of anterior 1/3rd and posterior 2/3rd of disc space, proper execution of the orthogonal maneuver so that cage can be placed horizontally, one should be careful from pushing the cage too much onto the opposite side. Also, while cage preparation, we must keep all the instruments (viz: shavers, cobbs elevators) parallel to the endplate especially in osteoporotic patients to avoid its fracture. Patients who have listhesis with large facet joint osteophyte can be considered a relative contraindication as translational correction of the listhesis can lead to impingement by osteophyte over the nerve root. To avoid oversized cage placement, adjacent segment disc height can be taken as reference for the selection of the cage size. Cage position has to be in anterior 1/3rd as posterior position of cage with less orthogonal maneuver can compress opposite nerve root.
Another important aspect of this complication is learning curve of this procedure. This complication was observed amongst initial 40 patients. We haven’t observed this complication in last 34 patients. So, with increasing experience for this procedure, technical improvement can avoid this complication.
CONCLUSION
Contralateral radiculopathy is a potential complication of MIS OLIF. It can be avoided with proper execution of of surgical steps especially during cage preparation and also proper patient selection is an important key too. Management can be surgical or non surgical depending upon the etiology of this complication.
Notes
No potential conflict of interest relevant to this article.