Full Endoscopic Spine Surgery in the View of Tubular Endoscopic Spine Surgery
Article information
Abstract
Integration of technological advancements across multiple modalities enabled different surgical specialties to embrace various minimally invasive approaches. Such advancements related to spine surgery are gaining popularity due to focal nature of majority of the spine pathologies. Tubular retractors of various types and dimensions have proved their worth by giving very good results when used with either microscope or endoscope. They enable surgical decompression and fusion with minimal alteration of the normal musculoligamentous anatomy of back and have proven their versatility by delivering excellent outcomes for different conditions. The evolution of the techniques of full endoscopy opened new paths which seem promising to further refinement of spine surgery. This progress has brought us to the crossroads of either carrying out the satisfactory techniques of tubular retractors or to try something different by taking another steep learning curve and shifting to full endoscopic techniques. It has to be seen whether the transition to full endoscopic intervention is worth exploring new horizons by taking a longer trajectory of learning when similar advantages are being achieved by existing tubular techniques. In this report, we discuss the pathologies dealt with and the changing trends for developing to full endoscopic techniques under the experience of tubular endoscopic spine surgery.
INTRODUCTION
Minimally invasive surgical techniques have become central in spine practice with the advent of operating microscopes and endoscopes [1-4]. Introduction of the tubular retractors by Foley and Smith [5] in 1997 heralded a paradigm shift in the popularity of minimally invasive techniques in spine surgery. Full endoscopic technique is being widely used in patients with lumbar disease for trans/extra-foraminal surgeries via the posterolateral approach and with a predominantly intradiscal and foraminal surgical fields [4,6-11]. It uses working channels as narrow as 4.2 mm. Tubular spine surgery encompasses tubular endoscopic, tubular microscopic and Destandau techniques [12-14]. This technique mostly uses tubes of diameters 16 mm and 18 mm with newer reports of using much smaller and much bigger diameter-tubes for certain indications [15,16]. This article attempts to discuss the pathologies dealt with both the techniques as well as the changing trends for developing to full endoscopic techniques in the background experience of tubular endoscopic spine surgery.
1. Lumbar Disc Herniations
Disc herniations (HNP) in lumbar spine are dealt with surgically when they are refractory to conservative management and causing significant discomfort to the patient or cause neurological deficits [1]. Various options include open discectomy, microdiscectomy and different forms of minimally invasive surgery. Minimally invasive procedures encompass tubular surgeries as well as full endoscopic spine surgery. Tubular retractors use the mechanism of serial dilation of paraspinal muscles after minimal dissection maintaining intact posterior tension band and undisturbed paraspinal musculature. Endoscopic approaches too maintain the normal anatomy in either transforaminal or interlaminar approaches. There are studies indicating both the techniques can be done under local anesthesia with conscious sedation reducing the risks of general anesthesia and can be carried out as day care procedures [17-19]. Besides, there is evidence of improvement in the operative comfort, surgical outcomes and patient satisfaction on gaining experience with tubular retractors as it would enable the surgeon to accomplish the goals of surgery with narrow diameter tubes. There is evidence of cases of lumbar disc herniation operated with 14 mm and even 12 mm size tubes showing significant improvement in operative time, blood loss, postoperative VAS, ODI scores [20]. Recently, the approaches of unilateral biportal endoscopy (UBE) are described for single as well as multilevel lumbar disc herniations without deep muscle dissection to perform laminotomy and discectomy [21,22]. They appear very promising in the evolution of minimally invasive techniques in decompressive spine surgery. The journal website link can be differentiated from the text. It can be placed elsewhere seperate from the text.
2. Lumbar Central and Paracentral Large Disc Herniation
Large disc herniations pose challenges in disc localisation in minimally invasive approaches due to less cross sectional area of the operating field [23]. There is evidence of excellent long-term outcomes in the cases operated using tubular microdiscectomy with tubes of various sizes according to the size, location and severity of disc herniations [24,25]. On the contrary, failure rates were reported in full endoscopic management of large disc herniations [27]. This can be attributed to the need for skill and expertise of exploration on the shoulder or axilla of nerve roots for any remnants of herniated fragments under such a high magnification. Though this can be relatively easier in tubular techniques due to familiarity with the technique, with the interlaminar approach in endoscopic technique gaining popularity, the ease of handling anatomic details that are similar to tubular techniques can help reduce the failure rates with time. UBE technique for bilateral decompression are described to be done with ease as it provides excellent visualisation and magnification with the interlaminar approach [21,22].
3. Migrated Disc Herniation and High Canal Compromise
Rostral or caudal or at times posterior migration of the herniated disc needs exploration towards the areas beyond the safe zone of Kambin’s triangle. This can be accomplished well by using microtubular techniques based on the direction and extent of migration of disc by docking the tube over pars and wanding around the operative field while tilting the operating table as and when necessary [24]. Translaminar tubular approach enables us to address both rostral and caudally migrated discs by docking tube on the respective laminae at the level of disc [25]. Figure 1 illustrates the tubular microscopic approach by the author in the management of a caudally migrated disc using a 12 mm tubular retractor. Full endoscopy techniques trying controlled reaming of the superior vertebral notch or part of the pedicle, directly visualized endoscopic drilling for accessing these highly migrated discs are opening windows to manage migrated disc herniations. Tubular retractors have proven their worth with good outcomes in migrated disc herniations and high canal compromise but full endoscopy has risks of either incomplete decompression or over resection of bone from pedicle in unexperienced hands. Ergonomic advancements providing better equipment such as angulated drills, lasers, forceps etc., are giving hope for considering the technique of transforaminal endoscopy for migrated discs [26].
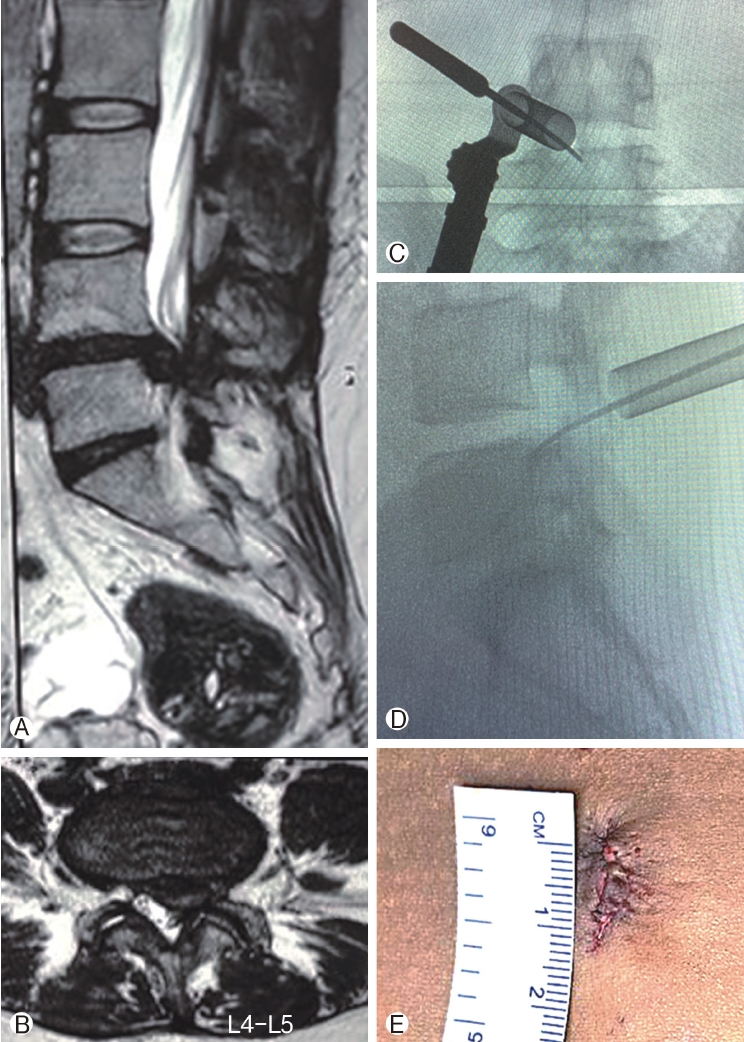
Ⓐ: Pre-operative image of T2 sagittal magnetic resonance imaging showing disc herniation with canal stenosis and caudal migration at L4-5 intervertebral disc level. Ⓑ: Pre-operative image of T2 axial magnetic resonance imaging showing left paracentral disc herniation with canal stenosis at L4-5 intervertebral disc level. Ⓒ : Intra-operative fluoroscopic posteroanterior image accessing the migrated disc using a 12 mm tubular retractor under microscope guidance. Ⓓ: Intra-operative fluoroscopic lateral image accessing the migrated disc using a 12 mm tubular retractor under microscope guidance. Ⓔ: Post-operative image of wound after closure measuring approximately 12mm in length.
4. Recurrent Disc Herniation
Recurrent disc herniations after conventional open or minimally invasive techniques have fibrosed soft tissues posing challenges in dissection and endoscopic manoeuvres. These are the cases which are at high risk for neural injury due to the epidural scarring or fibrosis. Besides, intraoperative bleeding can obscure the operative field in endoscopic spine surgery. Surgeons operating recurrent disc herniations should be well versed with the technique being followed and relevant anatomy. Tubular microscopic techniques have several advantages here with larger tubes that can be relatively better manoeuvred and bleeding control can be achieved, the unaltered intermuscular plane of Wiltse permits easy access to surgical field in cases of earlier midline open decompression. Literature supports the view that there is no significant difference in the outcomes in the cases operated for the revision discectomy and fusion [28]. The main advantage of tubular techniques is their versatility in converting the same procedure to fusions. However, there is evidence supporting the superiority of endoscopy over open and open microscopic techniques in terms of pain relief, minimising complications and earlier rehabilitation [29,30,31]. Full endoscopy on integration with multidisciplinary technological advancements may offer good options to manage recurrent disc herniations in near future.
5. Lumbar Canal Stenosis
In cases of severe canal stenosis, management with ‘over the top’ approach of microtubular laminotomy can decompress both central and lateral recess with minimal bone removal. There is evidence suggesting that there is no significant difference in the final outcomes in terms of pain, function and complications across various grades of severity of canal stenosis operated by microtubular techniques [32]. The patients with extreme stenosis who were relatively more disabled than those with trivial stenosis showed such an improvement that their final outcomes are similar to the latter in terms of ODI and VAS scores after microtubular decompression by unilateral laminotomy and bilateral decompression. The interlaminar approach of full endoscopic spine surgery also has similar ‘over the top’ approach to microtubular laminotomy. In spite of steep learning curve and lack of long-term reports on full endoscopic approach in context of lumbar canal stenosis in the current circumstances, one can reduce the operating times and complications with experience. There are reports showing similar functional outcomes in cases of stenosis when decompression is done by microtubular techniques and full endoscopy with the latter showing favourable rates of complications [33]. Further studies are needed to determine the long term benefits and cost effectiveness of full endoscopy.
6. Instability
Minimally invasive interbody fusion has enabled surgeons to do fusions with significant reduction in peri-operative blood loss, early recovery, shorter hospital stay, lower surgical site infections and undisturbed posterior tension band. Several studies comparing minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) and open TLIF concluded both the techniques have similar outcomes [32,34]. Tubular microscopic techniques coupled with percutaneous pedicle screws offer a less steeper learning curve than full endoscopic fusion techniques like unilateral biportal and uniportal approaches. Tubular techniques not only allow large diameter (7.5 mm) percutaneous pedicle screws but are also congenial for manipulation and reduction of extreme spondylolisthesis or even spondyloptosis [35]. The author described reduction of spondyloptosis in an obese individual by cantilever mechanism under tubular microscopic guidance using the cage of MISTLIF as a lever to reduce the vertebral slip. While such manoeuvres are feasible with tubular retractors, it will probably take some more time to realise such a possibility with full endoscopic techniques.
Currently, There is evidence citing fusions done by unilateral biportal endoscopy provide a view which is very similar to that of tubular retractors. It uses two different ipsilateral portals -one for endoscope and second working portal. It has a learning curve less steeper than uniportal endoscopy but it is recommended to gain experience in many microtubular surgeries before attempting biportal endoscopy [36]. Till date, the fusions done by endoscopic techniques included low grade spondylolisthesis. High grade spondylolisthesis is regarded as a contraindication for full endoscopy. Long term follow-up and larger clinical trials are necessary apart from development of instrumentation to accommodate 7.5 mm pedicle screws, expandable cages, avoid interference of continuous saline irrigation for intradiscal bone packing and to overcome other technical limitations.
7. Synovial Cysts and Tumors
Excision of synovial cysts and localised tumors can be done by both tubular endoscopic and full endoscopic techniques reducing morbidity. Management of tumors under local anesthesia is ideal and would be a boon for patients with co-morbidities and a low life expectancy. Lumbar intraspinal synovial cysts can be decompressed from the contralateral side by tubular microscopic techniques sparing the facet and avoiding fusion adding to the versatility of the technique [29]. Intradural pathology and tumors of the spine can be managed by minimally invasive techniques conserving the bony and musculoligamentous tissues essential for stability of spine. There are studies reporting the usage of microtubular technique to excise focal tumors like osteoid osteoma from C2 vertebra [24,37,38]. The tubular retractors provide adequate window for tumor surgery which is still not completely established with full endoscopy. There is scope for expansion of the indications of full endoscopic spine surgery with time and experience to include certain pathologic conditions.
8. Cervical Spine-HNP, Radiculopathy and Myelopathy
Application of any minimally invasive technique to cervical spine surgery needs expertise with the technique. Posterior cervical foraminotomy in cases of foraminal disc or bony stenosis causing radicular pain can be performed by minimally invasive techniques. Tubular techniques are commonly used for posterior based approaches but expandable tubular retractors are particularly handy when doing anterior cervical spine fusion surgeries in cases of myelopathy and radiculopathy. They reduce the pressure of retraction and risk of iatrogenic injury to viscera, cause less postoperative pain and dysphagia, and better cosmesis with small scar [39]. Microscopic anterior cervical discectomy and fusion (ACDF), anterior cervical corpectomy and fusion (ACCF) can be done with help of tubular retractors. Direct decompression, restoring cervical lordosis and anterior column reconstruction can be achieved [40,41]. On the other hand, full endoscopic techniques can achieve almost anything and everything - posterior foraminotomy, unilateral laminectomy and bilateral decompression, anterior discectomy and anterior trans-corporeal discectomy. Spacers can be placed endoscopically after discectomy to maintain disc height. However, trials comparing microtubular ACDF or full endoscopic anterior/posterior foraminotomy and discectomy are lacking.
9. Thoracic Spine HNP
Symptomatic thoracic spine disc herniations can be excellently excised using tubular microendoscopic [42] as well as full endoscopic techniques [43].
Advantages of Full Endoscopic Spine Surgery
Like other minimally invasive modalities, the endoscopic techniques have certain advantages over open techniques like less blood loss, early recovery, short hospital stay, good patient satisfaction outcomes and general acceptance and preference by both patients as well as the treating surgeons. Endoscopic techniques in spite of smaller portals, give a magnified view of the spinal canal increasing the scope for identification of new pathologies, development of new surgical techniques, involving lasers, radiofrequency coagulators and further refinement of surgical capabilities. Cosmetic appearance with smaller scar is another advantage of full endoscopic spine surgical techniques. Either the full endoscopic approach or the tubular approaches, both give minimal scar as most of the surgeries are done in prone position with the surface area of the back stretched out and when patient becomes upright, the small incisions shrink to smaller scars. Ability to carry out decompression as a day care procedure under local anesthesia with conscious sedation is an advantage of both full endoscopy and tubular techniques [17-19]. Minimally invasive techniques focus on the site of pathology, so they do involve measures to localise the level before giving skin incision reducing the incidence of wrong level spine surgery than in open technique [44]. Evolution of biportal endoscopic spine and adjacent segment degeneration [22].surgery expanded the indications identical to those of open technique like disc herniations, stenosis, low-grade spondylolisthesis.
Disadvantages of Full Endoscopic Spine Surgery
Lack of versatility narrows down the pathologies which can be treated with full endoscopic techniques. Inadequate long term evidence is available regarding the endoscopic lumbar fusion surgeries and outcomes. Tubular techniques are the attractive alternatives with greater versatility. Requiring adequate hands on exposure with microtubular technique before carrying out biportal endoscopy is recommended by endoscopic spine surgeons. Though they give a magnified view, they lack adequate working area and field of vision of operative site is narrow which adds to the difficulty in the learning curve. Constant irrigation can cause increased cerebrospinal pressure, which can further lead to neurologic dysfunction. Surgeon must make sure good, uninterrupted inflow and outflow irrigation system is in place. Irrigation can also interfere with intradiscal bone packing in fusion surgeries. Radiation exposure to surgeon as well as the patient is more as the instrumentation is entirely c-arm guided.
Challenges of Full Endoscopic Spine Surgeries
The potential challenges of full endoscopic spine surgeries include steeper learning curve, increased cerebrospinal fluid pressure, haemorrhage, epidural, psoas and retroperitoneal hematomas, endoscopic management of intraoperative complications, wrong level surgeries. Handling of the instruments as well as anatomic structures in the operative field needs proper training. Surgeons should develop the skill to manage common intra-operative endoscopic complications like incidental durotomy, neurovascular injuries, pedicle injuries, peritoneal injuries, missed fragments, instrument related complications without conversion to open surgery. Delayed post-operative complications reported include psoas abscess, post discectomy pseudocyst formation, instability, epidural scarring, spondylodiscitis and recurrence. Endoscopic techniques have limitations in their indications and patients who are not suitable for minimally invasive procedures like high-grade spondylolisthesis, deformity corrections, fractures and other pathologies that necessitate open techniques.
Paradigm Shift to Full Endoscopic Technique
A paradigm shift from tubular microscopic spine surgery to full endoscopic technique is an attractive potential possibility keeping in mind the smaller portals, magnified view of the operative field and cosmetic scar. Good results have been documented with tubular techniques with limited exposure of visceral surface area to pathogens and reduced incidence of surgical site infections [44], similar cosmetic advantage and significant patient satisfactory outcomes. The scar left by tubular technique is small and cosmetic too. A surgeon who is trained, already established and generally satisfied with tubular techniques and their versatility may question himself the reason to shift to full endoscopy by taking another steep and difficult learning curve when such major advantages and benefits are associated with tubular surgeries and the same applies to full endoscopic techniques.
Caution and Tension
Even after taking a long and steep learning curve, a devoted full endoscopic spine surgeon may be confined to a narrow range of spine conditions. Full endoscopic spine surgery may be associated with difficulty in localisation of the pathology with narrow tube of endoscope and overmagnified anatomy. In private practice, another limitation for full endoscopy would be the recurrent cost of the instruments and accessories. Cost is a concern even in relation to tubular surgeries, but of a limited magnitude.
CONCLUSION
In full endoscopic spine surgeries or the tubular techniques the principles are almost the same and the pathologic conditions to learn are the same. It appears possible and easier for a surgeon already familiar with tubular techniques to turn into full endoscopic spine surgeon. But it has to be seen whether it is worth taking a second, longer and steeper learning curve and if the overall advantages are the same after travelling towards the end of the learning curve. In budding spine surgeons, it can even cause Dunning-Kruger effect as the field is upcoming and a lot of knowledge and experience has to be gained to obtain optimum competence. Certain limitations do exist for a technique in its evolving stages but the possibility of achieving long term evidence citing significant advantages over the existing techniques in terms of patient and surgeon satisfaction, operating costs, recovery and rehabilitation will have to be seen.
Notes
Dr. AG Kulkarni is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. There are no other potential conflicts of interest relevant to this article to declare.