Learning Curve for Minimally Invasive Spine Surgeries: A Review of Initial 162 Patients in Five Years of Implementing MISS Technique
Article information
Abstract
Objective
An inherent learning curve is associated with minimal invasive spine surgery (MISS). Operation time, complications and learning-curve are associated with one another during an initial learning. The purpose was to identify the learning-curve in MISS procedures (for both discectomy and fixations).
Methods
We performed a retrospective analysis in initial 162 patients who were operated by a single surgeon during first five-years of independently implementing MISS. All surgeries were performed using tubular retractor between 2012 and 2016 in form of microendoscopic discectomy (MED), and later added with MISS-fixations. All had single or double level disc herniation with or without lumbar stenosis and/or instability. In-patient charts were reviewed to compare intraoperative blood loss, operative time, hospital stay and complications.
Results
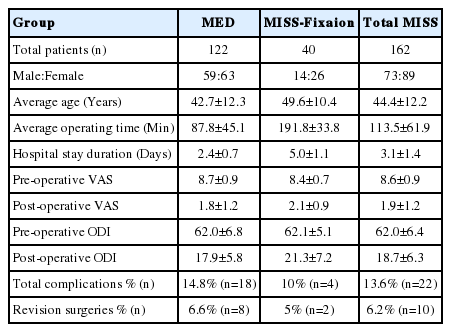
Average age was 44.4±12.2 years and average operation time was 113.5±61.9 minutes. Operative time was decreased to less than 90 minutes after 30 surgeries, and less than 60 minutes after 50 surgeries for MED. For MISS-fixations, it was 191.8±33.8 minutes. Average hospital stay was 3.1±1.4 days, which was significantly less in MED compared to MISS-fixation (p<0.0001). Preoperative VAS was improved from 8.6±0.9 to 1.9±1.2 (p<0.05) postoperatively. Preoperative ODI was improved from 62±6.8 to 17.9±5.8 postoperatively. Complication rate was 13.6% (n=22) and revision surgery rate was 6.2% (n=10). Intraoperative and postoperative complications such as, dural tear, root sleeve injury, postoperative hematoma, incomplete excision requiring revision and loosening of screw cap were found during initial fifty surgeries; however, recurrent disc and iatrogenic instability was found throughout the series.
Conclusion
Fellowship training facilitates art of learning MISS surgeries and infuse confidence during initial 30 surgeries. Higher complications and operative time is commonly encountered during learning curve. Surgeon needs to stay persistent despite initial complications. After 50 cases, a plateau is usually attained with less complications and satisfactory outcome.
INTRODUCTION
Several studies have shown benefits of minimally invasive spine surgeries (MISS) over the conventional fusion methods in terms of intraoperative blood loss, severity of postoperative pain and hospital stay [1,20,25,26]. However, literature has also reported complications related to surgeon’s learning curve [10,11,29]. The complication rates have been shown to vary in different surgeons’ hands. Literature has reported a common set of complications such as, neurological deficit, dural tear, wound infection, malpositioning of screw and cage migration while using MISS techniques [1,10,11,20,25,26,29]. However, these studies have reported the learning curve either for Micro-Endoscopic Discectomies (MEDs) or for MISS-fixations. None of the existing literature has reviewed a learning curve when both the procedures are implemented simultaneously. A spine surgeon usually attempts both procedures simultaneously; and skill acquired in MED also helps during MISS-fixation surgeries. However, there is no literature available suggesting which procedure to start with while implementing MISS in to one’s clinical practise; and at what stage one should add the other complex MISS procedures.
Endoscopic transforaminal decompression with fragmentectomy technique or tubular retractor based technique have been evolved as a minimal invasive technique [16]. Surgeon who takes time to learn these techniques, has specific training during the fellowship or has actually scrubbed with the mentor may find the learning curve less steeper. The high learning curve discourages the surgeons from adopting the endoscopic or MISS techniques for implementing it in to their clinical practice [16]. A major challenge of MISS is the technical difficulty of working through a narrow surgical corridor, which results in to a limited visualization of anatomic landmarks. The learning curve is challenging and a spine surgeon trained in traditional method must overcome it to master MISS [2,8]. Inspite of adequate surgical training, there are surgical difficulties, high complication rate, long operative hours and increased overall expenditure, which eventually affects the surgical confidence. Therefore many people fail to adapt and continue the new technique. The purpose of this study was to analyze the learning curve of a spine surgeon while implementing the MISS technique in both discectomies and fixations because a skill acquired in discectomy also facilitates the art of MISS fixations. Our study shall help young surgeons to pave their path for MISS surgeries and assess the commonly encountered complications.
MATERIALS AND METHOD
This retrospective review analysis was performed in initial 162 patients (73 male and 89 female) who were operated between 2012 and 2016 by a single surgeon while implementing MISS technique in to the clinical practice. The average age of patients for the study was 44.4±12.2 years. All patients were operated by MED and MISS fixations using the tubular retractor system. All patients had single or double level pathologies for which they were operated. A total of 168 patients were operated using MISS technique. Four patients did not give consent to participate in the study and 2 were lost to follow-up. Hence, 162 patients were included in this study. All patients were followed-up for a minimum period of 2 years postoperatively. The inclusion criteria for MED were clinical evidence of lumbar disc herniation (LDH) and clinical findings were consistent with MRI (Magnetic Resonance Imaging). Each patient had at least 6 weeks of failed conservative trial and signs of radiculopathy were not improving and/or worsening. Lumbar sagittal X-rays and MRIs were used to correlate clinical and radiological findings. Patients who had spinal instability in form of spondylolisthesis, facetal hypertrophy or facetal effusion were selected for MISS-TLIF procedure. LDH without spinal instability was treated with micro-endoscopic discectomy with fenestration surgery (MED) using the tubular retractor. Foraminal decompression was carried out in cases with foraminal stenosis.
All patients were operated by a single spine surgeon who is fellowship trained in MISS techniques. The MISS procedure was performed using tubular dilators (METRx- Medtronics, USA) only at levels found to be positive as determined by the MRI and clinical symptoms. In accordance with the procedure described by Perez-Cruet et al. [21], after the guide-wire inserted over respected level and side under c-arm, initial dilator was inserted over the guide-wire after 2-cm skin incision across the guidewire. Serial dilators were then gradually inserted to dilate paraspinal muscles up to the lamina. Final retractor tube was inserted and fixed with the table clamp. Remaining serial dilators were removed and microscope was brought in for further procedure. Later fenestration was created at index lamina which was followed by falvotomy to expose root and dura. Root was retracted gently to expose the herniated disc. The herniated disc was carefully removed and nerve root was made free of the tension.
In certain cases, TLIF (transforaminal lumbar interbody fusion) was required for additional stabilization, which was also performed using the MISS techniques [19,27]. TLIF was performed on more symptomatic sides. Fluoroscopy was used to determine the operative level in all cases. The pedicle screws were inserted at the respective levels under fluoroscopy guidance. The pedicles were identified and the Jamshedi needle was inserted. Guide wires were placed in the tracks made at the respective levels and the direction of the screw placement checked under lateral fluoroscopy image. This was followed by sequential dilatation, reaming and screw insertion. The disc space were identified under fluroscopy and a vertical skin incision (length: 22 mm) was kept at the disc space level cranially 12 mm and caudally 10 mm. A tubular retractor system (METRx- Medtronics, USA) was then introduced under fluoroscopic guidance to the facet joint. The first (smallest) tubular dilator was inserted and docked to the facet complex. Dilators of increasing diameter were then sequentially inserted to dissect muscles off the underlying facet complex. A working port was then introduced and secured to the operative table with a special arm. Decompression, discectomy and cage insertion were done from the same port under microscope.
Postoperative follow-up was done at 6 weeks, 3, 6, 12 months and yearly thereafter. The patients were also followed up in case of any complication or urgent assistance. Results were analyzed using VAS (Visual Analogue Score) for pain and ODI (Oswestry Disability Index) scores. Perioperative and postoperative complications were specifically recorded and studied from the hospital records. Complications that were recorded from the day of operation to three months postoperative period were included in perioperative complications. Complications seen after three months were included in postoperative complications.
RESULTS
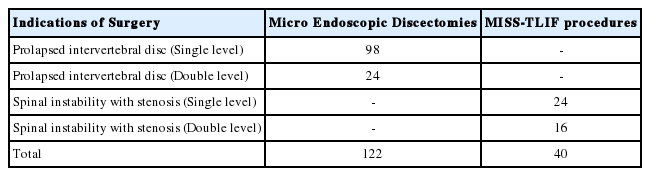
Surgeries were successfully performed in all patients. None of the surgery was converted to an open procedure in the series. There were 122 MED and 40 MISS-TLIF procedures carried out as per the requirement of the patients’ pathology (Table 1). Average follow-up was 49.1±14.4 months (range, 29-87 months). The average operative time was 113.5±61.9 minutes (range, 35-300 minutes) (Table 2). While comparing operative time of MED versus MISS-TLIF in patients, we found that the average surgical time in MED was 87.8±45.1 minutes (range, 35-270 minutes) versus 191.8±33.8 minutes (range, 140-300 minutes) in MISS-TLIF (p<0.0001). Longer duration was observed in MISS-TLIF surgeries as compared to MED alone (p<0.0001, t-test). However, it was observed that the average time duration in MISS surgeries decreased with the increase in number of cases in each group (Fig. 1). The analysis of the operative time showed that the average surgical time in MED group decreased to less than 90 minutes after 30 surgeries (Fig. 1Ⓐ). After initial 50 surgeries, the timing for single level discectomy and decompression was less than 60 minutes including bilateral decompression with unilateral approach (Fig. 1Ⓐ). Average hospital stay was around 3.1±1.4 days. The hospital stay in MED (2.4±0.7 days) patients was significantly less as compared to MISS-TLIF (5±1.1 days) (p<0.0001, t-test). Longer duration of admission was required for patients undergoing fixations. It was observed that the average duration of the hospital stay also decreased with the increase in the number of cases, however it was not significant. Estimated blood loss (EBL) was higher in MISS-TLIF group when compared with MED group with an average EBL of 52.3±37.3 mL (109.9±23.5 mL in MISS-TLIF versus 33.4±14.6 mL in MED, p<0.0001) (Table 2).
Summary of the study results for the evaluation of the learning curve for Minimally Invasive Spine Surgery procedures
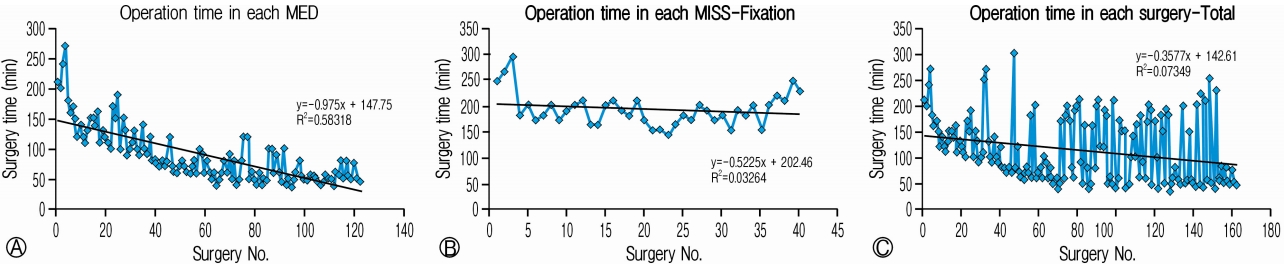
Operative time in surgery group versus the patient number. Operative time was reduced gradually in each group of surgery Ⓐ MED, Ⓑ MISS-Fixation and Ⓒ Total MISS group. In between higher picks suggested double level decompresssion along with/without fixations.
The VAS (Visual Analogue Score) decreased from preoperative score of 8.6±0.9 to 1.9±1.2 postoperatively showing significant improvement (p<0.05) in painful condition of the patients (Table 2). Similarly ODI scores also showed reduction from preoperative 62±6.4 to 18.7±6.3 postoperatively, which suggested significant improvement (p<0.05) in their quality of life.
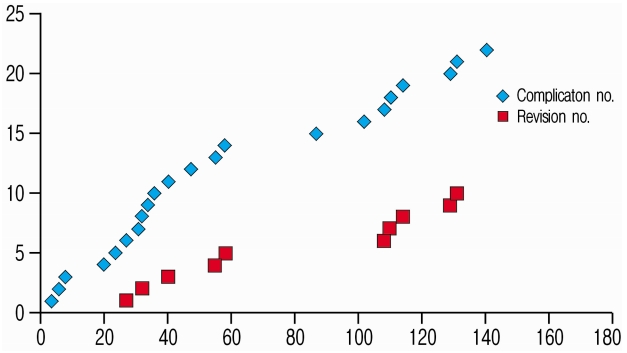
There were complications and difficulties related with handiling of neural tissues such as dural tear and root sleeve injuries were noticed in initial cases (Table 3). These complications were not seen in later cases. Other complications were related with surgical expertise, which included incomplete excision was also seen in initial 50 cases. Other complications such as, instability, loosening of cap, discitis and broken instrumentation/implants were seen scattered (Fig. 2) (Table 3). It was noted that the surgeries conducted after 50 cases did not have complications such as dural tear or root sleeve injuries; however, recurrent disc or instability happened in later cases as well. The overall complication rate was 13.6% (22 out of 162) with 6.2% (10 out of 162) of the patients requiring revision surgeries. MED had more complications (18 out of 122, 14.8%) as compared to MISSTLIF procedure (4 out of 40, 10%) in the study group (Fig. 3). There were 10 patients (6.2%) who required revision surgeries; 8 (6.6%) from MED group and 2 (5%) from MISS-TLIF group. There was statistically no difference in complications or revision surgeries between two groups (p=0.734 for complications and p=0.837 for revisions, chi square test). There were five patients who did not return to their work after surgeries in the series. There were 4 patients from MED group and one from MISS-TLIF group and all of them having complications in form of dural or root sleev injuries, epidural hematoma and incomplete excision of the discs. All patients who did not return to their previous work were operated in initial 50 surgeries (Table 3).
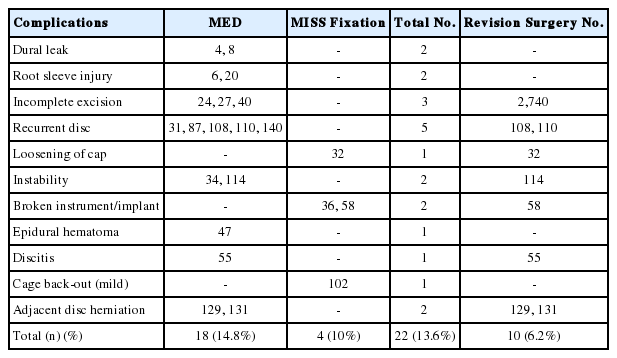
Complications encountered during the learning curve of Minimally Invasive Spine Surgeries. ‘Surgery No.’ indicates the case number operated by the spine surgeon during the learning curve, 1 being the first case operated
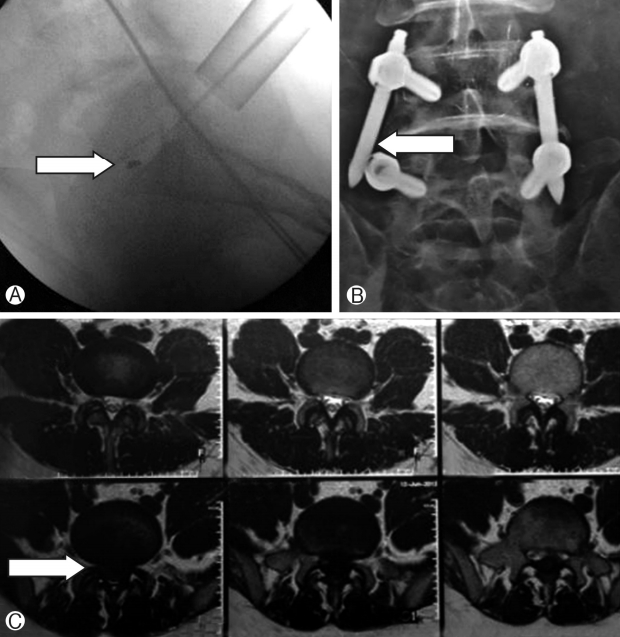
Complications encountered during MISS and MED surgeries. Ⓐ Broken tip of disc forceps, Ⓑ Loosening of screw cap which required revision surgery and Ⓒ Incomplete excision of the disc which required revision surgery.
DISCUSSION
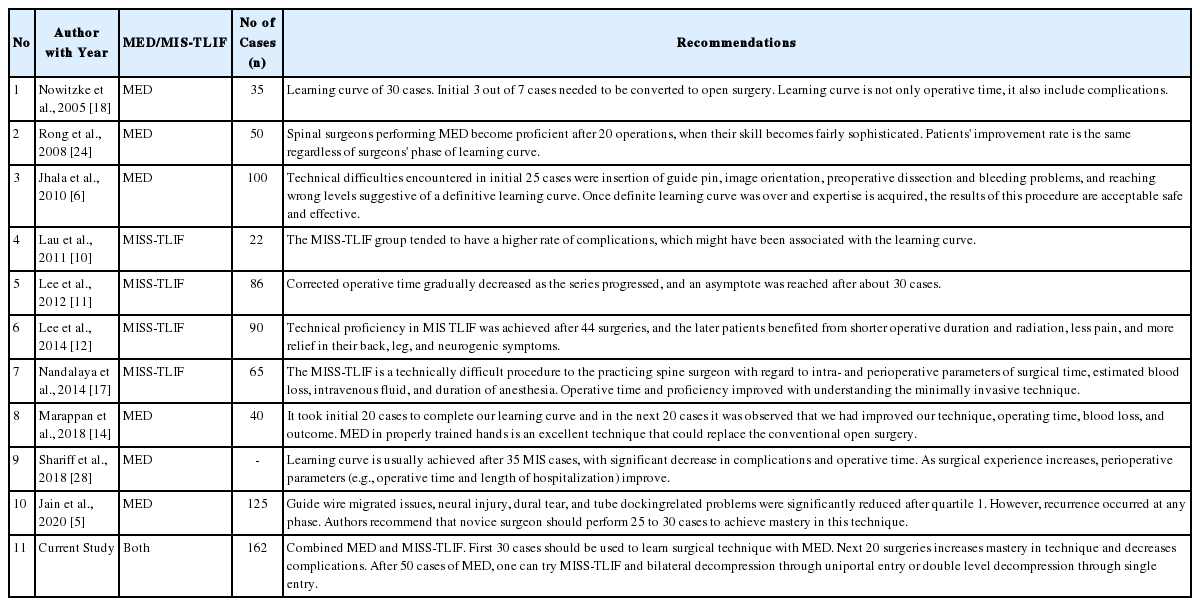
Most of the studies conducted in the recent era have focussed on either MED or MISS-fixations exclusively [6,11,21,30]. We report a unique study where the analysis of learning curve includes both MED and MISS-fixations. Hence it provides a practical applicability to the spine surgeon who wants to implement both surgeries simultaneously, not merely being limited to only one procedure. A skill developed in MED also helps in MISS-fixations and vice-versa making the learning curve less steep. As described by Cook et al., a learning curve must contain a starting point (normally the first case), a learning rate (with increasing performance on patient outcome) and an asymptote when the expert level is reached [22]. In this study, we report a typical learning curve as described by Cook et al. which may pave way for the growing spine surgeons. To the best of our knowledge, this is the first study that has included MED and MISS-TLIF both in learning curve.
In a retrospective study by Jhala et al., the mean duration of surgery was found to be 70 minutes [6]. Our study shows a mean of 113.5±61.9 minutes. The reason for the difference in timing is the fact that we have included MISS-fixations along with MED. The mean duration of only MED procedure in our study was 87.8±45.1 minutes, which is comparable with the other studies conducted. Additionally, there were 24 patients who had double level MED, which is the other reason to have slightly longer operative time in MED group. Therefore, if we further divide operation time according to single level MED, average time would further decrease. Perez-Cruet et al. [25] showed an average surgical time of 66 minutes and complication rate of 5%. We had complications in 13.6% of our study population, which included both MISS-TLIF and MED. Similar results have also been shown in a few literature where the success rate ranges between 88% and 98.5% [3,9,15] with only either of the procedures performed (MISS-TLIF or MED). This paper again emphasize that beginners need to be ready and persistent with his learning curve in spite of higher complication rate while implementing MISS techniques in to clinical practice.
Katayama et al. in their study compared the results of microdiscectomy versus macrodiscectomy [7]. They reported that there was no difference between the surgical outcomes of both; however, microdiscectomy gave better lighting, magnification and therefore decreased the length of incision and tissue invasion. They have also noted that microdiscectomy allowed the patients to return early to their work with lesser use of postoperative narcotic analgesics. Returning early to work is not only important for the psychological needs of the patient but also for improving the socio-economic status of the family [4]. Comparing average hospital stay of 1-2 days, 7.7 hours and 24-48 hours according to Jhala et al., Perez-Cruet et al. and Ranjan et al. [6,21,23], respectively, we had an average hospital stay of 3.06±1.38 days. The patients included in other studies had only MED without fixation. The average hospital stay for MEDs alone in our patients was 2.6±1.04 days which is comparable with the existing studies. They had shown a complication rate of around 5-6.5% versus 13.6% in our study. About 4% of their patients underwent repeat surgeries versus 5.6% patients in our study.
Lee et al. had studied the learning curve of MISS-TLIF [11]. They studied single level fusions in 86 cases with 2 years follow-up. As per their study, 30 cases were needed to reach a plateau in operative time. Similarly Jhala et al. [6] and Rong et al. [24] suggested to perform 25 and 20 cases with MED to become familiar with the technique and to overcome the learning curve. Similarly other literature also indicated to perform 20-40 cases of MED to overcome learning curve in the technique [5,14,28] (Table 4). In our case series, operative time had reached a plateau at around 50th case for MED and MISS TLIF both. In our study with MED cases we have noticed that initial 30 cases are required to get accustomed with the technique as surgical time gradually decreased to 90 minutes; and further 20 cases are required to master the technique as operation time was less than 60 minutes (Fig. 4). Later on there was not a major change in operation time after 50 surgeries. We must remember that double level cases or bilateral decompression would vary in surgical time even after 50 cases; however, it can be dealt with surgical expertise after proficiency achieved during initial 50 cases. Also we have seen that average operative time was gradually decreased in both groups (Fig. 1); however, it will increase if surgery is at two levels. In an another study by Lee et al. of 144 MISS-TLIFs, average duration of surgery was 166.4 minutes and the patients had to stay for around 3.4 days in the hospital [13]. Similarly other studies on learning curve in MISS-TLIF noted that it has higher complication rates and longer operation time as it is technically more challenging [10,17]. Lee et al. noticed that technical proficiency in MISS-TLIF was achieved after 44 surgeries, and the later patients benefited from shorter operative duration and radiation [13]. Our study had an average surgical time of 117±54 minutes and hospital stay of 3.06±1.38 days. This may be due to the inclusion of MED along with MISS-TLIF in it. The average duration of surgery for MISS-TLIF alone was 125±30.5 minutes and hospital stay of 5.2±1.2 days which is comparable with the studies conducted.
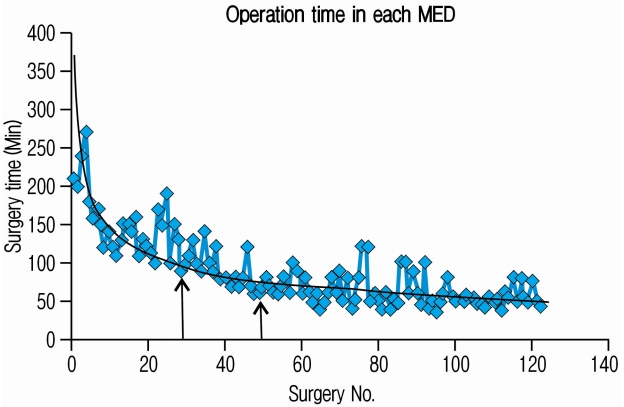
Figure suggests our learning curve pattern in MED cases. Power analysis shows surgical time reduced to 90 minutes in first 30 cases and it further reduced to 60 minutes in next 20 cases. Overall surgical time remained around 60 minutes after 50 cases. Surgical time may vary depending upon double level discs and bilateral decompression.
There were a number of complications encountered during the learning curve of MISS surgeries ranging from dural leak and root sleeve injury in the initial stages to implant loosening and mild back out of cage in MISS-TLIF procedures (Table 3). Nowitzke et al. in their series of 35 cases with MED noticed that 3 out of initial 7 cases needed to be converted to the open procedures and therefore, learning curve is not only operative time, it also includes complications [18] (Table 4). The complications were reduced after meticulous handling of the instruments, as the learning curve of the surgeon is improved. The blood loss also showed inverse correlation with the experience of the surgeon. Haematoma was noticed in one case after discectomy. This was prevented in future cases by meticulous haemostasisby cauterization. Discitis prevention was done by maintaining strict sterility of the equipments. Compression of the construct was carried out to reduce the incidences of cage backout. These all complications in intial implementation of MISS technique gradually improves to a surgeon as learning curve gets better.
This study was focused on the learning curve on an individual surgeon on MISS techniques. Large number of patients (162) as compared to the previously conducted studies makes it more informative. Inclusion of MED and MISS-TLIF, and thereby, studying the learning curve together gives a unique platform for young spine surgeons. An observation in our institute shows that the number of patients opting for MED has increased over the period of five years. With only 10% of the patients who required discectomy were selected for MED in 2012, it was increased to 90% in 2016. This also indicated on increased satisfaction and confidence of the individuals and the surgeon with MISS surgeries. It also indicates that as surgeon’s learning curve progresses, surgeon would be more inclined to perform MISS procedures. However, this may not be applied to MISS-TLIF procedures due to higher cost constrain.
As stated by Cook et al. [16,22], “Case mix sometimes complicates assessment of learning curves because as the surgeon becomes more experienced, the cases attempted become more difficult”. This also applies here; as the confidence of the surgeon handling this technique rose, cases that had been rejected earlier were included and solved. This is evident by the fact that the number of MISS-TLIF increased in later surgeries as compared to first 50 cases. In summary, we studied 162 cases of MED and MISS-TLIF surgeries and explored a method to calculate the surgeon’s learning curve. This would help the new spine surgeons to pave a way for a more confident surgical experience with better learning outcomes in both MED and MISS fixations.
CONCLUSION
MISS is a procedure for discectomy and/or fixation with early encouraging results. A spine surgeon needs to believe and stay persistent while implementing MISS surgeries in spite of clinical fellowship. MED gives satisfactory confidence during initial 30 surgeries. Higher complication rates and operative time is commonly encountered during initial surgeries. Next 20 cases can be combined with simple MISS fixations and mastering the technique. After 50 cases, a plateau phase is attained; hence MISS-fixation and TLIF can be attempted.
Notes
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical Approval
This study complies with the current ethical norms and does not contain any studies with human participants or animals performed by any of the authors. It is a retrospective analysis of the surgeries performed in the hospital. The surgeries have been performed after informed consent and approval of the patients.