Transpedicular Percutaneous Discectomy for High-Grade Down-Migrated Lumbar Disc Herniation
Article information
Abstract
Objective
The purpose of this study was to evaluate the clinical outcomes of percutaneous endoscopic discectomy using the transpedicular approach for hernias with down-migration.
Methods
The study involved a retrospective descriptive analysis of 7 patients who underwent surgery by 2 senior surgeons at 4 different hospitals between 2016 and 2024. The minimum follow-up period was 6 months. All patients were treated with lumbar discectomy through a transpedicular approach with an oblique trajectory. Preoperative and postoperative clinical data were collected for statistical analysis.
Results
The surgical procedures were successful and complication-free for all patients. The preoperative and postoperative radicular visual analogue scale and Oswestry Disability Index scores were compared, and the differences were statistically significant (p<0.05).
Conclusion
At the last follow-up, 100% of patients had good to excellent results according to the modified MacNab criteria. The transpedicular approach, when using a percutaneous endoscopic technique, requires precise surgical planning and accurate knowledge of the vertebral anatomy. The technique can be made more accessible to inexperienced surgeons by describing it with different instrumentation.
INTRODUCTION
Percutaneous endoscopic lumbar discectomy is a minimally invasive technique that reduces iatrogenic injury to paraspinal muscles, ligaments, and facet joints. It also reduces intraoperative bleeding, postoperative pain, hospital stay, and time off work compared to other surgical alternatives [1,2].
This improvement is due to the use of new working cannula endoscopes, laser and radiofrequency probes, bone drills, and flexible articulated curved forceps. Technological advancements have enabled the performance of percutaneous endoscopic spine surgery, which includes the removal of herniated discs beyond the intervertebral space. This overcomes the anatomical barriers that previously restricted access. The statement is supported by reference [3]. However, treating herniated discs with significant displacement using traditional approaches (transforaminal or interlaminar) can be challenging and may result in segment instability or significant retraction of neurological structures [4].
It is important to note that herniated discs with high-grade down-migration in zone 4 of Lee's classification [5] are most likely to disconnect from the disc and produce disc sequestration. Incomplete hernia removal is the primary cause of failure of endoscopic discectomy [4,6].
Accessing the juxtapedicular epidural space involves creating a tunnel through the pedicle to reach the medial wall, as described by Krzok et al. [7] and subsequently modified for trajectory [8-10].
This article presents the techniques used with different instrumentation (joimax, MaxMoreSpine, and elliquence) and the results of 7 patients with high-grade down-migrated disc herniations.
1. Preoperative Planning
Adequate preoperative planning is necessary to perform the technique safely. In addition to traditional radiological analysis in orthogonal projections, computed tomography (CT) and magnetic resonance imaging (MRI) obtained within the last 3 months, are necessary to rule out the presence of hypoplastic pedicle, calcified disc fragment, severe osteoporosis, and central disc herniations with down-migration [8].
Traditional radiology provides a preview of the intraoperative fluoroscopic images. In both projections, it is necessary to identify and mark the pedicles, as well as the position of the migrated disc in the lateral projection.
On axial CT and MRI slices, it is important to identify calcification of the disc, hypertrophy of the yellow ligament, stenosis of the lateral recess, and degeneration and possible hypertrophy of the interfacial joint. These structures could potentially interpose between the medial bone wall and the disc herniation.
Sagittal and coronal MRI slices allow accurate assessment of the location of the migrated disc herniation, while CT slices allow measurement of the height (>12 mm) and width of the pedicle (>8 mm) (Figure 1).
2. Technique Steps
The patient is positioned in a prone position with the patient’s hips and knees flexed on cushioned supports and a radiolucent table. General anaesthesia is used in all cases described. The skin incision point and trajectory of the Tomshidi needle (or similar) has to be planned using the preoperative imaging studies.
Discography (1 mL of methylene blue or indigo carmine, 2 mL of serum, and 2 mL of contrast) is recommended to improve visualization of the migrated disc fragment and differentiate it from other structures.
The procedure involves advancing a needle or Tomshidi (MaxMoreSpine, Hoogland Spine Products GmbH, Munich, Germany) until it is positioned on the lateral wall of the pedicle above the transverse process. Orthogonal intraoperative x-ray images are obtained to verify the correct placement of the needle before commencing reaming or drilling through the pedicle bone.
Next, the spinal needle or Tomshidi is replaced by a guide needle to introduce the obturator through an approximately 8-mm incision in the skin and paraspinal muscles. The obturator tip should be placed on the lateral wall of the pedicle.
There are variations depending on the chosen instrumentation. For MaxMoreSpine, the Tomshidi is introduced into the pedicle without penetrating the medial wall. Then, the guide wire is introduced, and the atraumatic hand drills are progressively introduced through it until an 8 mm tunnel is achieved, still without penetrating the medial wall of the pedicle (Figure 2).

Steps of the manual drilling technique (MaxMoreSpine, Hoogland Spine Products GmbH, Munich, Germany).
When using joimax (joimax GmbH, Karlsruhe, Germany) or elliquence (elliquence, LLC, Baldwin, NY, USA) instruments, tunnelling of the pedicle from lateral to medial should be initiated after insertion of the obturator and working cannula, using either fluoroscopy or a motorized drill. The use of trephines can decrease surgical time, but it is important to note that mobility within the pedicle is limited. For better visualization, we recommend using a 30° endoscope.
To facilitate the extraction of the migrated disc fragment, it is recommended to use a 30° angulation and flexible instruments. If there is difficulty in removing the hernia, accessing the disc space through Kambin's triangle is an alternative. In certain instances, the utilization of both approaches may be warranted due to the extent of the herniation. Transpedicular access is indicated for fragments that cannot be reached from the foraminal approach.
After the initial tunnelling, the medial wall can be penetrated using a diamond burr on a high-speed motor under direct endoscopic vision (Figure 3).
The target point should always be the medial wall of the pedicle to reach the juxtapedicular disc fragment. The endoscope is inserted through the tunnel to directly visualize the migrated disc herniation. Cancellous bone haemorrhage often occurs during pedicle drilling, but it can be stopped with the radiofrequency probe or the use of motorized diamond burr drilling.
Once the disc is visualized, the radiofrequency probe can be used to reduce the fragment for easy removal with flexible endoscopic forceps. The surgeon explores the ventral juxtapedicular epidural space using an endoscopic nerve hook to confirm complete removal of the herniated disc and freedom of the transverse nerve root. The endoscope and working cannula are then removed, and the wound is closed with a single skin suture (see Supplementary Video Clip 1 of case number 6) (Figure 4).
MATERIALS AND METHODS
The study is a retrospective descriptive analysis of 7 patients who underwent surgery by 2 senior surgeons in 4 different hospitals between 2016 and 2024. The minimum follow-up period was 6 months. All patients were treated with lumbar discectomy through a transpedicular approach with an oblique trajectory. Preoperative and postoperative clinical data were collected for statistical analysis. A descriptive analysis of the data was performed, calculating means and standard deviations.
To study the evolution of variables between preoperative and postoperative periods, repeated measures contrasts were employed (parametric or nonparametric depending on the normality of the samples). The R Development Core Team analysis software, version 4.1.3 (R Foundation for Statistical Computing, Vienna, Austria), was used. A significance level of p<0.05 was determined as statistically significant.
RESULTS
All procedures were completed without the need for open surgery. The surgeries were performed at the segmental level of L2–3 in four cases, L3–4 in one case, and L4–5 in two cases. The patients had a mean age of 52±17.75 years. The mean follow-up period was 44.7±39.8 months, with a minimum follow-up of 6 months. The preoperative radicular VAS score had a mean of 8.43±1.13, which improved to 1±1,15 and the preoperative axial back pain VAS score had a mean of 4,43±1,51, which improved to 0,29±0,76, with a minimum follow-up of 6 months postoperatively (p=0.017).
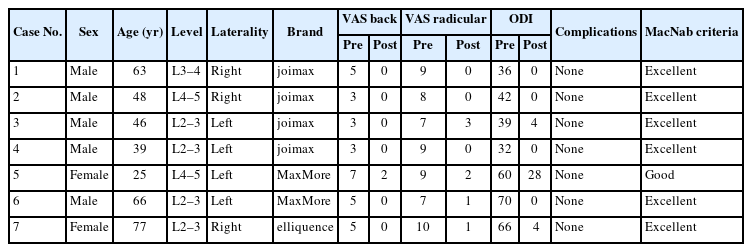
The mean Oswestry Disability Index (ODI) score also improved from 49.29±15.59 preoperatively to 5.14±10..25 at final follow-up (p=0.018). Both the VAS and ODI scores showed significant improvement at each postoperative time point. Based on the MacNab surgery outcome criteria, 85.7% (6 of 7) of patients achieved an excellent outcome. And only one patient reported a good outcome, as shown in Table 1.
DISCUSSION
Despite significant advancements in surgical technique and technology over the past few decades, patients with herniated discs that have migrated continue to pose a challenge for endoscopic discectomy.
Lee et al. [5] developed a classification system based on the location of disc herniation migration in the sagittal plane of the MRI. They noted that significant upward or downward migrations were not suitable for the transforaminal approach. Traditional surgery was recommended due to the high failure rate of endoscopic procedures.
Choi et al. [11] suggested that the interlaminar approach offers better exposure for migrated disc herniations and is superior to the transforaminal approach.
Yang et al. [12] compared the efficacy and safety of interlaminar endoscopy and microscopic discectomy and reported similar clinical results for this type of herniation, except for low back pain, which was significantly reduced in the endoscopic option (interlaminar endoscopic lumbar discectomy).
Another study [13] compared the clinical results of the microscopic translaminar approach with the transpedicular approach. The transpedicular approach was found to be superior to the other surgical option in terms of postoperative pain relief, neurological recovery, and the Oswestry quality of life scoring system.
In 2017, a modification was described regarding the entry angle. The vertical orientation carries a significant risk of pedicle height fracture and surgical failure. The proposed oblique orientation reduces this potential complication [9].
Jiang et al. [10] suggest that if the disc herniation is very large and cannot be removed entirely, a release of the neurological structures should be performed. Although annuloplasty cannot be performed and the intervertebral space is not reached, the risk of recurrence theoretically increases. However, we have not observed any hernia recurrence in our patients. Likewise, in our cases, we have not encountered any complications such as pedicular fracture, instability requiring stabilization or persistence of symptoms due to residual fragment.
It should be noted that the anatomical characteristics of the lumbar pedicles vary depending on the level [14]. Therefore, the use of this approach in the pedicles of L1 and L2 is relatively contraindicated due to the high risk of fracture caused by their small dimensions [15].
However, it is important to acknowledge that our study has a limitation in that the number of cases is small. Therefore, larger samples are needed to determine the reliability and safety of the procedure.
During the follow-up, we performed axial tomography scans on our patients, and we have observed the persistence of the pedicle tunnel in one patient (Figure 5).

(A) Transpedicular tunnelling direction. (B) Postoperative computed tomography scan of patient number 6.
In conclusion, we recommend proper planning of the entry point and angulation, as well as correlation between radiological and nuclear magnetic resonance images, to ensure access to the most distal point of hernia migration. Although there are several brands available, initial access can be achieved using either manual or trephine drills. Tunnelling of the medial wall can be performed with a motorized diamond drill and Kerrison forceps to limit the risk of neurological injury.
CONCLUSION
The application of consecutive steps in a sequential, safe, and protocolized manner allows for effective teaching and reduces potential complications. This approach shortens the learning curve and facilitates the implementation of the technique for treating down-migration juxtapedicular herniated discs in selected patients [16].
Advancements in navigation and robotics can greatly benefit the endoscopic transpedicular approach for percutaneous pedicle screw implantation. Real-time control of the guide wire's positioning in all 3 planes of space allows for accurate design and performance of the working tunnel, reducing potential complications and increasing the likelihood of successful complete removal of the hernial fragment.
Notes
Conflict of Interest
The corresponding author, Manuel González-Murillo, is a consultant of Stryker, MaxMoreSpine, elliquence, and Unintech in Spain and Portugal. The other authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Supplementary Material
Supplementary video clip 1 can be found via https://doi.org/10.21182/jmisst.2024.01298.
Supplementary video clip 1.
OOOOOO.