Technical Considerations and Avoiding Complications in Interlaminar Endoscopic Lumbar Discectomy
Article information
Abstract
The fully endoscopic technique has become the most effective and safest option for the treatment of lumbar disc herniation. Specifically, the interlaminar approach, which was first described at the beginning of the 21st century, is used for the treatment of L4–5 and L5–S1 intracanal disc herniation. Learning protocolized maneuvers facilitates reproducibility and increases the safety of the procedure. The description of the main maneuvers in this article aims to reduce complications and the learning curve with their widespread implementation.
INTRODUCTION
Throughout history, there have been advances in technology that have enabled the treatment of different pathologies through the application of minimally invasive techniques. Spinal endoscopy constitutes a paradigm shift in the treatment of spinal pathology. Since Forst and Haussman [1,2] introduced the arthroscope into the spine to visualize it, modifications have been developed in instruments and approaches that, today, make spinal endoscopy close to be considered the gold-standard in the treatment of disc herniation and soon also in the treatment of canal stenosis [3,4].
In the area of the lumbar spine, it is possible to differentiate 2 main endoscopic approaches in full-endoscopy for the treatment of disc herniation: transforaminal endoscopic lumbar discectomy and interlaminar endoscopic lumbar discectomy (IELD).
The transforaminal approach, which was historically described first, uses the Parviz Kambin’s [5-7] safe triangular zone corridor. It is an essential approach for every endoscopic surgeon and is suitable for various hernia locations and revision procedures.
The interlaminar approach, originally described simultaneously by Choi et al. [8] and Ruetten et al. [9] at the beginning of the 21st century for the treatment of L5–S1 intracanal disc herniations, has progressively expanded its indications. It is currently the gold-standard approach for L4–5 and L5–S1 intracanal hernias and for canal stenosis [10].
Unlike the transforaminal approach, in the interlaminar approach (more familiar to spine surgeons), a posterior approach is used, passing through the lamina and the flavum ligament. As far as complications are concerned, postoperative dysesthesia is more frequent in the transforaminal approach [11] and certain modifications have been described with the aim of reducing its occurrence [12]. In the interlaminar approach, despite having a larger space, excessive traction of the dural sac and roots can also cause injuries and other complications. The reproducibility of the technique could reduce the occurrence of complications.
The aim of this article is to provide a description of the technical connotations and expedients necessary to avoid complications in the interlaminar approach in the treatment of disc herniation (IELD).
SURGICAL TECHNIQUE
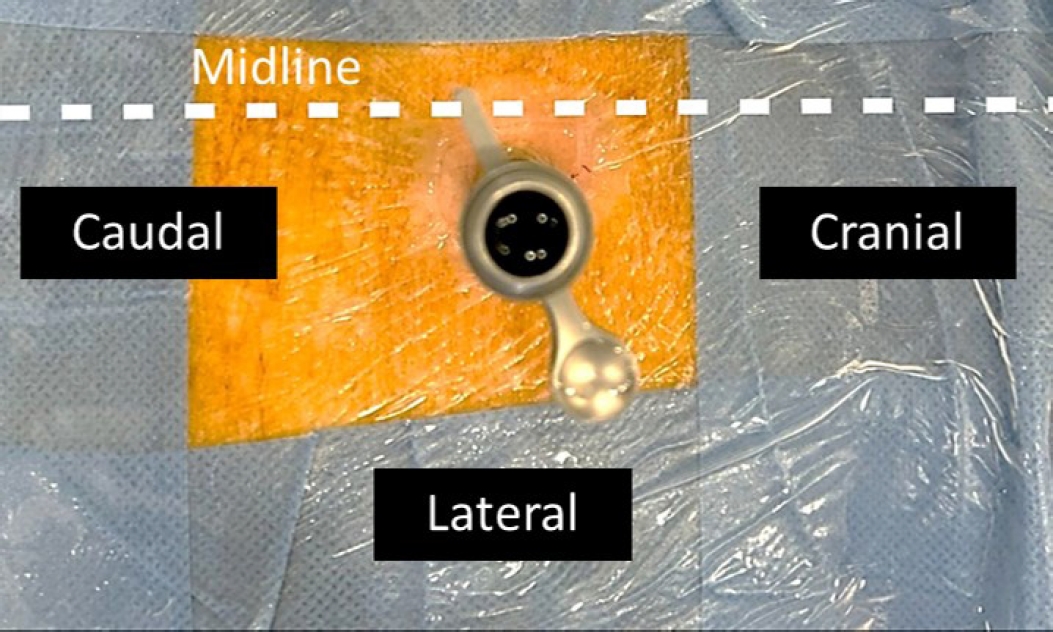
The interlaminar approach (IELD) can be performed under local anesthesia, regional anesthesia with sedation, or general anesthesia. With the patient in a prone position on a radiolucent table with padded supports under the chest and pelvis and semiflexed knees, the interlaminar window is marked on the side corresponding to the pathology to be treated.
An 8- to 10-mm incision is made in the skin with a number 11 scalpel until reaching the muscular fascia plane. If the patient has a lot of adipose tissue, it is recommended to incise with the scalpel until it touches the tip of the spinous process and then lateralize it to penetrate the fascia. This will facilitate the subsequent insertion of the dilator.
The choice of instruments should be emphasized at this point. There are different brands on the market that provide solutions for different pathologies. In the case of some commercial brands, it is advisable to choose transforaminal instruments for this approach. Although they are longer and may cause some difficulty in handling them in thin patients, their smaller thickness means that, once inside the canal, they cause less traction on the neurological structures.
After insertion of the dilator, the latter is used to blindly dissect the multifidus muscle from the cranial and caudal laminae with craniocaudal movements. The surgeon positions himself in the interlaminar window that constitutes the valley between the vertebral laminae, and the adequate positioning is certified using intraoperative scopy.
Next, the working cannula is inserted with the bevel pointing medially. At this point, we recommend not performing cranio-caudal movements in order to avoid disinserting the flavum ligament from the lateral region.
After cleaning and excising the muscular and adipose tissue above the flavum ligament, a small entry is made with the dissector so that serum enters the epidural space and causes a detachment due to hydrostatic pressure.
In lumbar segments above L5–S1, a limited hemilaminectomy is performed through the removal of bone along the attachment of the flavum ligament, employing a diamond burr with a high-speed drill. Additional bone resection of the rostral or caudal lamina may be undertaken to facilitate access to displaced disc fragments. The specific dimensions of the hemilaminectomy are currently subjective and will be finalized subsequently, alongside a potential lateral recess decompression, once the precise boundary of neural structures has been ascertained.
There are several ways to incise the flavum ligament: directly (with a needle and a dilator), longitudinally (following the fibers of the ligament), transversely (from medial to lateral), or by detaching the ligament from the lateral recess (splitting [13]).
We recommend the transverse incision from medial to lateral with scissors, always facing laterally. This incision allows better mobilization of the working cannula and reduces potential complications of dural or neurological injury. The application of pressure of the working cannula on the surface of the ligament flavum provides tension, which favors its progressive separation.
Once in the epidural space, the blood vessels of the lateral recess are coagulated, and it is assessed whether a recessectomy using Kerrison forceps is needed. The objective is to visualize the lateral margin of the nerve. Once visualized, mobilization is performed with a Penfield dissector and the introduction of the working cannula.
This is a key step in our goal of avoiding neurological and dural injury complications. The insertion of the working cannula should be performed perpendicular to the nerve axis, not to the spinal axis.
Suh et al. [14] in their 2005-cadaver study on the analysis of the origin of the spinal roots in relation to the intervertebral disc determined that, in the case of L5–S1, the S1 root never originates below the disc level but rather above it 75% and at the same level 25% of the time. These findings explain why disc herniation at L5–S1 is mostly axillary. In the case of the L5 root, it originates above the disc in 12.5%, at the level of the disc in 25% and below it in 62.5% of the cases.
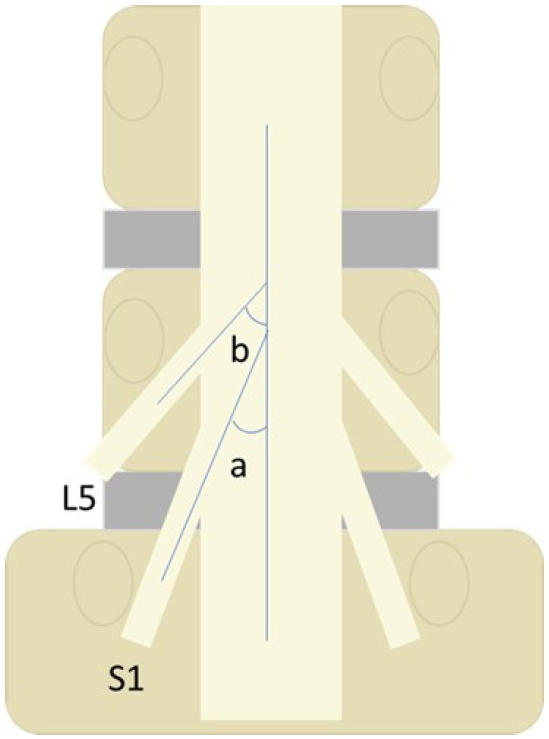
On the other hand, in the morphometric analysis using magnetic resonance imaging performed by Hasegawa et al. [15], it is determined that the average starting angle between the neural axis and the S1 root is 17.9°±5.8° and 27.7°±8° at the L5 root (Figure 1).
Considering these anatomical data and the fact that the appearance of an axillary hernia can increase the starting angle, it is recommended to insert the working cannula perpendicular to the nerve root pathway to avoid neurological injury to the nerve in its caudal portion (Figures 2 and 3).
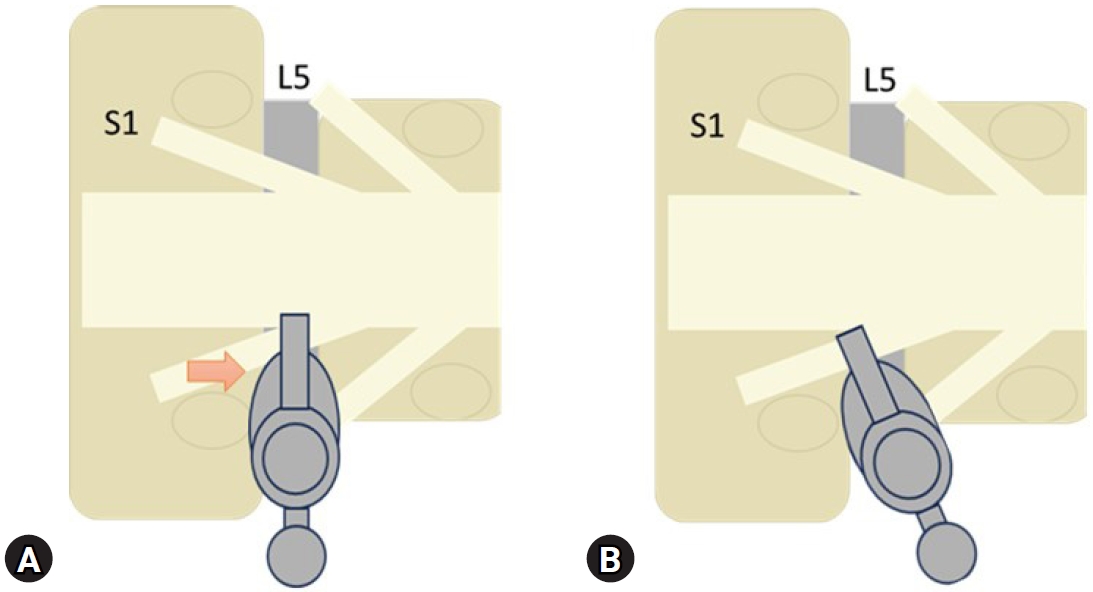
(A) If the cannula is inserted perpendicular to the neural axis, damage may be caused in the distal area of the root (red arrow). (B) Recommended insertion maneuver perpendicular to the root.
Once separation with the dissector and insertion of the working cannula have been performed the endoscope is moved medially so that the tip of the working cannula is introduced into the recess, and it is rotated there to protect the neurological structures. This limits traction of the nerve and the dural sac. It is possible then to move gently and progressively to start the discectomy (Figure 4).
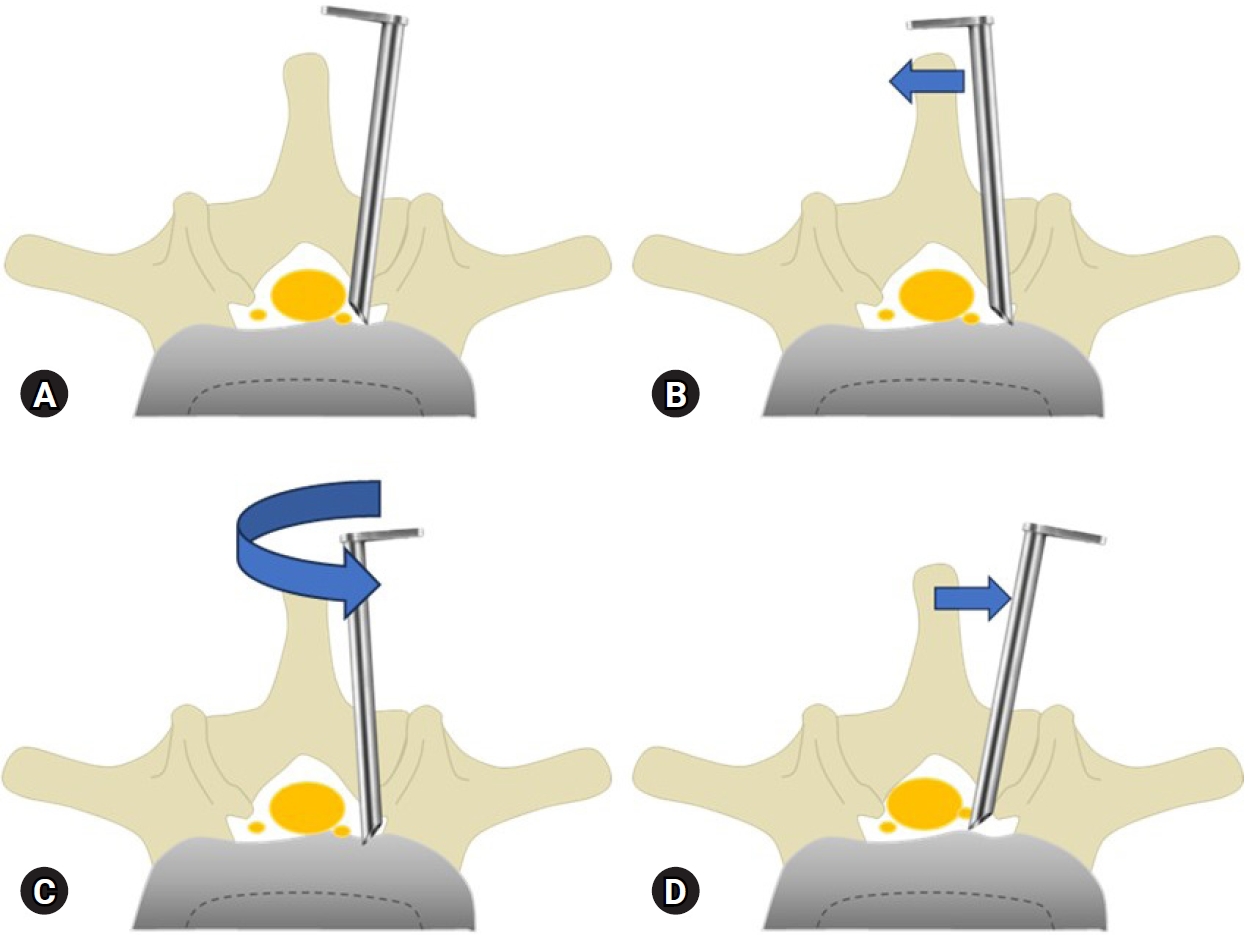
Working cannula mobilization maneuvers with the aim of reducing the retraction of the dural sac and lumbosacral roots. (A) Separation and insertion of the working cannula perpendicular to the nerve root. (B) Medial mobilization with the objective of introducing the tip of the cannula into the recess. (C) Rotation of the cannula. (D) Lateral mobilization for the separation of the sac medially.
We should mention that sometimes, if the disc herniation is large, it is necessary, prior to all these maneuvers, to partially remove a disc fragment to avoid excessive traction of the nerve.
When discectomy is performed, intermittent neurological release of the working cannula by means of its rotation and displacement towards the recess is recommended. This release will reduce ischemia in neurological structures, avoiding injuries to them, and will also facilitate the exit of disc fragments.
CONCLUSION
The application of consecutive steps in a sequential, safe and protocolized manner allows them to be taught and reduces potential complications. In this way, the learning curve will be progressively shortened and will facilitate the establishment of this technique as the gold-standard in the treatment of intracanal disc herniation in L4–5 and L5–S1.
Notes
Conflict of Interest
The corresponding author, Manuel González-Murillo, is a consultant of Stryker, MaxMoreSpine Elliquence and Unintech in Spain and Portugal. The other authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.