Evaluation of Traversing Nerve Root Injuries During Endoscopic Transforaminal Lumbar Interbody Fusion: Observation of Traversing Root via an Accessory Portal
Article information
Abstract
Objective
The aim of this study was to observe possible risks for traversing root injuries during endoscopic transforaminal lumbar interbody fusion (endo-TLIF) via an accessory portal.
Methods
Twenty patients were recruited for this study according to our inclusion and exclusion criteria. An accessory portal was made 3 cm caudal to the working portal, and a 30°/4.3-mm endoscope was utilized to observe possible risks for traversing root injuries throughout the entire process of disc preparation and cage implantation.
Results
The traversing root was observed via the accessory portal throughout the process of disc preparation and cage implantation in 20 patients. Endo-TLIF was shown to be a suitable method for decompression and cage implantation as it provided a sufficient working space and window. No cases of traversing root injuries were observed in our study.
Conclusion
Endo-TLIF was found to be a suitable method for disc preparation and cage implantation. Our observations showed that endo-TLIF is a safe method for decompression, disc preparation, and cage implantation.
INTRODUCTION
Due to an ageing population, we are seeing an increasing incidence of spinal degenerative diseases [1]. Symptoms may vary between individuals, ranging from persistent aching pain in the back or neck to radiating numbness, tingling or pain throughout the limbs [2-4]. Discectomy and laminectomy are the most common surgical procedure performed, which involves removal of the herniated disc and degenerated vertebral [5]. However, for severe degenerative diseases, whereby the surrounding vertebral and joints are unable to provide adequate structural support, spinal fusion may be recommended for symptoms relief and provide structural stability [6,7]. Traditionally, there are several approaches for spinal fusion which includes the anterior approach (anterior lumbar interbody fusion), posterior approach (posterolateral lumbar interbody fusion, PLIF) and lateral approach (lateral lumbar interbody fusion) [8].
With development of endoscopic equipment and technologies, we are currently increasing interests in endoscopic spinal surgery as it utilizes smaller incisions as compared to traditional open surgeries [9]. Current endoscopic techniques include the biportal endoscopic transforaminal lumbar interbody fusion (TLIF) and the uniportal endoscopic posterolateral TLIF [10,11]. The biportal TLIF uses a viewing scope placed on the contralateral side via the Kambin triangle, with a working scope placed on the ipsilateral side. Kang et al. [4] compared the biportal TLIF with PLIF and minimal invasive TLIF and concluded that the former had favourable postoperative 1-year follow-up outcomes with faster recovery and no differences in fusion rates. The reported advantages of the Trans-Kambin approach include, ability to perform under local anesthesia, direct viewing of fusion and discectomy, and preservation of the vertebral body [12]. However, there were concerns regarding traversing and exiting nerve root injuries as the neural components were not visualized with the Trans-Kambin approach. Traditionally, surgeons relied heavily on motor-evoked potentials and electromyography for intraoperative neural examinations. Furthermore, the size of the Trans-Kambin window was also reported to be sufficient only for implantation of small cages.
Harms and Jeszensky [11] proposed an approach involving facetectomy to enlarge the working space of Kambin’s triangle, whereby Foley et al. [13] used this as a platform to a propose a minimally invasive tubular approach TLIF. However, it was still technically challenging due to the small working channels of the equipments used. The uniportal endop-TLIF is one such procedure that is currently gaining popularity [14]. Kim and Wu et al. first reported on the use of uniportal endoscopic TLIF in grade 2 spondylolisthesis and scoliosis patients with <30° curve [7,8,12]. Clinical results showed that such a procedure is safe with good early functional results and improvement in coronal Cobb angles [7]. They further showed that such an approach can be used to adjust foraminal height, disc height, and improve alignment whilst simultaneously minimizing collateral soft tissue injury. It was hypothesized that endoscopic TLIF (endo-TLIF) had reduced risks of traversing root injury due to its unique approach and wider viewing window. However, there are currently no available articles reporting regarding the risks of traversing root injury and endo-TLIF. Therefore, in this study, we inserted a second accessory portal to observe the traversing root during disc preparation for endo-TLIF to observe for risks of traversing root injuries.
MATERIALS AND METHODS
1. Patient Cohort
This study was approved by the Institutional Review Board (IRB) of China Medical University Hospital, Taichung, Taiwan and conducted in accordance with the Helsinki Declaration (IRB No. 31541). Written informed consents were obtained from all participants. From January 2022 to December 2023, 20 patients were assessed for eligibility for endo-TLIF and prospectively recruited from China Medical University Hospital, Taichung, Taiwan. Diagnosis was done using lumbar spine magnetic resonance imaging and physical examinations. Inclusion criteria include: (1) grade II and below spondylolisthesis, (2) spinal stenosis with instability, (3) adjacent segment disease, and (4) recurrent disc herniation. Exclusion criteria include: (1) spinal fusion surgery due to trauma, (2) revision spinal fusion surgery, (3) infection, (4) tumor, (5) pseudoarthroses, (6) congenital spinal deformity, and (7) sagittal malalignment. All patients completed at least 6 months of postoperative follow-ups at our out-patient department clinic.
2. Surgical Technique
1) Position, anesthesia, and approach
The patient was intubated under general anesthesia and placed in a prone position on a radiolucent surgical spine table. The skin incision corresponded with the trajectory for the upper percutaneous pedicle screw. Due to the flexibility of the uniportal endoscope, unlike the fixed tubular fusion technique, the location of our incisions did not interfere with the process of discs preparations.
2) Docking and working channel placement
A guidewire was placed onto the medial inferior portion between the facet joint and caudal vertebral lamina. Gradual dilatation was done using an obturator and an open bevel working channel was docked and secured. A 10°/7.1-mm LUSTA endoscopic System (Vantage Biotech Co., Ltd., Taoyuan, Taiwan) was used for the central and lateral recess decompression. When necessary, a 30°/4.3-mm endoscopic System (Vantage Biotech Co., Ltd.) was utilized for enhanced intervertebral disc clearance due to its orientation. This procedure was conducted under saline irrigation.
3) Systematic drilling with facetectomy
The decision on which side to perform the facetectomy was influenced by the patient's clinical presentation and site of compression based on his preoperative radiographic imaging. Inferior facetectomy was done by drilling on the isthmus with the intention to excise fibrotic tissues associated with isthmic spondylolisthesis and to free the inferior articular process (IAP). For a thorough en bloc harvest of the inferior facet, the scope is retracted to the halfway point, and the working cannula was leveraged to manipulate the IAP away from the facet capsule and fibrotic tissues. The IAP was then harvested using a forceps for subsequent bone grafting. The base of the superior articular process (SAP) could then be visualized clearly after IAP facetectomy. Superior facetectomy and harvesting of SAP was then done by drilling on the intersection of the caudal lamina and transverse process with an endoscopic osteotome. After which, the lateral flavum was released. To prevent unintentional dura tears, the inner layer of the ligamentum flavum was preserved till bony decompression was completed. The ipsilateral ligamentum flavum was detached via dissection from its superior and inferior laminal attachments after bone decompression. If contralateral decompression was determined to be required due to lateral recess or foraminal stenosis, the contralateral ligamentum flavum was released and subsequent decompression was done.
4) Endoscopic discectomy and end plate preparation
The endoscopic working cannula was positioned towards the traversing nerve root for visualization of discs and end plate. A radiofrequency probe was used to reveal the L4/5 disc space. Epidural veins were often noted to be adjacent to the discs and radiofrequency ablation was used for incidental venous bleeding. Ablation was also done to release adhesion between dura and the discs. During ablation and discs preparation, the working cannula was directed 180° away from the traversing nerve root for nerve protection. An annulotomy was then performed using the ablation probe. Discectomy and end plate preparation were achieved using a drill and the ablation probe was used to differentiate between the cartilaginous endplate and the subchondral bone. The direct endoscopic visualization provided the surgeon with a clear view on the end plate throughout the entire procedure. After end plate preparation, the endoscope was retracted and dilatation was sequentially executed through a custom-made working cannula. Throughout the procedure, an accessory portal was placed via an incision 3 cm caudal to the primary incision (Figure 1). A 30°/4.3-mm endoscope was utilized to observe the traversing root throughout the entire procedure.
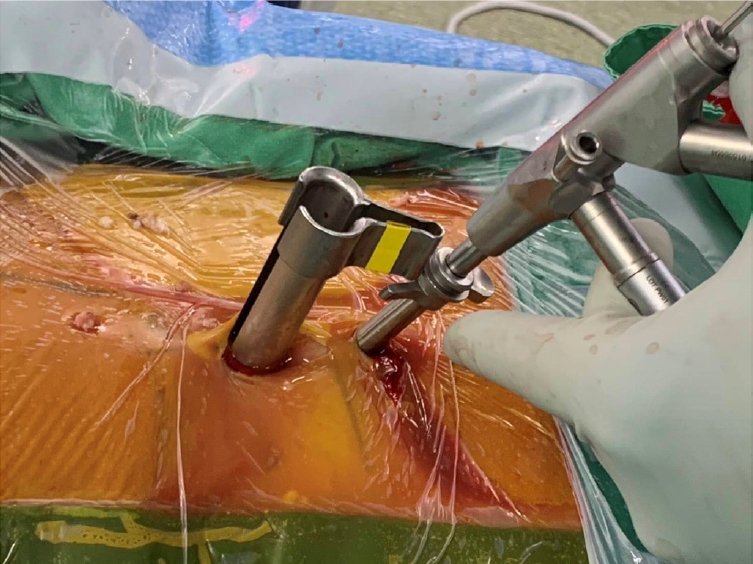
Photograph of an accessory portal made via an incision 3 cm caudal and ipsilateral to the primary incision.
The autograft was then mixed with an allograft and subsequently placed into a porous interbody cage. Using fluoroscopic guidance, an optimally sized bone-laden cage was placed into the disc space. The endoscope was reintroduced to assess the cage's alignment with the end plates and the posterior aspects of the vertebral walls. A successful decompression was determined as pulsations seen from both the traversing and exiting nerve roots under the influence of endoscopic hydrostatic pressure. After achieving hemostasis, a drain was placed above the facet level, and its placement was verified using endoscopy.
5) Percutaneous instrumentation under fluoroscopic guidance
To restore lordosis, the height in the Wilson frame was adjusted, and percutaneous pedicle screw fixation was performed. The proximal pedicle screws were set deeper relative to the distal screws to further reduce spondylolisthesis.
6) Postoperative care
Patients typically began mobility rehabilitation on the following day depending on pain tolerance. Initial physiotherapy exercises included bedside static quadriceps activities and ankle pumps. Drains were generally removed between postoperative days 1 and 2.
RESULTS
A total of 20 patients were recruited for this study, and all patients were informed of the insertion of an accessory portal for observation of traversing root injuries. In this study, there were 2 females and 18 males. The mean age was 45 years old with a mean duration of symptoms of 24 months. All patients had unilateral symptoms with lower back soreness, tenderness and range of motion limitations. Almost all of the patients had sciatica, nerve root signs and radiating pain. There were no reported complications and no reoperations during the follow-up period. Furthermore, all of the patients had underwent conservative treatments such as back bracing, oral analgesia and localized injections but to no avail.
Figure 1 showed an intraoperative image of the location of our accessory portal, which was placed approximately 3 cm caudal and ipsilateral to the working cannula. A 30°/4.3-mm endoscope was utilized to observe the traversing root during disc preparation and cage implantation to observe for traversing root injury during endo-TLIF. Representative images were captured from the accessory portal and as shown in Figure 2. Figure 2A showed docking of the working cannula after bony decompression, and the intact ligamentum flavum could be seen on the lateral side of the channel. As seen from Figure 2B, a bipolar could be inserted and used for release of ligamentum flavum and dura. After dissection of the ligamentum flavum, the traversing root could be clearly observed via the working cannula. Prior to this study, a Kirschner wire was routinely inserted between the traversing root and bony component to protect the traversing root during disc preparation as seen in Figure 2C. Figure 2D showed postinsertion of cage with no traversing root injury throughout the preparation and insertion process. Figure 2E showed an image of the contralateral traversing root which could be released from the working cannula without affecting the traversing root.
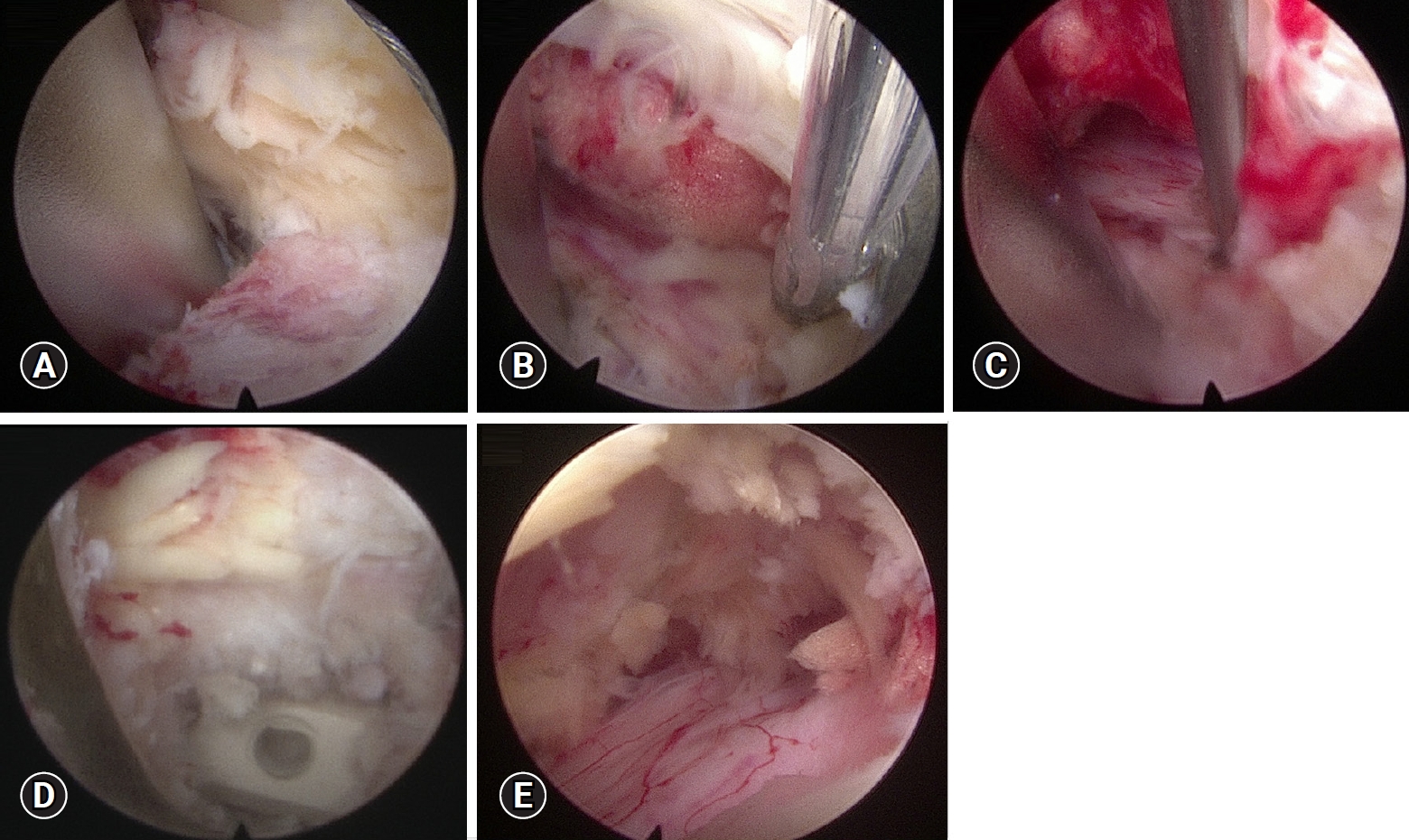
(A) Docking of the working cannula with an intact ligamentum flavum on the lateral side of the channel. (B) Bipolar forceps were used to release the ligamentum flavum and dura mater, and the traversing root could be directly observed via the working cannula. (C) A Kirschner wire was inserted between the traversing root and bony component to protect the traversing root during disc preparation. (D) Successful cage implantation was conducted via the working cannula with no traversing root injury, and (E) the contralateral traversing root could be released and observed from the contralateral working cannula.
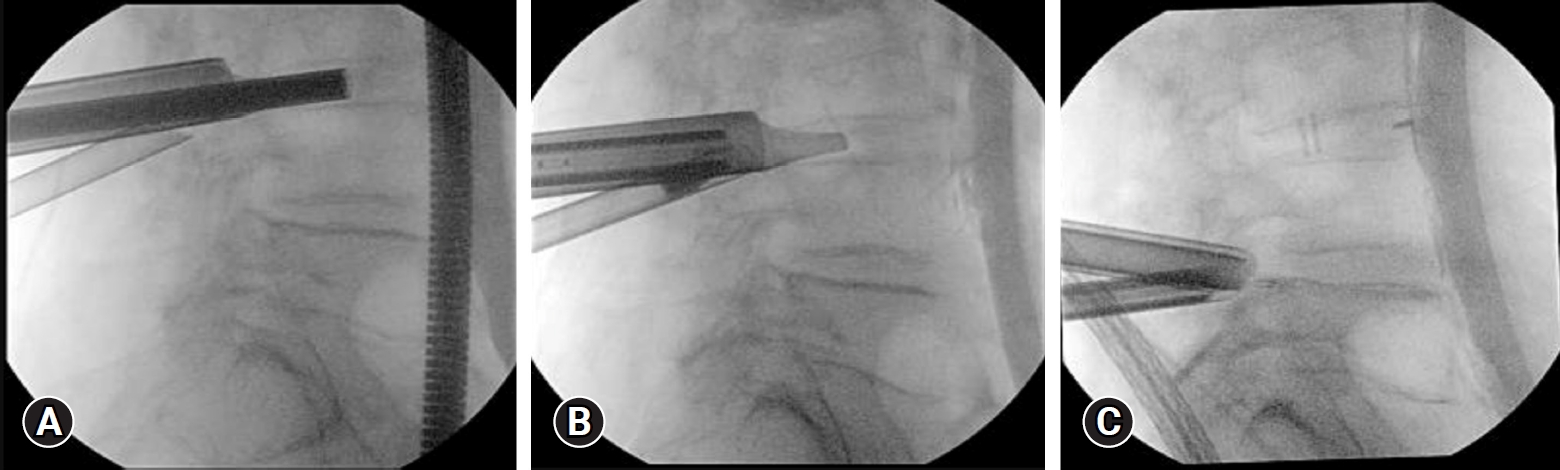
Figure 3 showed representative intraoperative fluoroscopic images of discs preparation and preparation.
DISCUSSION
The safety of endo-TLIF with regards to the traversing nerve root is a crucial consideration in fusion surgeries. Kim et al. first introduced this technique in a technical note in 2020 [6]. The main aim of this technique was to improve access to the disc space for thorough decompression and insertion of larger cages, which had been proven and published by Kim et al. [7] in subsequent publications. This was also observed and confirmed from our accessory viewing port as seen from our results. Recently, case reports and series were published emphasizing on the good functional outcomes and recoveries of patients with scoliosis and for patients undergoing fusion surgeries [7,8]. In all the publications, there were no reported complications regarding traversing nerve root injuries. As this is an apparently newer technique, there are currently no statistics regarding risks of traversing nerve root injuries. Therefore, our team sought to observe for risks of traversing nerve root injuries during endo-TLIF from an accessory portal. From our study, it could be observed that endo-TLIF had sufficient working window and space for disc preparation and cage insertion, and that it poses a very low risk to traversing nerve root injury. Prior to this study, our standard operating procedure included inserting a Kirschner wire in between traversing nerve root and bony component for protection of nerve root. However, it was observed that with careful manipulation and removal of facet joint, we can reduce risks of traversing nerve root injuries. Furthermore, after removal of facet joint, there was ample working space for instruments manipulation. With direct visualization provided by endo-TLIF, we were also able to reduce risks of traversing nerve root injuries.
CONCLUSION
Endo-TLIF was shown to be a suitable method for discs preparation and cage implantation. However, there were concerns regarding risks of traversing root injuries during endo-TLIF. In this study, we observed for risks of traversing root injuries via an accessory portal in 20 patients undergoing endo-TLIF. Our observations showed that endo-TLIF is a safe approach and method for decompression, discs preparation and cage implantation for various types of patients.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgements
We would like to thank China Medical University Hospital, Taichung, Taiwan for their support in this work.