Full Endoscopic Paramedian Partial Lumbar Corpectomy for a Lumbar Burst Fracture With Spinal Canal and Foraminal Stenosis: A Case Report With a Technical Note
Article information
Abstract
Burst fractures are common in thoracolumbar spinal injuries, often resulting in vertebral collapse with or without neurological deficits. While traditional open surgery is the standard approach for surgical decompression, it has some drawbacks and complications. Conversely, full endoscopic spine surgery remains underexplored for these patients. This case report presents a 77-year-old patient with an L3 burst fracture and severe neurological deficits caused by retropulsion bone fragments, leading to spinal canal compromise and right L3–4 foraminal stenosis. The patient underwent a full endoscopic paramedian approach for partial lumbar corpectomy and foraminal fragment removal. Vertebroplasty and short-segment pedicle screw fixation were also performed to restore sagittal alignment and spinal stability. After surgery, the patient experienced significant improvements in pain, numbness, and muscle strength. Radiographic assessments confirmed successful correction of the deformity and decompression of the spinal canal. The study emphasizes the benefits of endoscopic techniques in enhancing patient recovery for burst fractures. However, certain limitations are acknowledged, including the need for further research and expertise in utilizing this approach. In conclusion, paramedian endoscopy shows promise as a valuable alternative to traditional open surgery, offering potential advantages in terms of complications and recovery for burst fracture management.
INTRODUCTION
Burst fractures account for 15% of all thoracolumbar spinal injuries and typically result from high-energy trauma such as traffic accidents and falls from heights [1,2]. Additionally, with the aging society, the incidence of osteoporotic vertebral burst fractures is also increasing [3]. This type of fracture is caused by flexion of the spine, which exerts a compressive force on the anterior and middle columns of the vertebrae, resulting in the collapse and fragmentation of the vertebra into multiple small pieces. In certain circumstances, when the bone fragments are pushed posteriorly into the spinal canal, they can cause damage to the neural structures, leading to neurological deficits. The extent and seriousness of these deficits, including conditions such as incomplete weakness, paraplegia or cauda equina syndrome, depend on the level and severity of the injury. Treatment options range from conservative measures like pain management, bed rest, and bracing, to more invasive procedures such as vertebroplasty and pedicle screw fixation (PSF). However, in cases where the irreducible retropulsion fragments lead to persistent or worsening neurological symptoms, more extensive interventions like open decompression or corpectomy may be required [4]. Traditional open surgeries, regardless of the approach used (anterior, posterior, or combined), have disadvantages such as significant blood loss, a high rate of complications and infection [5].
Full endoscopic spine surgery has gained popularity in recent years [6], but its application in burst fractures has been limited in the literature. This article demonstrates the utilization of spine endoscopy through a paramedian approach for direct decompression in a case of burst fracture with concomitant central and foraminal stenosis. By presenting our findings, we seek to contribute valuable insights into the potential benefits of employing full endoscopic techniques in treating burst fractures, with a focus on optimizing surgical outcomes and promoting efficient patient recovery.
SURGICAL TECHNIQUE
1. Case Presentation
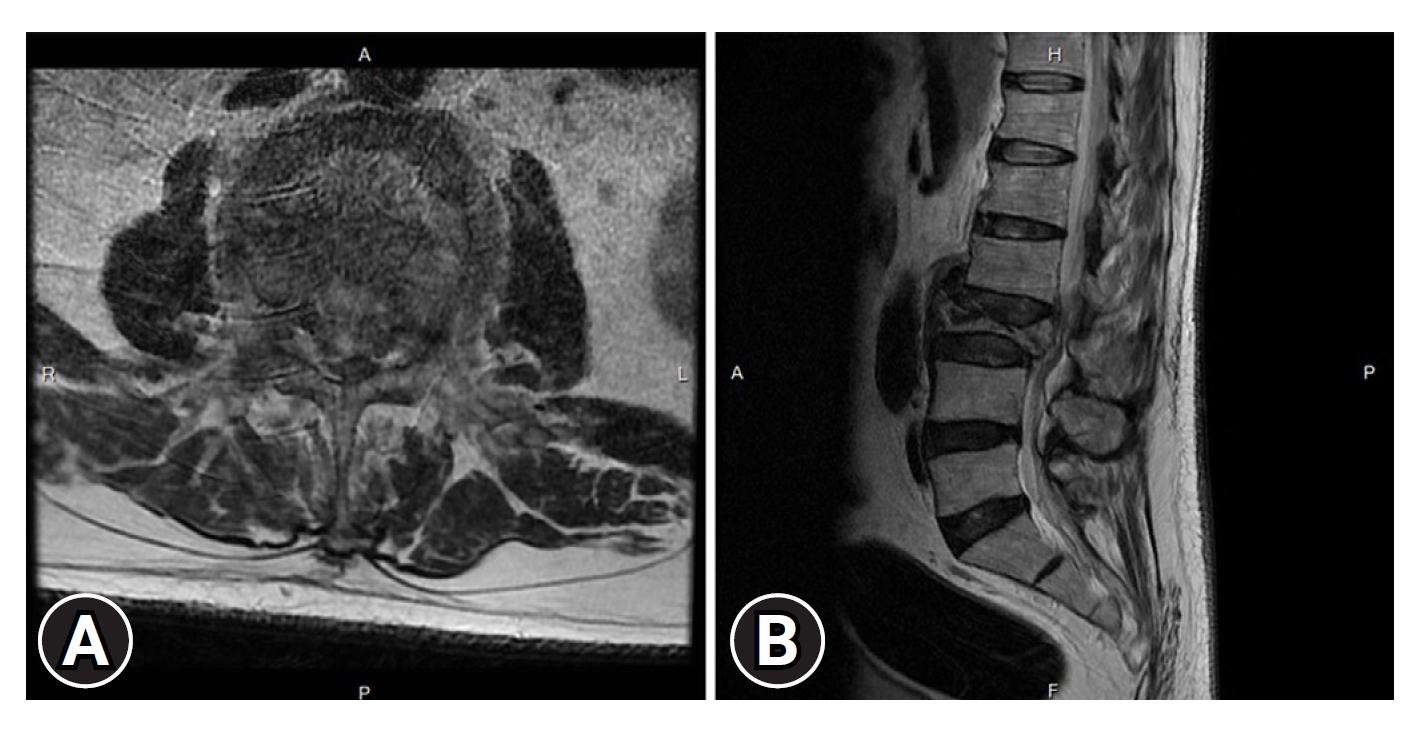
A 77-year-old male presented to the orthopedic outpatient clinic with progressive low back pain following a recent fall 4 weeks ago. He also reported worsening weakness in both lower limbs, with the right side being more severe. Additionally, he experienced progressive numbness and worsening weakness in both lower limbs, with the right side being more severe as well. Upon examination, the patient was unable to stand up independently. The muscle strength in the right lower limb was graded as 2/5, while the left lower limb was graded as 3/5. Radiography of the lumbar spine revealed a burst fracture of the L3 vertebra with a noticeable collapse in vertebral height (Figure 1A). The computed tomography (CT) further showed retropulsion bone fragments causing spinal canal compromise (Figure 1B). Additionally, one fragment was identified at the right L3–4 foramen, resulting in foraminal stenosis and right L3 nerve root entrapment (Figure 1C). The magnetic resonance imaging revealed severe compression of the dural sac at the L3 vertebral body (Figure 2A), along with disruption of the posterior longitudinal ligament (PLL) (Figure 2B). Supraspinous ligament and interspinous ligament injuries were also suspected. The patient was diagnosed with a L3 burst fracture involving both endplates and the posterior vertebral wall, classified as Denis type IIA and Magerl type A3.3 [2,7]. Based on the Thoraco-Lumbar Injury Classification and Severity Score [8], the patient obtained a score of 6 due to the presence of a burst fracture with nerve root entrapment and suspected posterior ligamentous complex injuries. Surgical treatment was recommended, involving a comprehensive approach that combines spine endoscopy through a paramedian approach to directly remove the retropulsion fragments in the spinal canal and at the right L3–4 foramen, along with the utilization of vertebroplasty and short-segment PSF to correct and maintain sagittal alignment and spinal stability.
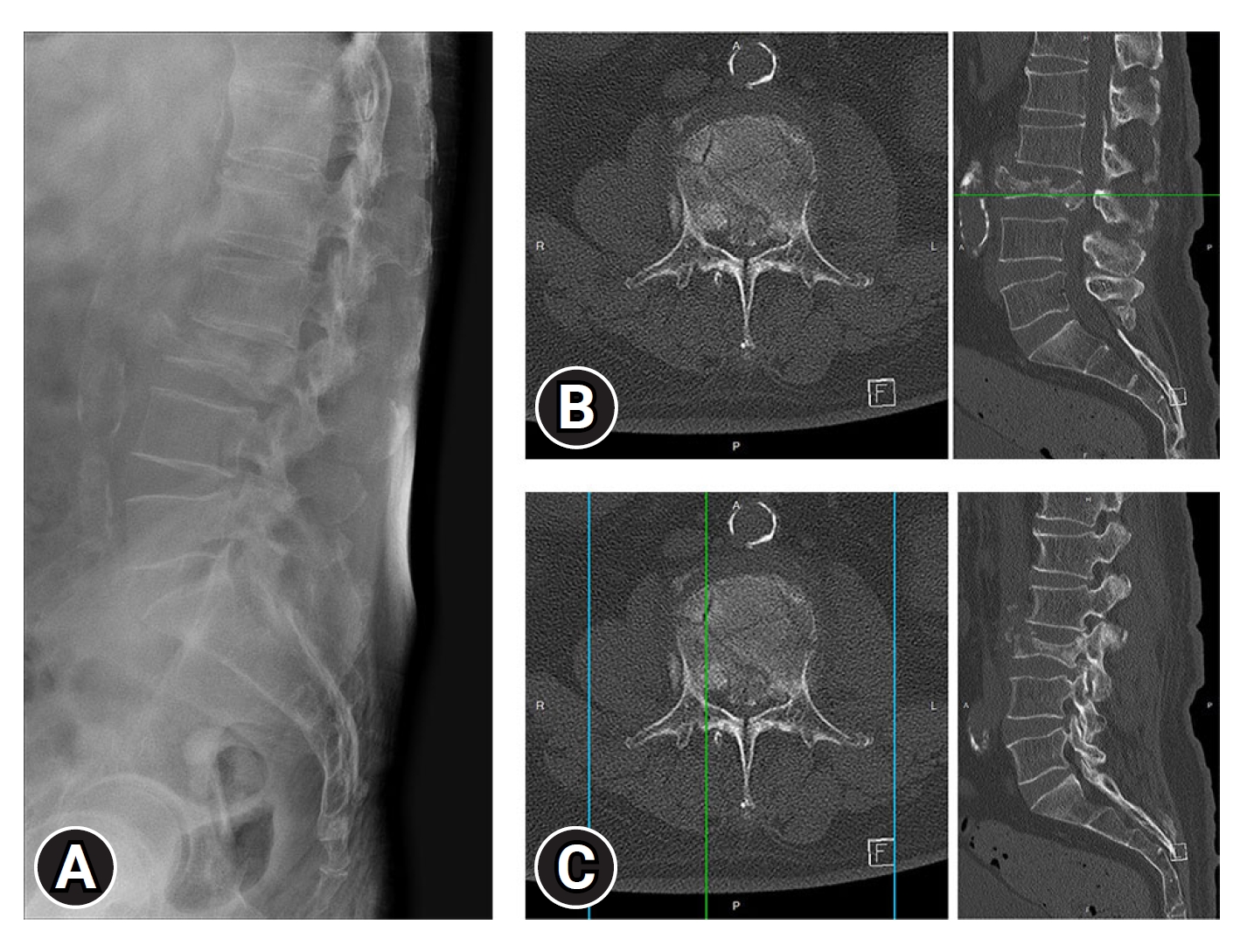
(A) Preoperative lateral radiograph indicates a burst fracture of the L3 vertebra with a noticeable collapse in vertebral height. (B, C) Preoperative computed tomography images show retropulsion bone fragments causing spinal canal compromise and one fragment at the right L3–4 foramen, resulting in foraminal stenosis and right L3 nerve root entrapment.
2. Operation Technique
Under general anesthesia, the patient was placed in a prone position on the Allen Spine System frame, ensuring proper padding of all pressure points. Following skin preparation and draping, the initial step involved performing percutaneous reduction by gradually applying anterior-directed force on the low back at the L3 vertebral level. Subsequently, PSF and vertebroplasty were carried out to correct deformity, restore vertebral height, and achieve spinal stability, thereby facilitating indirect decompression of the spinal canal. Under C-arm fluoroscopy guidance, 4 cannulated screws (65–50 mm) were inserted into the pedicles of L2 and L4 through mini-open Wiltse approach, and cement augmentation was performed for each screw. Vertebroplasty was then applied through the left pedicle of the L3 vertebra. To provide initial stability during endoscopic decompression, a rod was inserted and secured to the left-side screws (Figure 3A).
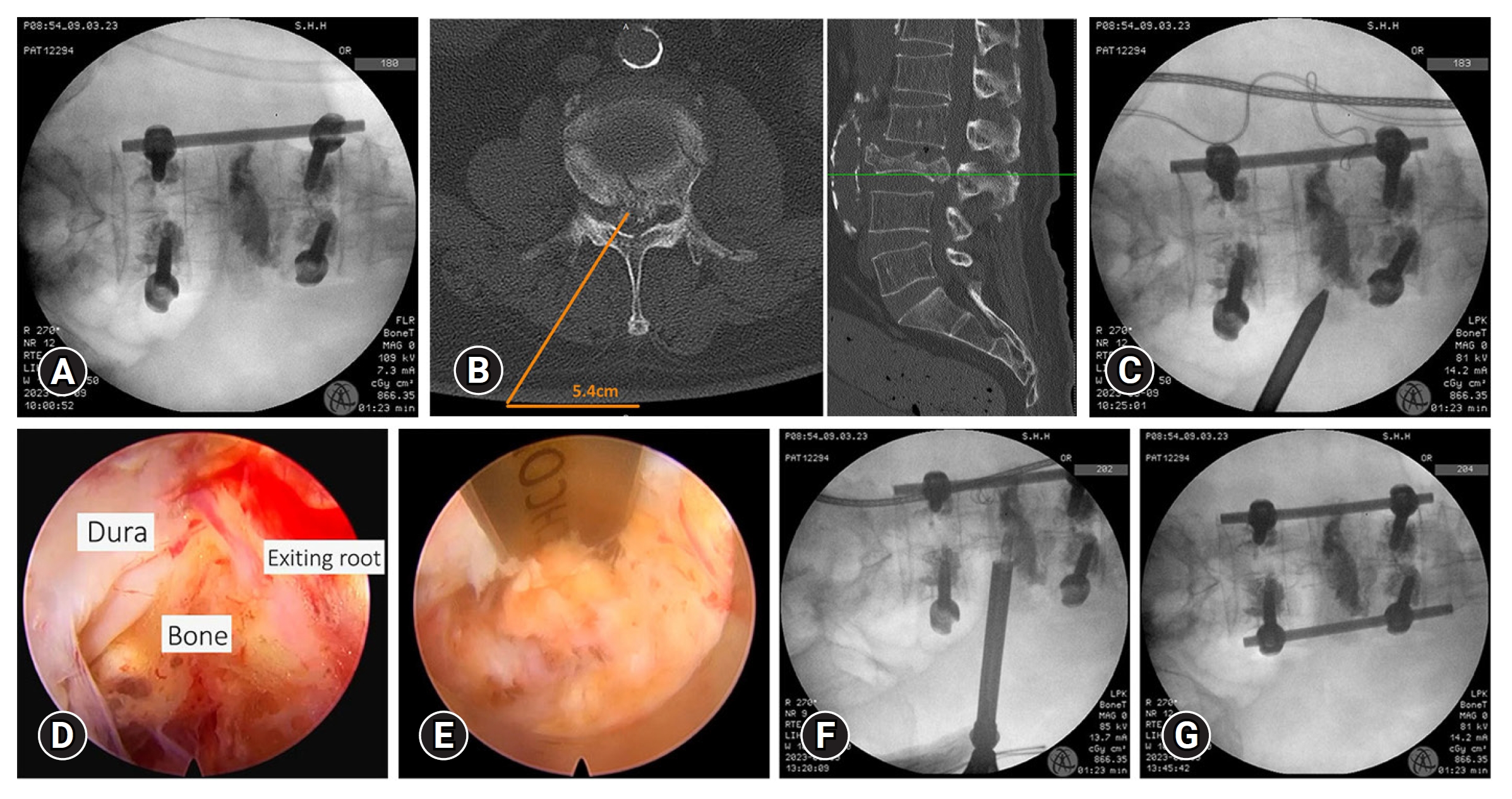
Intraoperative fluoroscopy images and views of the full endoscopic paramedian approach. (A) Pedicle screw fixation and vertebroplasty were carried out first to correct deformity and restore vertebral height to facilitate indirect decompression of the spinal canal. (B) The planned entry point for the spine endoscope on preoperative computed tomography, specifically targeting the protruded bone chip through the intermuscular plane between the longissimus and iliocostal muscles. (C) An intraoperative fluoroscopy image demonstrates the docking of the spine endoscope at the right-side L3–4 facet joint with a slightly cephalic trajectory towards the L2 vertebral body. (D) The posterior-pushed bony fragments were located in the axilla region of the L3 nerve. (E) The fragments were carefully dissected into smaller pieces using a root retractor and subsequently removed using a disc rongeur. (F) An intraoperative fluoroscopy image displays the final extent of the partial corpectomy. (G) Following the endoscopic decompression procedure, bilateral rods were fastened.
The endoscope system used was the TCEHORD (Daejeon, Korea) Percutaneous Stenoscopic Lumbar Decompression (PSLD) system, which had a working channel diameter of 5.7 mm, an outer diameter of 8.4 mm, a working length of 120 mm, and a lens angle of 12°. The entry point for the spine endoscope was planned on CT, targeting the protruded bone chip, through the intermuscular plane between the longissimus and iliocostal muscles. A transverse skin incision measuring 1 cm in length was made, located 5.4 cm lateral to the midline at the L3–4 disc level (Figure 3B). The spine endoscope was docked at the right-side L3–4 facet joint with a slightly cephalic trajectory towards the L3 vertebral body (Figure 3C). To avoid the risk of iatrogenic cauda equina syndrome, the initial bony procedures, including right hemilaminectomy and foraminoplasty, were performed first. This was followed by the removal of ligamentum flavum and bony chips in the foramen and epidural space. Subsequently, the L3 nerve root and dural sac were identified. The posterior-pushed bony fragments were located in the axilla region of the L3 nerve (Figure 3D). They were carefully dissected into smaller pieces using a root retractor and subsequently removed using a disc rongeur (Figure 3E). The final extent of the partial corpectomy was verified using a C-arm based on the preoperative CT findings (Figure 3F). Following the endoscopic decompression procedure, the right-side rod was inserted and securely fastened, followed by retightening of the left-side rod (Figure 3G). A Jackson-Pratt drain was inserted at the endoscopic wound, and all skin incisions were closed. The total operating time for the procedure was 5.2 hours, and the estimated blood loss was approximately 50 mL.
3. Result
After the operation, the patient was instructed to wear a lumbosacral corset for 3 months. On postoperative day 1, physical examination showed significant improvement in low back pain and bilateral lower limb numbness. The muscle strength in the right lower limb improved to 3/5, and the left lower limb improved to 4/5. The patient was able to walk with the assistance of a walker, albeit with a slow pace and limited distance. Postoperative lateral radiograph revealed restored sagittal alignment and the height of the L3 vertebra (Figure 4A). The patient was successfully discharged on the sixth day after surgery and participated in a postacute care rehabilitation program for 2 weeks. At the 2-month follow-up, the surgical wounds had healed without any complication (Figure 5A), and the patient experienced complete resolution of low back pain and lower limb numbness. Bilateral lower limb muscle strength returned to baseline, and the patient was able to walk independently without the need for assistive devices (Figure 5B). Follow-up radiographs indicated intact screws without any signs of breakage and maintained sagittal plane alignment (Figure 4B). CT scans in the sagittal view revealed a well-reduced wedge angle and regional kyphosis angle, indicating successful correction of the deformity. The sagittal view also confirmed the removal of the retropulsion fragment at the right foramen (Figure 4C). Furthermore, the axial view demonstrated the extent of hemilaminectomy, foraminoplasty and partial corpectomy, providing evidence of adequate decompression of the spinal canal (Figure 4D).
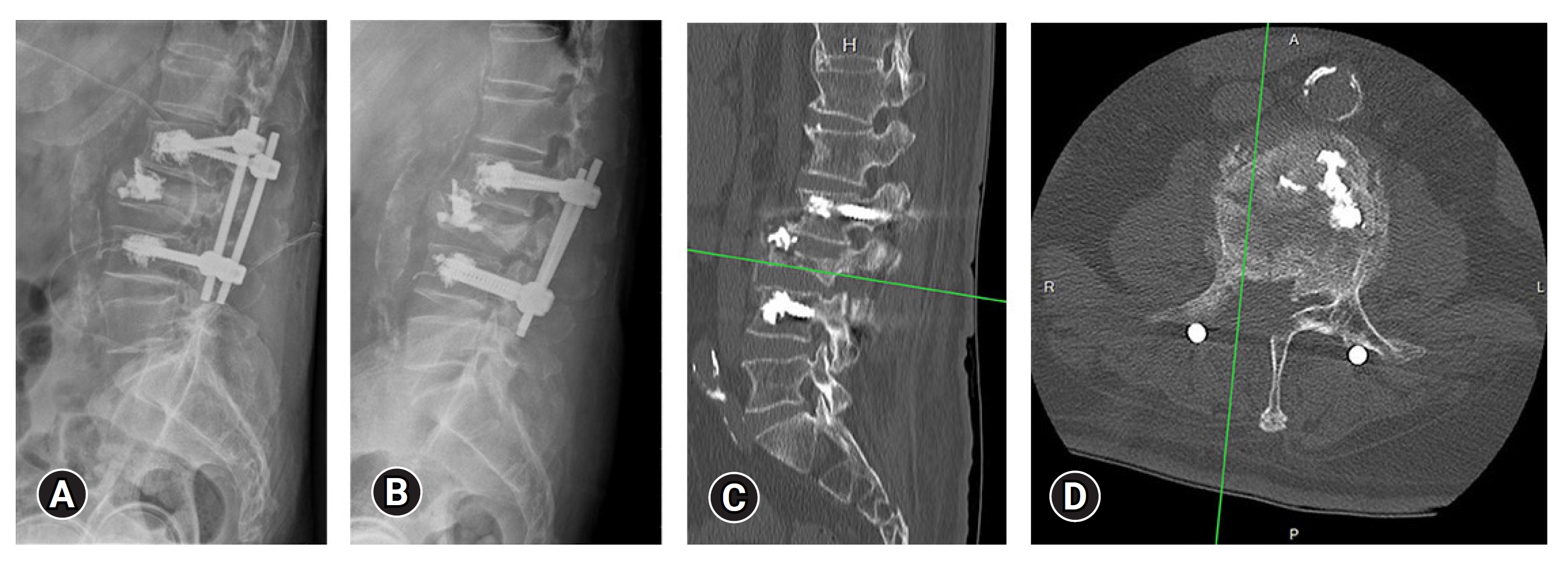
(A) A postoperative lateral radiograph reveals restoration of sagittal alignment and the height of the L3 vertebra. (B) Two-month follow-up radiograph indicated intact screws without any signs of breakage and maintained sagittal plane alignment. (C, D) Two-month follow-up computed tomography images show the removal of the retropulsion fragment at the right foramen and the extent of hemilaminectomy, foraminoplasty, and partial corpectomy, providing evidence of adequate decompression of the spinal canal.

(A) Photograph of the patient's surgical wounds. (B) At a 2-month follow-up, the patient demonstrated independent ambulation without the use of assistive devices.
Written informed consent for publication of patient’s image has been obtained.
DISCUSSION
In this study, we report the pioneering use of a full endoscopic paramedian approach for posterior corpectomy and removal of foraminal fragments in the treatment of a lumbar burst fracture with concomitant central and foraminal stenosis, leading to severe neurological deficits. Managing lumbar burst fractures requires careful consideration of factors such as fracture type and stability, patient health, and comorbidities [4]. Preoperative assessment is vital for selecting the most suitable surgical approach. The main surgical objectives include restoring vertebral height, correcting kyphosis, decompressing the spinal canal, preventing additional spinal cord injury, and promoting neurological recovery.
In cases with intact PLL, indirect reduction of the retropulsion fragment can be achieved through ligamentotaxis, and PSF alone is then used to stabilize and realign the fractured vertebra [9,10]. While percutaneous PSF (PPSF) is a well-established technique, PSF through the mini-open Wiltse approach remains a valuable alternative with demonstrated advantages over PPSF in meta-analyses, including shorter learning curve, reduced facet joint violation, and decreased operative time [11]. Although stand-alone vertebroplasty in thoracolumbar trauma is controversial, combining it with PSF has shown promise in restoring vertebral body height, supporting the anterior column, and preventing correction loss and implant failure [12,13]. This combination allows for short-segment fixation instead of long-segment fixation, which preserves more motion segments and is particularly valuable for certain elderly patients [14].
For patients with retropulsion fragments that cannot be reduced by indirect reduction, resulting in persistent or worsening neurological symptoms despite isolated PSF, surgical decompression and removal of the bone fragments are necessary to address the issue [4]. The neurological deficits in these cases are commonly attributed to compression on the ventral surface of the spinal cord. While an anterior approach intuitively provides more direct decompression compared to the posterior approach and potentially facilitates better neurological recovery, studies have found that for thoracolumbar burst fractures, the choice between anterior or posterior approach does not significantly impact clinical outcomes [4,15]. However, traditional open surgeries, regardless of the approach employed (anterior, posterior, or combined), can result in significant blood loss, a high incidence of complications and infections, and a prolonged recovery period that delays the resumption of normal daily activities [5]. Maciejczak et al. [16] proposed a minimally invasive posterior keyhole corpectomy technique, which offers the advantage of reducing approach-related morbidity. However, even with the removal of the pedicle and the utilization of a specialized retractor system, this approach still has limitations in terms of visualization of the surgical field. In recent years, full endoscopic spine surgery has gained popularity due to its excellent visualization, minimal tissue disruption, reduced blood loss, and decreased postoperative pain [6]. It provides a direct view for decompression, allowing surgeons to precisely address spinal pathologies. In the existing literature, 2 case reports describe the application of transforaminal endoscopy for performing corpectomy in patients with burst fractures [17,18]. However, when the retropulsion fragments present around the foramen, performing foraminoplasty and directly extending the distal end of the cannula to the posterior end of the vertebral body can be challenging and may pose an increased risk of nerve root injury. The full endoscopic paramedian approach was introduced with the advantage of effectively addressing foraminal and extraforaminal lesions [19]. To our knowledge, this is the first report describing the use of the paramedian approach with hemilaminectomy and foraminoplasty to simultaneously address fragments in the foramen and spinal canal in burst fracture patient with neurological deficits. This approach offers advantages such as enhanced visualization, thorough decompression, and minimized soft tissue disruption, making it a viable alternative to previously described approaches.
However, it is important to acknowledge that our report has certain limitations. Firstly, the report includes only one patient with a fracture at the L3 level, and the patient was in the subacute stage (4 weeks posttrauma), rather than the acute stage. Further practice and research are needed to determine if this approach can be applied to higher-level fractures and in the acute stage. Secondly, this approach may not be suitable for all lumbar burst fractures due to the trajectory angle of the working cannula. The choice of approach needs to consider the location of the retropulsion fragments. Lastly, in addition to the equipment and resource requirements for spine endoscopy, the technical complexity of this approach demands a high level of expertise, and the initial operation time may be longer with a steep learning curve. However, once proficiency is achieved, the overall blood loss is minimal, and the whole procedure can be performed under local anesthesia, making it a favorable choice for elderly patients or those with multiple comorbidities.
CONCLUSION
In conclusion, the utilization of full endoscopic paramedian approach with laminectomy, foraminoplasty, and partial corpectomy is a valuable technique for simultaneously addressing fragments in the foramen and spinal canal in burst fracture patients with neurological deficits. This technique offers a favorable alternative to the traditional open approaches with the potential advantages of fewer approach-related complications and a faster recovery. However, further research and clinical studies are needed to validate the applicable level and assess the effectiveness and safety of this technique.
Supplementary Material
Supplementary video clip 1 can be found via https://doi.org/10.21182/jmisst.2023.00906.
Supplementary video clip 1.
The step-by-step procedure of the full endoscopic paramedian approach with hemilaminectomy and foraminoplasty to simultaneously address fragments in the foramen and perform partial corpectomy.
Notes
Conflicts of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.