Comparative Study of the Outcomes of Endoscopic Unilateral Laminotomy for Bilateral Decompression (ULBD) With Destandau Technique and Microscopic ULBD: A Randomized Double-Blinded Study of 685 Patients
Article information
Abstract
Objective
Lumbar canal stenosis is a common finding amongst elderly patients visiting spine surgeons for back pain. Uniportal unilateral laminotomy for bilateral decompression (ULBD) is an emerging minimally invasive procedure for lumbar canal stenosis. This study compared the clinical outcomes of endoscopic ULBD with Destandau technique and microscopic lumbar canal decompression.
Methods
A prospective multicenter study on 685 patients undergoing single-level spinal canal decompression. Patients with axial back pain, lumbar radiculopathy, lumbar canal stenosis & claudication distance <1,000 m were included. Parameters assessed were Dura expansion, thecal sac’s cross-sectional area, horizontal displacement, blood loss, operation time, hospital stay, modified MacNab score, visual analogue score (VAS), side changing (self) status, Oswestry Disability Index (ODI), and the Short-Form 36 for quality of life (QoL).
Results
Group 1 (endoscopic ULBD with Destandau technique) had 343 patients and group 2 (microscopic ULBD) had 342 patients. Group 1 had lower horizontal displacement (0.34%±0.21%, p<0.001) and significant improvement of VAS (42.28%±3.20%, p<0.001) at 1-week postsurgery with shorter hospital stay (1±0.2 days vs. 1.8±0.8 days, p<0.01) and significant improvements of ODI and MacNab scores (42.28±3.20 and 85.30%, p<0.001). The 30-second chair test (3.4±0.13 vs. 5.6±2.41, p<0.001), 10-meter walk test (1.0±2.15 vs. 0.55±3.23, p<0.001), and SF-36 physical health component score (48.20±8.46 vs. 74.48±0.54, p<0.001) improved significantly as well. Furthermore, 92% of patients were able to change sides while in bed at 1-week postsurgery. Claudication distance improved significantly in both groups.
Conclusion
Group 1 patients had better clinical and functional outcomes within 3 months of surgery than group 2 patients, with improved QoL, shorter hospital stays, claudication distance, and self-side changing ability.
INTRODUCTION
Spinal canal stenosis remains the most common indication for spine surgery in elderly [1]. Patients with degenerated spine and neurological symptoms often have dysfunction [2], dissatisfaction and poor quality of life (QoL). Their output in daily routine activities suffer, rendering them dependent on others for assistance.
Patients with spinal canal stenosis often present with back pain and radiating pain. Treatment options range from medications to surgery. Recently minimal invasive techniques like unilateral laminotomy for bilateral decompression (ULBD) performed using endoscope system or microscope are being preferred [3]. The newer techniques involve use of enhanced optics, instrumentation, and artificial intelligence [4], thereby improving precision and limited tissue dissection. Research articles have reported early clinical recovery with endoscopic procedures, but studies comparing ULBD performed by with endoscopic system (Destandau technique) and microscope are very few.
Spine instability and back pain have been reported post microscopic ULBD [5]. Endoscopes on other hand offer excellent magnification, illumination and 4K clarity through a single portal. It is important to assess patient-related outcome scores to understand the impact of surgical procedure on patient’s QoL.
This study was initiated to compare the clinical outcomes (surgical timing, blood loss, hospital stay, MacNab scores, Oswestry Disability Index (ODI), 36-item Short Form health survey [SF-36] scores, and complications) in patients undergoing spinal decompression performed by endoscope with Destandau technique and microscopes. Secondly to document patient specific parameters like visual analogue score (VAS), QoL, side changing ability postoperatively.
MATERIALS AND METHODS
A prospective multicenter study performed at 3 centers in Bhubaneswar, India from May 2012 to February 2019 on 685 patients undergoing single-level decompression for spinal canal stenosis. Patients were randomized into 2 groups; randomization was done by computer generated number.
1. Inclusion Criteria
Back pain, lumbar radiculopathy, lumbar canal stenosis (single level) with or without disc herniation, claudication distance <1,000 m, no improvement after 6 weeks conservative treatment and minimum 1-year follow-up.
2. Exclusion Criteria
Consent refusal, instability (segmental), same level surgery, extensive calcified or hard disc herniation, posterior longitudinal ligament ossification, and infection.
3. Surgical Technique
All peocedures were performed under general anesthesia and standard radiolucent operating table was used for all surgeries.
1) Group 1: modified chest knee position (Figure 1)
(A) Patient position for endoscopic unilateral laminotomy for bilateral decompression (modified chest knee position). (B) Placement of Destandau endoscopic system (Tube) with skin markings.
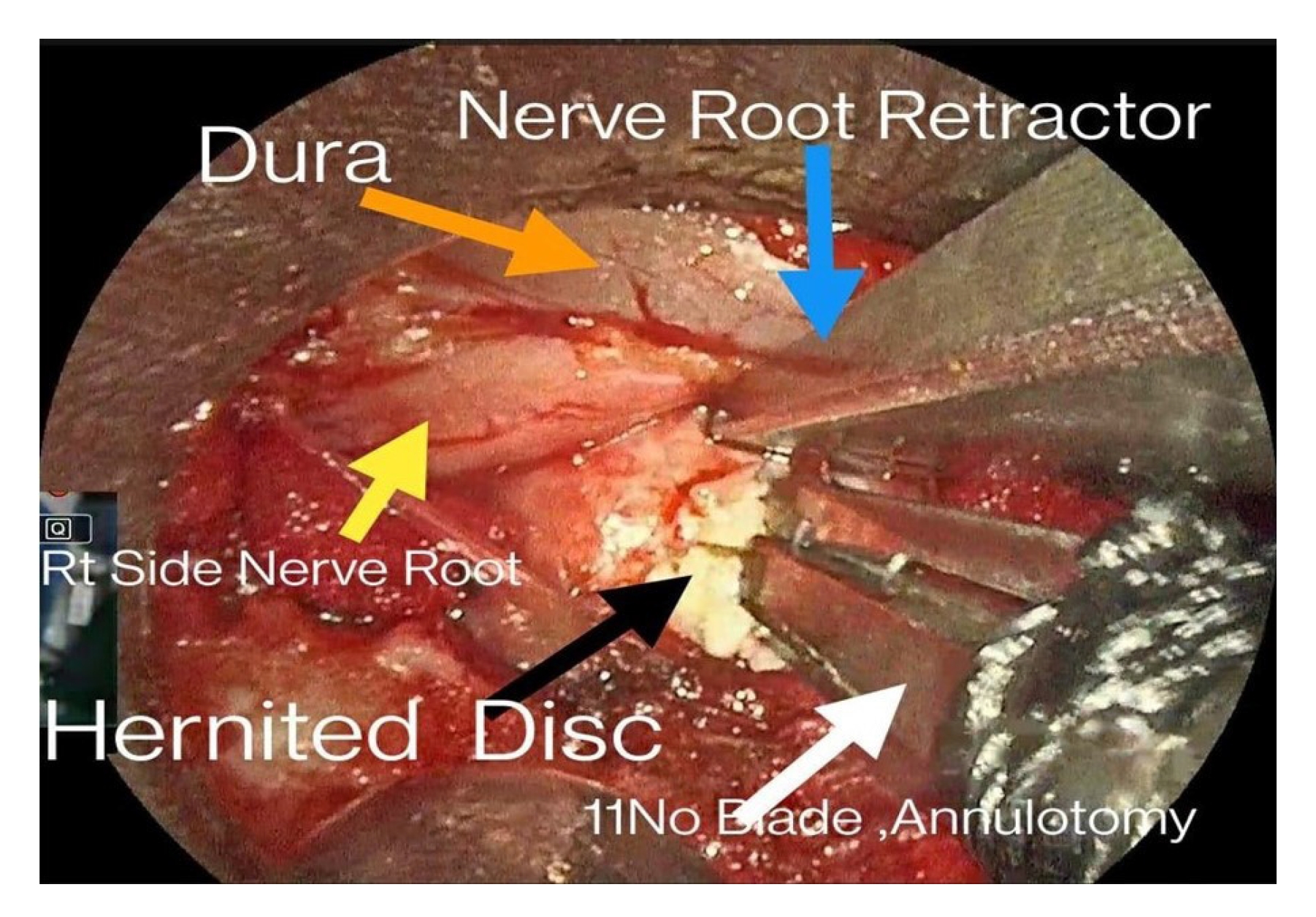
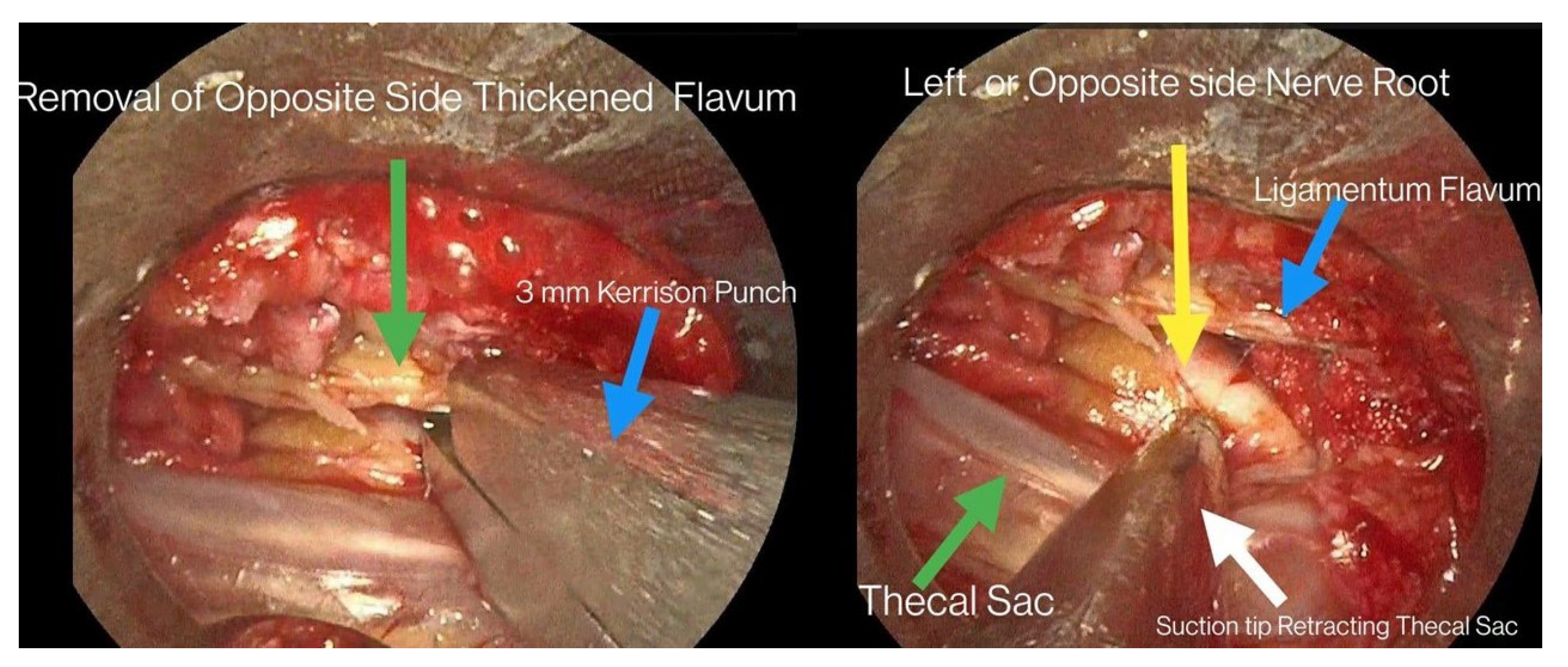
Destandau Endospine System (Karl Storz, Tuttlingen, Germany) comprising of endospine tube, trocar, and working insert was used (Figure 1). Levels were marked with use of localization device, skin incision (15–20 mm) was marked 5 mm besides midline, and Mayo scissors were used to dissect the aponeurosis. Periosteum elevator was used to dissect the paravertebral muscles from spinous process and superior lamellae to expose the interlaminar window. Laminotomy was performed under vision to expose underlying dural sac and nerve root.Discectomy was performed under vision (Figure 2), adequacy was confirmed by pushing saline and visual confirmation by endoscope in disc cavity. Further, over-the-top decompression was performed on contralateral side (Figure 3).
2) Group 2: patient placed in Wilson Frame
A 30- to 50-mm midline incision was marked. Aponeurosis along with paravertebral muscles were dissected as usual. Laminotomy was performed followed by the microscopic soft tissue decompression. Medial facet and ligamentum flavum were dissected under microscopic visualization by high-speed drill and a curette. Discectomy was performed followed by over-the-top decompression on contralateral side.
4. Randomization and Blinding Protocol
Patients were randomized into 2 groups. In group 1, ULBD were endoscope assisted, surgery performed with Destandau technique. In group 2, ULBD were microscope assisted.
The principal investigator was aware of the patient’s grouping and procedure done, did not perform the surgery or follow-up assessment himself. Surgeons performing the surgery did not know about the patient’s grouping. Doctors performing follow-up assessment were unaware of patient grouping and procedure performed.
5. Parameters Assessed
Authors assessed the dura expansion, thecal sac’s cross-sectional area, horizontal displacement, operation time, estimated blood loss, hospital stay, modified MacNab score, and incidence of complications in both groups.
6. Clinical Evaluation
Surgical scar condition, back pain status, radiating pain status, side changing (self) status and walking ability were assessed. VAS scores for back pain and leg pain, ODI, and SF-36 for the QoL were assessed.
7. Rehabilitation
Patients were offered bed rest depending on patient's comfort. Active hip, knee, and ankle toe exercises (active and passive) were started on same day of surgery depending on patient's tolerance. Weight bearing was allowed from day of surgery.
8. Follow-up
Patients were discharged 1–2 days after surgery. In both groups, patients were discharged 1-2 days after surgery. Patients were followed up during their visit to hospital at 1, 3, 6 weeks and 3, 6, 12 months postsurgery.
9. Statistical Analysis
IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA) was used. Pre- and postoperative outcomes were compared by paired sample t-test. To compare clinical results between 2 groups; independent 2 sample t-test and chi-square test were used; p<0.001 was considered significant.
10. Ethical Statement
Ethical committee clearance was obtained before enrolling patients for the study (AH-2012/04-657). Written informed consents were obtained from all participants before the start of study.
RESULTS
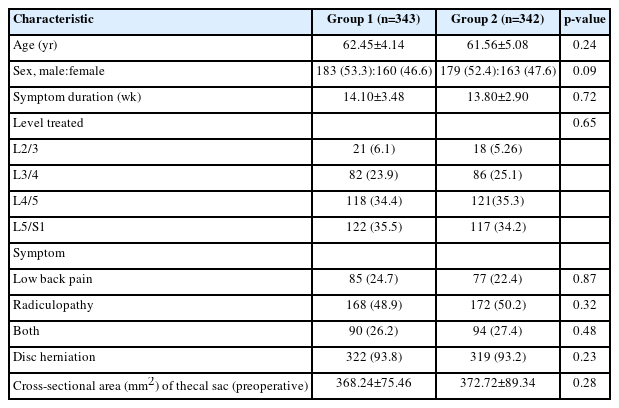
A total of 685 patients who underwent single-level spinal canal ULBD were included in this study. Endoscopic ULBD with Destandau technique (group 1) had 343 patients and microscopic ULBD (group 2) had 342 patients. The demographic and preoperative characteristics of the patients were statistically similar (Table 1).
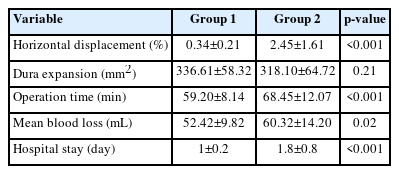
The radiologic outcomes and surgical data are shown in Table 2 and clinical outcomes are shown in Table 3. The degree of horizontal displacement was lower in group 1 than group 2 (0.34%±0.21% vs. 2.45%±1.61%, p<0.001). Postoperative pain and ODI expressed in percentage were significantly improved in both groups (p<0.001). There was a significant difference in the improvement of pain (VAS) at 1 week after operation between the groups 1 and 2 (42.28%±3.20% vs. 50.15%±6.82%, p<0.001). Authors observed a significant difference in hospital stay. Group 1 patients were comfortable and discharged early (1±0.2 vs. 1.8±0.8, p<0.01).
There was a significant difference in ODI at 1 week after operation between the groups 1 and 2 (42.28±3.20 vs. 50.15±6.82, p<0.001). However, there was no significant difference in ODI at 1 month after operation and 1 year after operation in both groups.
There was a significant difference in the modified MacNab score at 1 week after operation between the groups 1 and 2 (85.30% vs. 88.44%, p<0.001). However, the difference was not significant from 1-month to 1-year postsurgery.
There was no significant difference in dura expansion (336.61±58.32 vs. 318.10±64.72, p=0.21), operation time (59.20±8.14 vs. 68.45±12.07, p=0.04) and blood loss the groups 1 and 2 (52.42±9.82 vs. 60.32±14.20, p=0.02).
At 1-week postsurgery; there was significant improvement 30-second chair stand test results (3.4±0.13 vs 5.6±2.41, p<0.001) and 10-meter walk test (1.0±2.15 vs 0.55±3.23, p<0.001) (Table 4) values in group 1. SF-36 physical health component subscale score also had significant improvement at 1-week postsurgery in group 1 (48.20±8.46 vs. 74.48±0.54, p<0.001). Furthermore, 92% of patients were able to change sides while in bed at 1-week postsurgery. Overall QoL and patient satisfaction was better in group 1. Claudication distance improved significantly after decompression for both the groups (Table 4).
There were 22 cases (6.43%) of cerebrospinal fluid leak in group 2 and 12 (3.50%) cases in group 1, all of which were treated with conservative treatment including bed rest, fluid replacement, and medications. Surgical site infection occurred in 8 cases (2.3%) in group 2 and 5 (1.45%) in group 1 were treated with antibiotics. At 1-year follow-up, 6 patients (1.74%) in group 1 and 11 patients (3.21%) in group 2 had recurrence.
DISCUSSION
There is often a poor radiographical and clinical correlation in spine pathologies. The treatment must be tailored to accommodate patient’s needs. Patients not responding to conservative therapy warrant surgical decompression [6]. Minimally invasive surgical procedures are being done for patients suffering from lumbar canal stenosis worldwide [7].
Conventional or open decompressive laminectomy has been done over the years and is an established procedure. Although it offers better hand control and manipulative freedom; but it involves extensive soft tissue stripping and larger surgical scar. Conventional surgical management of lumbar canal stenosis has been open decompressive laminectomy. This is a useful procedure with enhanced hand manipulative control, but it involves stripping and retraction of paraspinal muscles along with removal of spinous process and lamina, this can lead to iatrogenic instability [8], adhesions [9], scarring and para spinal muscle atrophy thus persistent back pain.
Minimal invasive techniques aim at precise dissection and specific soft tissue removal, limiting removal of important structures. This allows early rehabilitation, better clinical outcomes [10] and cosmesis. Variety of surgeries are being performed using minimally invasive techniques like lumbar discectomy [11], foraminal decompression, spinal fusion, and deformity correction [12]. The patients underwent surgery with minimally invasive techniques. The advantages of minimally invasive approach undergo minimal tissue trauma, blood loss, shorter operative time, lesser hospital stays, perineural fibrosis [13,14], and have less analgesic requirement postoperatively.
Endoscopic spinal instrumentation has revolutionized spine surgeries. It offers clear magnified 4K vision, illumination, and magnification with precise soft tissue removal. Learning curve is high in endoscopic surgery due to small working channel and space, which can improve with training and experience.
In our study, patients presented with back pain, radiating pain, and combination of both. Group 1 patients had a shorter hospital stay, less blood loss, and operative time. They also had significantly better VAS scores and ODI at 1 week postoperatively. Later, scores were still better for group 1 but were not statistically significant between the 2 groups.
Significantly improved modified MacNab scores were observed in group 1 at 1-week, 1-month, and 3-month follow-ups (Table 3). At 1 year postoperatively, these scores were better for endoscopic group but not statistically significant.
At 1 week postoperatively, group 1 patients tolerated surgical procedure better and had improved functional scores (30-second chair stand test and 10-meter walk test) postoperatively with better SF-36 scores; the physical health component results were statistically significant (Table 4). However, the statistical difference between the 2 procedures was not significant in SF-36 mental health component scores.
Postoperatively; 92.65% patients could change side by themselves in group 1 as compared to 87.72% in group 2. These results could be interpreted as a significant improvement in the QoL of patients in group 1 at 1-week postsurgery. Improved claudication distance was seen in both the groups postsurgery owing to effective decompression.
CONCLUSION
Group 1 patients have better clinical and functional outcomes within 3 months of surgery compared to group 2 patients. They have improved QoL with shorter hospital stays, better SF-36 scores and self-side changing ability.
Notes
Conflicts of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.