Outpatient Fully Endoscopic Cervical Unilateral Laminotomy for Bilateral Decompression with Virtual Postoperative Monitoring
Article information
Abstract
Objective
Cervical endoscopic unilateral laminotomy for bilateral decompression (CE-ULBD) is a promising novel surgical approach. However, to date, there is a paucity of data regarding safety, efficacy, and functional outcomes following CE-ULBD.
Methods
The aim of this study was to investigate the outcomes of outpatient CE-ULBD combined with postoperative smartphone-based continuous physiological monitoring and virtual follow-up.
Results
We included a total of 23 patients in our study group. The mean age was 69.1±2.5 years. A significant postoperative reduction of the visual analogue scale for neck pain (4.1±0.6 pre- vs. 2.3±0.5 post-surgery; P<0.0001) and upper extremity pain (2.6±0.6 vs. 1.1±0.3; P=0.0012) was reported alongside a significant improvement in the Neck Disability Index (18.6±2.5 vs. 9.1±2.5; p=0.032). Eleven patients were monitored with continuous physiological monitoring via a smartphone app (SPINEhealthie). Those patients were more likely to be outpatients (p=0.0002) and less likely to have postoperative inpatient clinic utilization (p<0.0001). Continuous physiological monitoring suggested a trend towards higher levels of function in patients following CE-ULBD.
Conclusion
Our early results suggest that outpatient CE-ULBD followed by virtual postoperative monitoring is a safe and efficient therapeutic intervention for symptomatic cervical spinal stenosis.
INTRODUCTION
Spinal stenosis is present in 9% of individuals seventy years of age or older [1]. The development of spinal cord dysfunction is thought to be multifactorial, with both static and dynamic factors involved in the pathogenesis. Static factors comprise degenerative disc disease, osteophytes, facet hypertrophy, or ossification of the posterior longitudinal ligament [2]. Dynamic factors, such as repetitive flexion and extension of the spinal column during physiological body movements, cause repetitive dynamic microtrauma [3,4]. Additionally, movement and pathological interactions of the cerebrospinal fluid and the spinal cord have been reported at and beyond the level of stenosis, adding an oscillation component to the microtrauma theory [5-8]. Combined mechanical strain leads to hypoperfusion of the spinal cord, resulting in the loss of neurons and myelin through a cascade of neuroinflammatory processes and apoptosis [9,10]. Patients frequently first notice progressive loss of dexterity caused by degenerative cervical myelopathy. Besides that, neck pain, alongside sexual, bladder and gait dysfunction are common symptoms of degenerative cervical myelopathy [11].
Therapeutic approaches include conservative measures like physical and occupational therapy, cervical traction, and medication (i.e., steroids and nonsteroidal anti-inflammatory drugs) [12]. Surgical interventions have been reported to alleviate symptoms with an overall improvement in both functional and quality of life measures [13]. The general concept of all surgical approaches is the decompression of the spinal cord. Anterior discectomy and fusion (ACDF) is a well-established and effective surgical procedure. However, it is more suitable to one- or two-level pathologies, and patients may experience transient or permanent dysphagia after surgery [14,15]. Open posterior decompression and fusion as well as laminoplasty are other treatment options that address posterior pathologies effectively. Disadvantages of these procedures include significant blood loss, wound healing issues, non-union and persistent neck pain [16]. Full endoscopic spine-surgery (FESS) on the other hand presents a minimally invasive alternative to the aforementioned procedures [17]. While FESS has been described as efficacious and safe, especially with regards to an aging population [18] data supporting it as an effective mean for cervical spine decompression remain scarce. We previously reported on a novel FESS technique to decompress the spinal cord via a unilateral laminotomy for bilateral decompression (CE-ULBD) [19], allowing the surgeon to achieve a bilateral decompression through a unilateral laminotomy [20].
The scope of this paper was to further define the safety, efficacy, and objective functional impact (stepping data) of CE-ULBD. Additionally, we aim to present our early experience with virtual follow-up and asynchronous patient-provider communication using a novel smartphone application (SPINEhealthie).
MATERIALS AND METHODS
For this retrospective analysis, we included patients receiving CE-ULBD for symptomatic single- or multilevel central canal stenosis at the Department of Neurological Surgery at the University of Washington. Patients of >18 years were included when reporting preoperative neck pain and/or other symptoms of cervical myelopathy comprising loss of dexterity, gait dysfunction, sexual and/or bladder dysfunction, and radiating upper extremity pain alongside confirmation of central canal stenosis through magnetic-resonance-imaging (MRI). Patients reporting sole upper extremity pain and patients with foraminal stenosis were not considered for CE-ULBD. Patients gave written and informed consent preoperatively. Outcome measures were acquired through the SPINEhealthie application as well as the electronic patient chart. Relevant parameters were predefined and reviewed. They consisted of the patients’ demographics, patient-reported outcome measures (PROMs), imaging, and operative details. PROMs consisted of a visual analogue scale (VAS) for both neck and upper extremity pain [21], as well as the Neck Disability Index (NDI) [22]. In example, patients using SPINEhealthie get a reminder through their smartphone to report the aforementioned PROMs through the applications interface. Patients without SPINEhealthie were asked to complete a questionnaire incorporating the respective PROMs.
1. Post-Surgical Follow Up
Patients were offered either traditional inpatient follow-up or virtual follow-up using our SPINEhealthie smart phone application. SPINEhealthie allows for a continuous, asynchronous remote patient monitoring. In brief, the patient can report PROMs daily and is able to contact their respective provider via a chat function. Additionally, it allows for post-operative follow-up examinations to be carried out virtually. The application collects basic demographic information such as age, gender, and body-mass-index (BMI). Procedures are named according to the AOSpine Nomenclature for Working-Channel Endoscopic Spinal procedures [19]. Participating patients gave written and informed consent and were introduced to the applications use in general as well as the chat function and image transmission process. Patients were asked to report their PROMs at different timepoints. We assessed the demographics, a visual analogue scale (NRS) for neck and leg pain and the neck disability index (NDI) as parameters for the functional outcome [19]. Patients can synchronize their stepping data with the application as well. For patients without SPINEhealthie, the postsurgical PROMs were acquired through the electronic patient chart.
2. Surgical Techniques
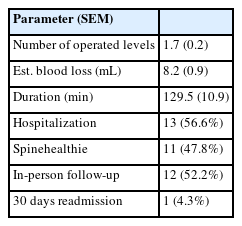
All procedures were performed by the same, experienced surgeon as previously described [20]. In brief, all patients underwent general anesthesia. Subsequently, electrophysiological monitoring was set up and recorded throughout the entire procedure. Monitoring included motor evoked potentials and somatosensory evoked potentials. The patients were positioned in a prone position the patient’s head was secured with Mayfield® head holders. Through anterioposterior (AP) and lateral fluoroscopic guidance, mediolateral and rostrocaudal approach trajectories were determined. For CE-ULBD, saline at room temperature is used for irrigation. Fluid is delivered to the working area with precise control of the flow rate and hydrostatic pressure by a specialized fluid pump (VersiconÒ, Joimax). Our initial default settings are 40 mmHg of pressure at a rate of 0.4 L/min for cervical decompression surgery. In order to correct for bed height and patient size, the endoscope is raised approximately 50 cm above the surgical field, which should result in cessation of flow. The irrigation pressure is then adjusted accordingly using the “level” function on the fluid pump. The vertical skin incisions at the previously located and marked locations were carried out using a #11 blade. After careful, blunt preparation of the subcutaneous layers, serial dilators were advanced on the lamina followed by tubular retractors. We then brought the endoscope (iLESSYS® Pro, Joimax® Inc, Irvine, CA), with a 4.7 mm working channel diameter and 7.3 mm outer diameter. Paraspinal muscles were dissected using a Bovie cautery. The laminectomy was performed using a 3.5 mm diameter diamond burr and a #3 Kerrison rongeur. The yellow ligament was resected piecemeal using both micro punch and rongeur. An adequate decompression was confirmed by the identification of the ipsilateral thecal sac and dural pulsations. Analogously, the contralateral side was decompressed using the same working channels via an over-the-top decompression. Upon completion, the wound was copiously irrigated, and meticulous hemostasis was obtained with gelfoam powder and the radiofrequency probe. No wound drainage was inserted post-surgery(Figure 1).
Intraoperative images during FESS. The initial endoscopic view depicts the juxtaposed edges of the index level laminae (lam) with connective tissue in between (A). A hemi-laminotomy is initiated by drilling along the juxtaposed edges of the laminae (B). The ipsilateral spinal cord is decompressed once the hemi-laminotomy is completed (C). The spinous process is generously undercut with the high-speed burr and yellow ligament is resected piecemeal using a micropunch (D) and Kerrison rongeur (E). Complete circumferential decompression of the dorsal thecal sac is achieved (F). FESS: fully endoscopic spinal surgery.
*= dura, lam = lamina, y = yellow ligament, sp = spinous process
3. Statistical Analysis
Continuous variables were analyzed as means±standard error of the mean (SEM). Categorical variables are depicted as frequency distributions or fractions of total (%). Repeated measurements were compared using a paired-samples t-test. For categorical variables, simple logistic regression and a multiple logistic regression adjusted for age and gender were performed. Statistical calculations were carried out and graphs designed using GraphPad Prism (Version 9.5.0; GraphPad Software, Boston, MA 02110; ©2023).
RESULTS
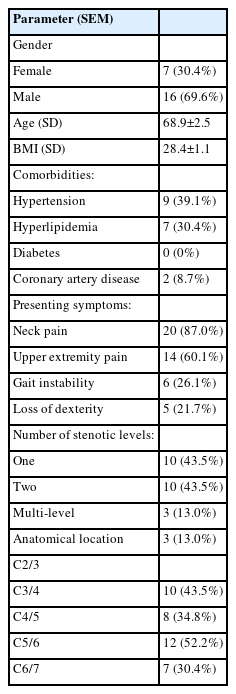
Our patient cohort included a total of 23 patients (7 female, 16 males) with a mean age of 69.1±2.5 and a BMI of 28.4± 1.1 (Table 1). Patients presented with a variety of symptoms. The main complaints were neck pain (87.0%), gait instability (26.1%) and dexterity impairment (21.7%). Pre-operative imaging revealed single- (43.5%), bisegemental (43.5%), and multilevel stenosis (13.0%) with C5/6 being most affected (Table 1).
All patients tolerated the CE-ULBD surgery well. On average, 1.7 spinal levels were decompressed, and the duration of the surgery was 129.5±10.9 minutes (Table 2). The estimated blood loss was minimal with 8.2±4.2 mL. One patient with extremely severe spinal stenosis, had reduction of her motor evoked potentials, and displayed a transient post-surgical neurological deficit that subsided within the first month after surgery. No other surgical complications were reported.
None of the patients suffered from postoperative deterioration or new permanent neurological deficits. Same day discharge was feasible in 43.4% of our patients. In our cohort 56.5% of patients elected to stay overnight in the hospital. The longest post-operative hospital stay was 2 days. One patient with active polysubstance abuse returned to the emergency department 12 days after surgery for a femur fracture that required surgery. Eleven patients in our cohort opted for virtual follow-up using SPINEhealthie smartphone app [23].
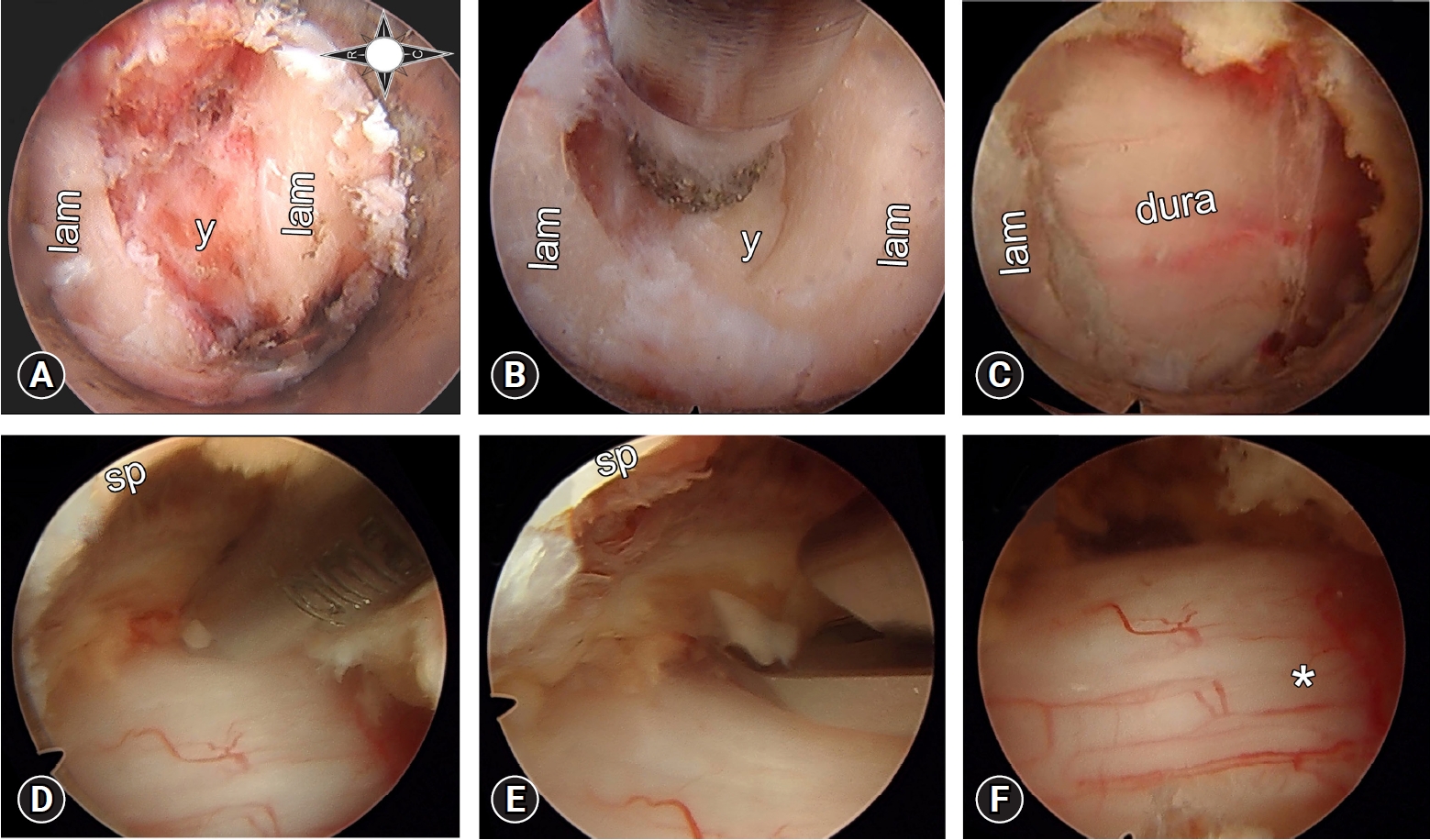
At the last point of follow up 15.6±2.4 weeks after the surgery, patient enjoyed a significant decrease in the neck pain compared to baseline (4.1±0.6 vs. 2.3±0.5; p<0.0001). Additionally, there was a significant decrease in the pain for the upper extremity (2.6±0.6 vs. 1.1±0.3; P = 0.0012; Figure 2). Importantly, CE-ULBD resulted in significant improvement of the neck disability index (18.6±2.5 vs. 9.1±2.5; p=0.032). Univariate logistic regression revealed a significantly lower rate for post-surgical hospitalization (p=0.0002) and in-person follow-ups (p<0.0001) for patients using the SPINEhealthie app. Objective pre- and postoperative stepping data was available for 4 patients (Figure 2). When compared to the pre-operative baseline, the patients displayed a tendency towards improved function as indicated by an increase in mean daily steps from 4,054±2,177 to 4,247±2,082.
Patient outcomes. The graphs depict the postoperative pain development for the first week after surgery. For the first 3 days, a significant increase in both upper extremity (p<0.0001) (A), and neck pain (B), can be seen. At the last point of follow-up, a significant decrease in pain when compared to the preoperative baseline is seen for both upper extremity pain (p=0.0005) (A), and neck pain (p=0.01) (B). (C) The graph shows patients’ weekly average stepping data (n=4, with the standard error of the mean) relative to their 90-day preoperative stepping average (interrupted line). Reported are the first 12 weeks post-surgery.
DISCUSSION
1. The Surgeon’s Perspective
FESS has been successfully utilized for decades. Unilateral laminotomy for bilateral decompression has shown excellent results in the lumbar spine, effectively relieving leg and back pain while improving functional outcomes [23-25].
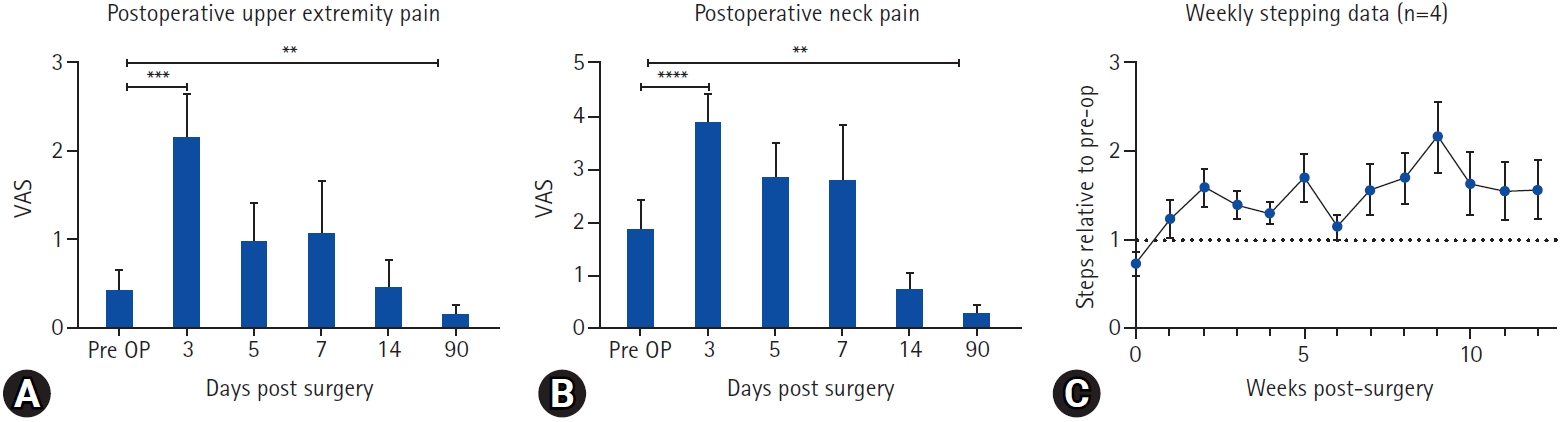
For the cervical spine, the bilateral decompression via unilateral laminotomy constitutes a relatively recent treatment strategyFigure 3. The paramedian technique we propose, as previously described, allows for a safe approach while easing the surgeon’s anatomical orientation [20]. During the surgical spinal cord decompression, the integrity of the spinal cord needs to be protected by the surgeon. Any accidental advancement of the tubular retractor, endoscope or tool onto the spinal cord could results in irreversible neurological deficits. In our series, one patient experienced transient post-operative neurological deficits. In conclusion, we believe that, if conducted by an experienced FESS-surgeon, this procedure poses a safe alternative to other, traditional techniques. Additionally, FESS offers several benefits when compared to the traditional, open procedures, as it has been described as less invasive, preserves spinal stability allowing to omit stabilization [26], and shows favorable results regarding complication rates [18]. Additionally, here we propose that stepping data might constitute a promising tool to monitor post-surgical progress objectively and continuously.
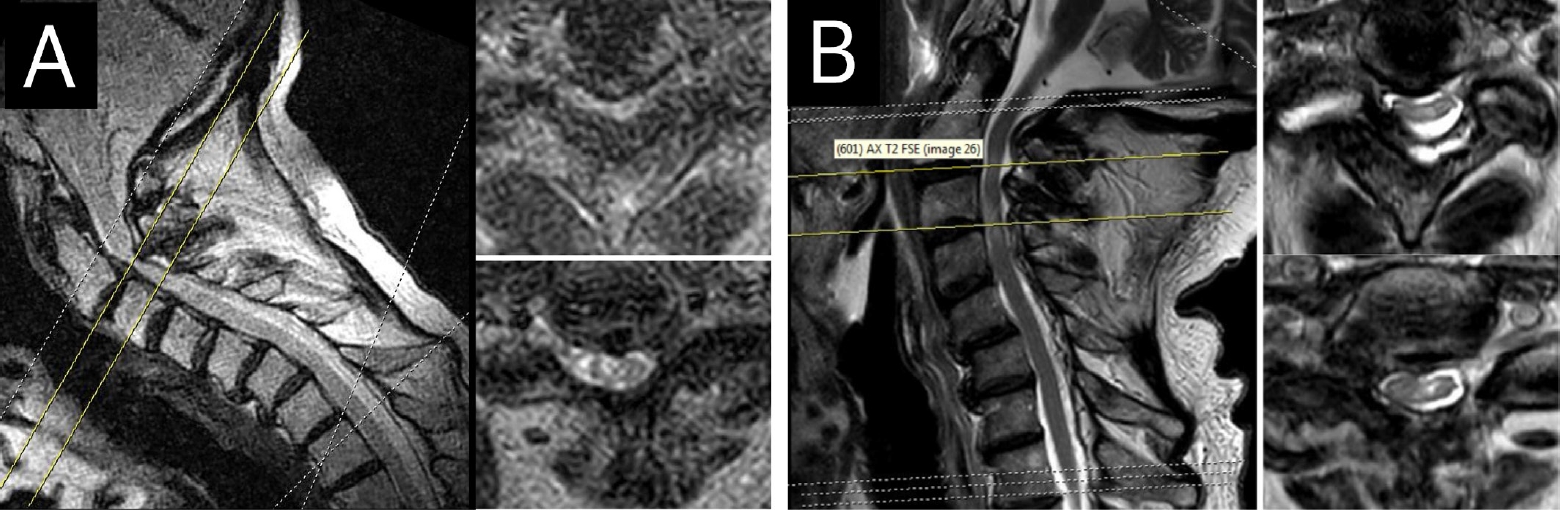
Magnetic resonance imaging (MRI) before and after cervical decompression. Depicted is an MRI scan of a patient with cervical two-level spinal canal stenosis at the C2/3 and C3/4 junction with T2-signal changes of the spinal cord. Cross-sectional images show (A) stenosis (B) and images of the same patient after CE-ULBD. The decompression can be seen directly and indirectly, as indicated by the patency of the subarachnoid space. CE-ULBD, cervical endoscopic unilateral laminotomy for bilateral decompression.
2. The Patient’s Perspective
Our results highlight the efficacy of CE-ULBD in significantly reducing the reported pain scores for the included patients in both neck and upper extremity. While there is a significant increase in the pain-levels within the first three days after surgery, the short-term functional outcomes as evidenced with significantly better NDI-score and a tendency towards better mobility, are encouraging for both the patient and the surgeon. While continuous physical therapy and self-reliant exercises are still imperative, we strongly believe that patients can benefit from our full endoscopic approach that mitigates some disadvantages of traditional spine surgery. Importantly, CE-ULBD is a minimally invasive outpatient procedure and is thought to have little effect onto adjacent motion segments. If necessary, traditional surgical options such as disc arthroplasty, anterior cervical discectomy, or fusion or posterior traditional decompression and stabilization remain viable treatment options in case additional treatment of the index level is necessary.
3. The Hospital’s Perspective
As surgeons, we strive to do what we believe is best for our patients. Considering limited resources in every healthcare system, simultaneous efficiency and mindfulness are required, too. Outpatient treatment after spine surgery has been shown to be cost effective when compared to inpatient treatment options [27,28]. With the focus on the lumbar spine, an influx in ambulatory surgeries has been described over the last decades without a simultaneous rise in postsurgical complications [29,30]. While some authors describe the safety of outpatient treatment after anterior cervical spine surgery [31,32], data concerning the posterior approach is lacking. Our study suggests no increase in clinic utilization after outpatient surgery. In fact, we show a significant decrease in clinic utilization after the introduction of the SPINEhealthie app, indicating that a continuous virtual patient monitoring post-surgery is an effective tool to optimize the clinics resources without putting patient’s safety at risk. The safety of the proposed procedure is underlined by the extremely low rate of emergency room utilization post-surgery in our group. In fact, outpatient treatment has been linked to a lower emergency room department utilization [33]. Lastly, the reduction of in-clinic visits is favorable from an economic standpoint and more convenient for the patient [34]. In fact, the COVID pandemic and the concomitant difficulties in providing in-patient visits, highlighted the necessity for a paradigm shift with possibilities for safe, virtual follow-ups.
4. Limitations
Main limitation of this study is the small cohort size. Moreover, it is a single center single surgeon study. Our ongoing efforts collect PROMs and mobility data in several academic centers using the SPINEhealthie app.
CONCLUSION
The presented data highlights the safety and effectiveness of the CE-ULBD in combination with virtual follow-ups. Importantly, we propose objective stepping data as a possible method to monitor postoperative recovery.
Notes
Ethical statements
Not applicable.
Conflicts of interest
No potential conflict of interest relevant to this article.