Full Endoscopic Interlaminar Contralateral Lumbar Foraminotomy for Recurrent L5-S1 Foraminal-extraforaminal Stenosis: A Case Report with a Technical Note
Article information
Abstract
After endoscopic lumbar foraminotomy, decreased disc height commonly causes foraminal restenosis and accompanying lateral recess stenosis. Interlaminar contralateral endoscopic lumbar foraminotomy can be used to treat multiple recurrent lesions instead of fusion surgery. Dorsal foraminal-extraforaminal decompression is challenging because of severe perineural adhesions. Therefore, neural decompression should be focused on the ventral foraminal expansion along the virgin dissection plane between the exiting nerve root and ventral foraminal pathologies. The prominent bony spur and herniated disc were removed using an endoscopic drill and forceps. As the foramen was enlarged, the endoscope was introduced deeper through the caudal-ventral foramen space to explore the extraforaminal and far-out lesions. Postoperatively, neurological deficits of L5 radiculopathy and radiating leg pain improved. The expanded foraminal-extraforaminal space was well maintained without progression of lateral wedging on the one-year follow-up images. We successfully treated recurrent foraminal-extraforaminal stenosis and combined lateral recess stenosis using the full endoscopic interlaminar contralateral approach at the L5-S1 level. This technique may be an alternative surgical method to treat the recurrent foraminal-extraforaminal stenosis in the collapse of the L5-S1 neuroforamen. However, this technique should be considered in highly selected patients unsuitable for fusion operations.
INTRODUCTION
The lumbar exiting nerve roots (ENR) pass through the neuroforamen below the pedicle and superior articular process (SAP), then curve downward in the far-out area. ENR entrapment in the foraminal and extraforaminal areas is usually caused by a hypertrophied ligamentum flavum and enlarged facet joints. The prominent syndesmophytes and herniated disc also compress the ENR from the ventral region and distort the ENR course in the far-out area.
The lumbar paraspinal or transforaminal endoscopic approach is commonly used to resolve foraminal and extraforaminal stenosis if conservative treatment fails. As the disc height decreases after foraminotomy, lateral recess stenosis develops, and restenosis of the foraminal-extraforaminal area occurs. These combined lesions cause the symptom recurrence, and a lumbar fusion operation is usually performed to resolve the recurrent ENR compression and combined lateral recess stenoses. However, lumbar fusion surgery is occasionally inappropriate for old, medically debilitated patients, and alternative surgical options are considered to treat combined and recurrent pathologies.
An advancing endoscopic approach was recently developed to treat contralateral coexisting lateral recess stenosis and foraminal and extraforaminal stenosis via a unidirectional interlaminar contralateral approach using full endoscopy and biportal endoscopy [1-3]. This technique showed favorable outcomes in the lumbar levels and reported more benefits at the L5-S1 level [3-5].
We successfully performed a full endoscopic interlaminar contralateral lumbar foraminotomy as an alternative surgical option to treat combined lateral recess stenosis and recurrent foraminal-extraforaminal stenosis in an elderly patient with severe medical problems. Expanded spaces at the lateral recess and foraminal and extraforaminal areas were well maintained in the one-year follow-up images without progression of lateral wedging.
This study was approved by the institutional review board (approval No. 2202-W03).
CASE REPORT
1. Case Presentation
An 82-year-old male presented with a 10-month history of gradually progressive motor weakness in his right leg. The patient complained of radicular pain in the right leg through the L5 dermatome despite 5 months of conservative treatment. He showed intermittent neurogenic claudication after 10 minutes of walking. Magnetic resonance imaging (MRI) and computed tomography (CT) showed lateral recess stenosis at the right side of the L4-5 level and foraminal-extraforaminal stenosis at the right side of the L5-S1 level (Figure 1A–F). Due to lateral recess stenosis, the patient underwent full endoscopic decompressive laminotomy at the right side of the L4-5 level (Figure 1G). A full endoscopic transforaminal approach was also performed at the right side of the L5-S1 level to treat the foraminal and extraforaminal stenosis (Figure 1H–M). Preoperative symptoms significantly improved after the surgery. There was no recurrence of symptoms during the three-year follow-up period. However, he revisited the hospital because of a recurrence of the symptoms that gradually progressed in his right leg. Despite 5 months of conservative treatment, the patient complained of buttock and radicular pain in the right leg through the L5 and S1 dermatomes. Neurological examination revealed hypesthesia of the posterolateral aspect of the lower leg. The motor power of his ankle dorsiflexion decreased to grade 4 (out of 5). MRI and CT revealed lateral recess stenosis and restenosis of the foraminal-extraforaminal space on the right side of the L5-S1 level (Figure 2A–G). In his past medical history, the patient had type 2 diabetes mellitus, hypertension, cerebral lacunar infarction, and coronary vascular disease. He had undergone two stent procedures for coronary vascular disease 1 year after the first decompressive surgery. This patient refused lumbar fusion surgery because of a previous history of cardiovascular and cerebrovascular diseases. Furthermore, revision transforaminal surgery for foraminal-extraforaminal restenosis might cause severe ENR injury. Therefore, we recommend a full endoscopic interlaminar contralateral approach to simultaneously treat coexisting contralateral lateral recess and foraminal-extraforaminal recurrent stenoses (Figure 2H–N).
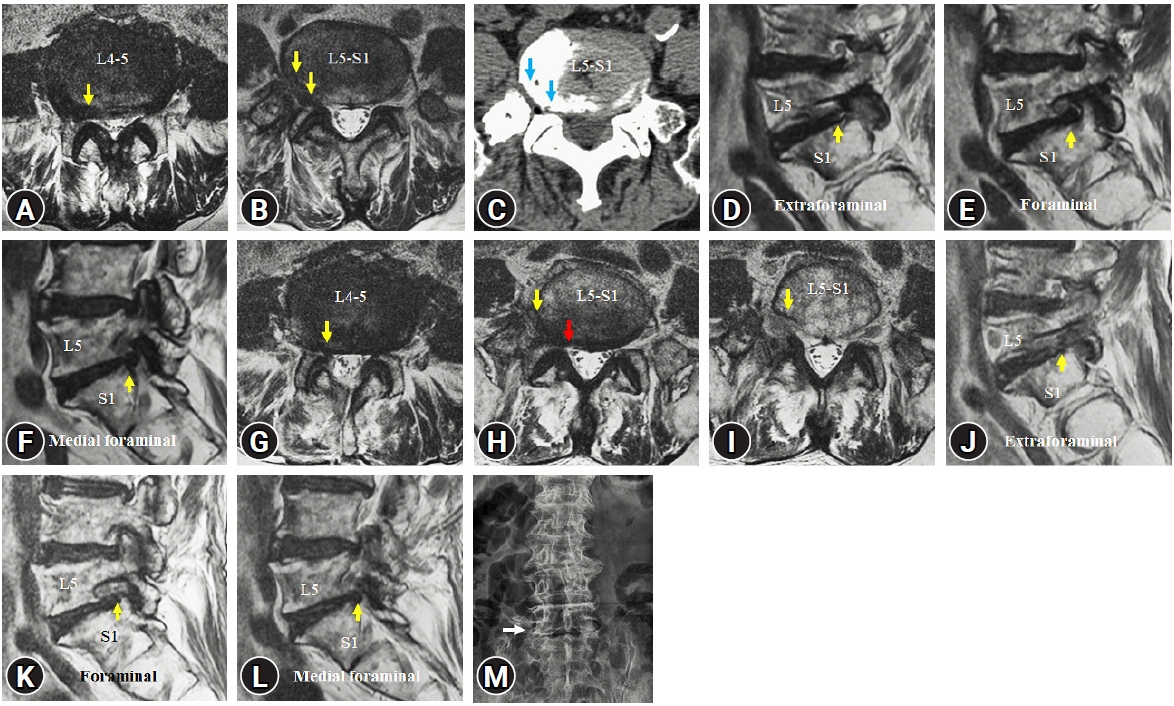
Pre and postoperative images for the initial operation at the L4-5 and L5-S1 levels. (A) Preoperative magnetic resonance imaging (MRI) shows lateral recess stenosis at the right L4-5 level. (B, C) Preoperative MRI and computed tomography images reveal foraminal, extraforaminal, and far-out stenosis at the right L5-S1 level. (D–F) Foraminal sagittal MRI documented the prominent bone spur and herniated disc in the foraminal and extraforaminal areas. (G–I) Lumbar endoscopic lateral recess decompression was performed for the L4-5 level, and transforaminal endoscopic lumbar foraminotomy was performed for the L5-S1 level using the full endoscopic system. Postoperative MRI axial images show lateral recess decompression at the right L4-5 level and foraminal-extraforaminal (yellow arrows) decompression at the right L5-S1 level. Medial foraminal stenosis was not resolved (red arrow). (J–L) Postoperative foraminal sagittal MRI reveals decompressed foraminal and extraforaminal areas (yellow arrows) by removing the dorsal foraminal lesions. However, bone spur and herniated disc at the ventral foraminal space have remained. (M) Lateral wedging is minimal on the postoperative X-ray image.
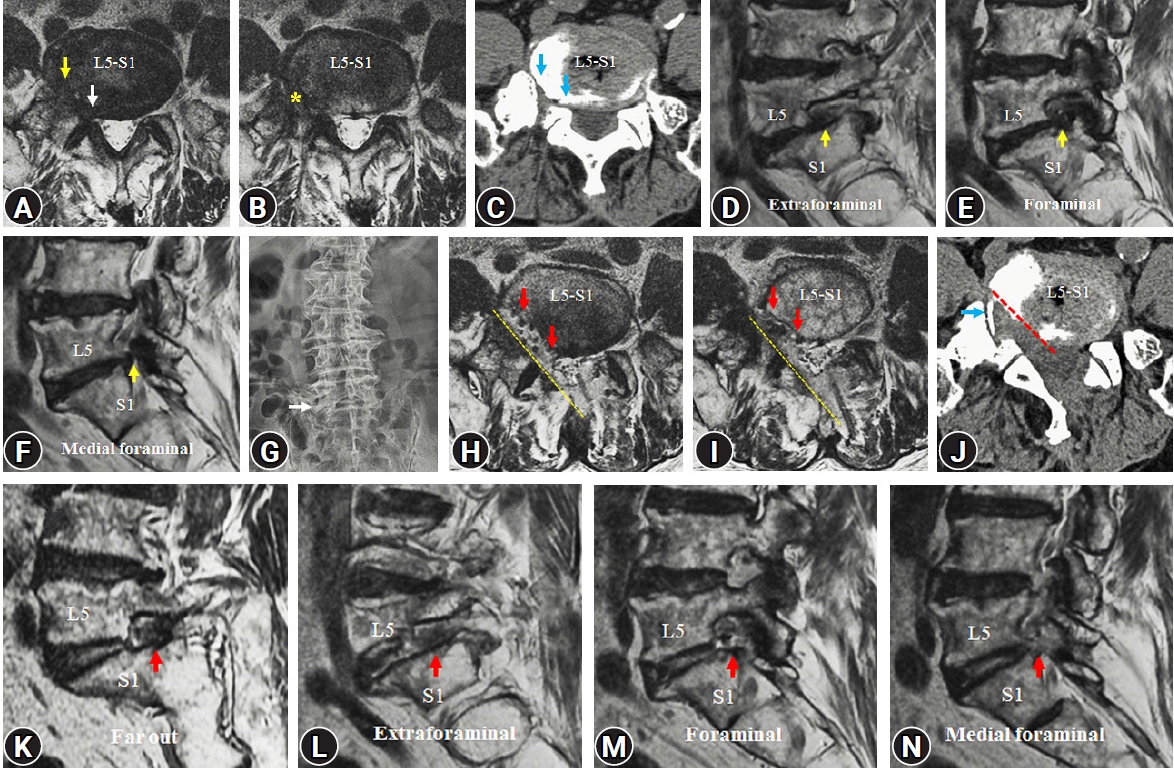
Pre and postoperative images for the revision surgery for the recurrent foraminal-extraforaminal stenosis at the right L5-S1 level. (A–C) Preoperative magnetic resonance imaging (MRI) and computed tomography (CT) images reveal severe stenosis of the foraminal, extraforaminal, and far-out areas (yellow arrow). The previous surgical tract (yellow asterisk) is unclear due to the restenosis. Bone spur in the ventral foraminal area has grown, inducing recurrent stenosis of the foraminal-extraforaminal area (blue arrows). Lateral recess stenosis has combined at the right L5-S1 level (white arrow). (D–F) Foraminal sagittal MRI shows recurrent stenosis without a perineural fat signal at the foraminal and extraforaminal areas. The exiting nerve root (ENR) is compressed by the bone spur and herniated disc (yellow arrows) and entrapped by the adhesion tissues. (G) Lateral wedging has not aggravated for 3 years after the initial foraminotomy on the X-ray image. We performed the full endoscopic interlaminar contralateral approach to resolve the contralateral lateral recess and recurrent foraminal-extraforaminal stenoses simultaneously through one surgical direction. (H, I) Postoperative MRI axial images reveal sufficiently decompressed lateral recess, foraminal, and extraforaminal area (red arrows) at the right L5-S1 level. The tract of the endoscopic approach is documented along with the sublaminar space and dorsal foraminal space (yellow dotted lines). (J) On the CT axial image, the ventral foraminal free area is created by bone spur removal and partial vertebrotomy (yellow dotted line) while preserving the facet joint. Some part of calcified adhesive tissue covering the nerve has remained at the far-out area (blue arrow). (K–N) On the sagittal foraminal MRI images, ventral foraminal pathologies are entirely removed, and remarkable neural decompression was obtained from the medial foraminal to the far-out areas (red arrows). Far-out stenosis is resolved by making the free space under the nerve root, and the natural downward course of the nerve root is restored (red arrow in K).
2. Operation Technique
A full endoscopic interlaminar contralateral approach was performed with the patient in the prone position on the Wilson frame under epidural anesthesia. The full endoscopic system, 15° viewing angle, 10-mm outer diameter, 6-mm working channel, 125-mm working length and 13.7-mm outer diameter working cannula (iLESSYS Delta; Joimax, Karlsruhe, Germany) was used for contralateral lateral recess decompression. A 2-cm skin incision was made on the medial border of the facet joints at the target level. After serial dilation, the working cannula was inserted and docked at the spinolaminar junction of the ipsilateral side, and contralateral sublaminar drilling was performed to create a sublaminar space up to the contralateral medial part of the foramen. The thickened ligamentum flavum in the contralateral lateral recess and medial foraminal region were removed using endoscopic forceps. The contralateral S1 nerve root was decompressed, and the medial part of the facet joint was exposed.
Subsequently, we changed to a smaller diameter endoscope with a viewing angle of 30°, an outer diameter of 7.3 mm, a 4.7-mm working channel, and a total length of 251 mm (TESSYS; Joimax) to pass the narrow foraminal area (Video 1). The medial part of the SAP was drilled, and the foraminal ligamentum flavum was removed to expose the ENR and entire disc height (Figure 3A). The hypertrophied annulus and prominent bony spur were removed using an endoscopic 3.0-mm diamond drill and forceps to expand the foraminal space and access the extraforaminal region (Figure 3B, C). After drilling the remaining overlying SAP (Figure 3D), a severely compressed ENR was found, entrapped by a prominent bony spur, hypertrophied annulus, and thick adhesion tissues (Figure 3E).
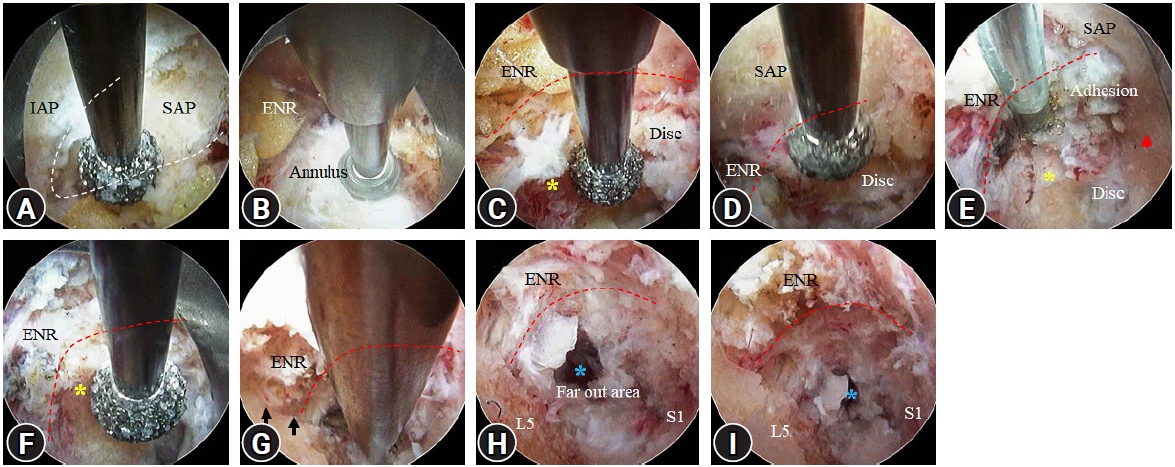
Intraoperative views of right-sided full endoscopic intralaminar contralateral approach for the recurrent contralateral foraminal-extraforaminal stenosis at the L5-S1 level. (A) Drilling the medial part of the superior articular process (SAP) to expose the foraminal space. (B) After identifying the exiting nerve root (ENR) and foraminal herniated disc, annulotomy was performed using the endoscopic drill. (C) Drilling of the prominent bone spur (yellow asterisk) and removal of the herniated disc. (D) Drilling of the SAP base part to open the extraforaminal space. (E) The ENR is entrapped by the adhesive tissue, bone spur, and herniated disc in the extraforaminal area. Partial vertebrotomy (red arrowhead) is necessary to expose the extraforaminal and far-out lesions. (F) Extraforaminal bone spur (yellow asterisk) was removed with an endoscopic drill to create sufficient space for instruments to access the far-out area. (G) The undersurface of the ENR (black arrows) is confirmed after removing the bone spur. Far-out residual bone spur and soft tissues are removed using the cutting rongeur. (H, I) After completing the far-out decompression, open space into the retroperitoneal space is exposed (blue asterisks). ENR restored its natural downward course without distortion.
Decompression of the dorsal aspect of the foraminal-extraforaminal space is challenging because of severe perineural adhesions (Figure 3E). However, virgin tissue and perineural fat were maintained below ENR. Therefore, neural decompression focuses on ventral foraminal expansion along the virgin dissection plane between the ENR and ventral foraminal pathologies. The ventral foraminal bone spurs were removed using an endoscopic drill to create additional space for neural decompression and instrument access (Figure 3F). This free space decreases foraminal pressure and enables the identification of a dissection plane between the ENR and hypertrophied annulus. Subsequently, the secured herniated disc and calcified annulus were removed using forceps and a cutting rongeur (Figure 3G).
With the enlargement of the foramen, the endoscope was introduced deeper through the caudal-ventral foramen to explore extraforaminal and far-out lesions. The ENR starts to curve downward at the extraforaminal area and is squeezed by the SAP base part and a bone spur in this patient with a collapsed neuroforamen. Therefore, bone drilling should be extended to the SAP base and foraminal portion of the lower-level pedicle to release the extraforaminal part of the ENR. If neural decompression is insufficient, partial vertebrotomy can help secure extra space along the path of ENR. Subsequently, the endoscope was carefully advanced into the far-out area, where the ENR was pressed and distorted by the prominent bone spur. Detailed bone drilling is limited to the far-out area due to the drill bit's long tract. Therefore, after thinning the bone spur, the remaining spur was removed using a cutting rongeur and forceps to expose the opening to the retroperitoneal area (Figure 3H). Finally, the ENR was entirely decompressed, and a natural downward path from the extraforaminal to far-out regions was restored (Figure 3H, I).
3. Result
Postoperatively, the motor weakness in the right leg improved from grade 4 to 4+. The radiating pain and neurogenic claudication in the right leg also improved remarkably. The patient experienced mechanical right buttock pain while straightening his back for two months after surgery, which was relieved with conservative treatment. Postoperative MRI and CT images showed sufficient decompression of the lateral recess and foraminal-extraforaminal areas (Figure 2H–J). The caudal and ventral portions of the foraminal-extraforaminal space were expanded by removing the bone spur and herniated discs. Far-out stenosis was also resolved with partial vertebrotomy (Figure 2K–N).
There were no recurrent symptoms of radiculopathy except for intermittent right buttock pain during the 12 months of follow-up. Preservation of the foraminal-extraforaminal expanded space was confirmed in the one-year follow-up MRI and CT images (Figure 4). Sufficiently expanded space created by drilling the SAP base and pedicle prevents restenosis and symptom recurrence (Figure 4D–G).
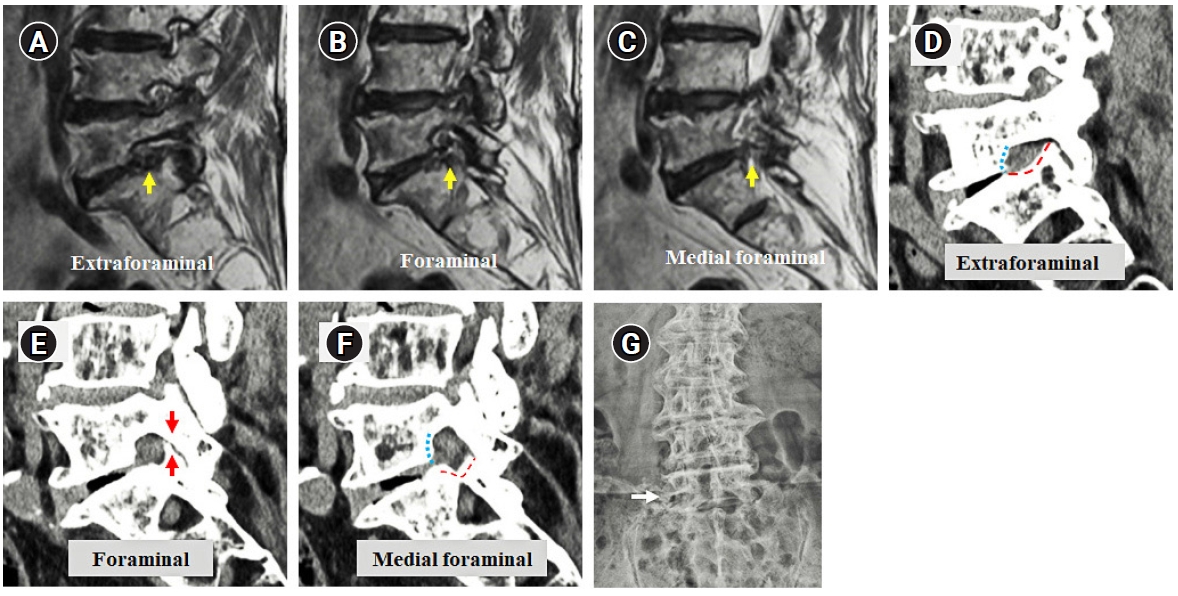
One-year follow-up images. (A–C) On the foraminal sagittal magnetic resonance imaging, expanded spaces in the foraminal and extraforaminal areas have well-maintained (yellow arrows). (D–F) A computed tomography image reveals well decompressed foraminal space after removing the bone spur (blue dotted line) and partial vertebrotomy (red dotted line). Propping structures prevent further foraminal height loss (red arrows). (G) Lateral wedging is not worsened in the X-ray image (white arrow).
DISCUSSION
The paraspinal or transforaminal endoscopic approach is commonly used to treat lumbar foraminal and extraforaminal stenoses. In cases of severe osseous lumbar foraminal stenosis, sufficient bone spur removal at the ventral foraminal area can induce postoperative dysesthesia due to excessive retraction of the dorsal root ganglion during ventral foraminal decompression [4]. These difficulties are pronounced at the L5-S1 level because it has a high iliac crest, inclination of the disc space, and wide facet joints overlapping the disc space [3]. Therefore, bony spurs and calcified herniated discs occasionally remained during transforaminal endoscopic lumbar foraminotomy at the L5-S1 level. As the disc height decreases after foraminotomy, lateral recess stenosis is combined, and the remaining ventral foraminal pathologies can accelerate symptomatic foraminal restenosis. Furthermore, the growing syndesmophytes in the far-out area induce additional neural compression and distort ENR.
In this case of the L5-S1 level, fusion operation is usually performed to resolve the recurrent neural compression and combined lateral recess stenosis because revision foraminotomy can induce serious ENR injury, and excessive facet resection is necessary during the additional lateral recess decompression. However, fusion surgery is occasionally unsuitable for elderly patients with serious medical problems owing to invasive procedures. Alternative minimally invasive surgical approaches are necessary to achieve sufficient neural decompression in these patients. Fortunately, the newly advanced interlaminar contralateral endoscopic lumbar foraminotomy (ICELF) has shown a favorable surgical outcome in treating contralateral coexisting lateral recess and foraminal-extraforaminal stenoses [2,3]. This technique is effective at all lumbar levels and more beneficial at the L5-S1 level with a wide facet joint, longer foraminal length, and inclination of the disc space [3,5]. Furthermore, several patients with recurrent foraminal stenosis have been successfully treated using the ICELF technique [4].
The dorsal aspect of the foraminal-extraforaminal area is full of severely adhesive tissues, and the ENR is entrapped by the hypertrophied SAP, prominent bone spur, and herniated disc from the caudal-ventral aspect. Revision surgery of the transforaminal approach through the previously operated tract can cause serious neural injury because of the unclear dissection plane between the ENR and adhesion tissues. Furthermore, excessive neural retraction is necessary to remove ventral foraminal lesions during the revision transforaminal endoscopic approach.
However, during ICELF, a small-diameter endoscope passes the collapsed neuroforamen through the caudal-ventral foraminal space while exploring the underlying ENR. Although severe adhesion tissues cover the dorsal aspect of the ENR, the virgin dissection plane with peridural fat is maintained at the ventral portion of the ENR. Therefore, ventral foraminal pathologies, including bone spurs and herniated discs, can be successfully removed along the virgin dissection plane without nerve root retraction. Sufficient free space is created under ENR, and this space enables adequate neural decompression and prevents restenosis even in the collapsed foramen.
The patient in this study had far-out stenosis caused by a growing syndesmophytes and hypertrophied ala bone. The ENR was compressed, and the downward course was distorted. Far-out stenosis had to be resolved for complete neural decompression. Therefore, extensive bone drilling was performed, including the syndesmophytes and cranial part of the S1 vertebrae, to create sufficient space under ENR. However, removing the ala bone from inside the neuroforamen is challenging. This free space resolved the far-out stenosis and played a role in preventing restenosis.
In the collapsed neuroforamen, the cranially migrated SAP contacts the upper-level pedicle or base part of the inferior articular process (IAP) and acts as a propping mechanism to prevent a further decrease in foraminal height. ICELF procedures do not remove the propping structures, such as the tip of the SAP and the caudal part of the isthmus or IAP. Instead, neural decompression was focused on the ventral foraminal-extraforaminal area, and sufficient additional spaces were obtained by removing the bony spur and partial vertebrotomy. These mechanisms may cause delays in restenosis and lateral wedging. This patient did not experience a recurrence of L5 radiculopathy during a one-year follow-up. In addition, the expanded foraminal and extraforaminal spaces were well preserved, and lateral wedging did not progress in the one-year follow-up images (Figure 4). However, this propping mechanism may not prevent foraminal restenosis in cases with preserved disc height. As disc height decreases, restenosis worsens inevitably, even after ICELF is performed.
Another advantage of ICELF is the simultaneous treatment of combined lateral recess stenosis while minimizing facet violation. The outer facet joint capsule and covering soft tissues are not injured during ICELF because contralateral lateral recess stenosis is decompressed by obliquely undercutting the medial part of the facet joint while the endoscope passes through the sublaminar space. A preserved facet may help to prevent postoperative segmental instability. However, if ipsilateral medial fenestration is performed for lateral recess stenosis, excessive facet resection is unavoidable because the lateral facet is resected during the previous foraminotomy procedure.
For successful ICELF without complications, surgeons should have sufficient experience with endoscopic lumbar decompression for ipsilateral and contralateral spinal canal stenosis and the endoscopic transforaminal approach for foraminal stenosis. Extensive experience with ICELF is also essential to performing ICELF for restenosis, especially at the L5-S1 level. Radicular arterial bleeding obscures the endoscopic view and causes incomplete decompression and nerve root injuries. The tract of the radicular artery should be identified and coagulated using a radiofrequency (RF) probe before removing lesions close to the ENR. However, the aggressive use of RF probes can induce nerve root injury and postoperative dysesthesia. Hemostasis is very difficult if segmental arterial bleeding occurs in the far-out area beyond the endoscopic view, and uncontrolled bleeding can induce a retroperitoneal hematoma. Preventive coagulation of vessels using the RF probes is critical to prevent retroperitoneal arterial bleeding during far-out decompression. After opening the far-out space, saline infusion pressure should be reduced to prevent retroperitoneal fluid collection.
Although this technique has impressive advantages, revision ICELF surgery should only be an alternative surgical option in highly selected patients. If recurrent lumbar foraminal-extraforaminal stenosis is combined with lateral recess stenosis, fusion surgery should be performed first instead of ICELF, especially at the L5-S1 level. Furthermore, ICELF is not recommended if segmental instability is found on preoperative radiographic images.
CONCLUSION
We successfully treated recurrent foraminal-extraforaminal and combined lateral recess stenoses using the full endoscopic interlaminar contralateral approach at the L5-S1 level. The endoscopic system moves parallel to the ENR while ensuring sufficient free space below the ENR. This technique may be an alternative surgical method to treat the recurrent foraminal-extraforaminal stenosis in the L5-S1 neuroforamen collapse. However, technical ability and surgical experience can affect surgical outcomes and should be considered in highly selected patients unsuitable for fusion operations.
Notes
Ethical statements
This study was approved by the institutional review board (approval No. 2202-W03).
Conflicts of interest
No potential conflict of interest relevant to this article.
Supplementary Materials
Supplementary Video 1.
Left-sided full endoscopic interlaminar contralateral approach for the contralateral lateral recess stenosis and foraminal-extraforaminal restenosis. (https://doi.org/10.21182/jmisst.2022.00528.v001).