INTRODUCTION
Fusion surgery has been golden standard of surgical treatment for various diseases of lumbar spine. The achievement of a solid fusion mass is major goal of fusion surgery to prevent the adverse outcomes associated with fusion failure. Among many graft materials for spinal fusion, autologous bones obtained from iliac crest have been proven with the most successful, but also have a possibility of complications with regard to harvesting. Accordingly, the development of safe and effective graft substitutes has been required.
Since introduced commercially in 2002, recombinant human bone morphogenetic protein-2 (rhBMP-2), has become one of the most commonly used bone graft substitutes world widely. However, while numerous papers have demonstrated that rh-BMP2 enhances fusion success rates, there also have been concerns about the occurrence of related complications, specifically including the development of ectopic bone formation, postoperative radiculitis, and endplate osteolysis [5,8,11-13,21,25]. And, it has been highly speculated that those complications related to rh-BMP2 would be proportional to the dose used. Several authors have suggested that higher dose of rh-BMP2 may induce more complications [6,7,13].
In Korea, the use of BMP in the spinal surgery area has been available since the mid-2010s by introducing first domestically produced rh-BMP2, which is Bio-BMP2 (Cellumed. Korea). Bio-BMP2 consists of rh-BMP2 obtained through Chinese Hamster Ovary (CHO)-cell culture and demineralized bone matrix (DBM) that acts as a carrier. This product has a prominently small dose of BMP (0.05 mg/mL) compared to other products such as INFUSE (Medtronic, Memphis, TN) (1.5 mg/mL).
The authors have used this rh-BMP2 (Bio-BMP2) with since November 2015, and report its safety and efficacy by evaluating clinical and radiographic outcomes of the lumbar interbody fusion including posterior lumbar interbody fusion (PLIF) and oblique lateral interbody fusion (OLIF).
MATERIALS AND METHODS
From November 2015 to September 2017, total 279 patients underwent lumbar interbody fusion surgery including PILF and/or OLIF using rhBMP-2 in our institute (Seoul St. Mary’s Hospital, Seoul, Korea) by single surgeon (K.S. Ryu), except the contraindications (Table 1). Among them, 199 patients who could be followed up more than 12 months were enrolled in the present study and a retrospective review was performed, including clinical records, plain X-ray, and CT scans.
Surgical procedure: PLIF procedure was performed by miniopen standard manner. An extensive laminectomy with facetectomies was done in all patient. After bilateral annular windows were made, complete discectomy was carried out. The entire nucleus and cartilaginous end plates were removed using pituitary forceps, curettes, and reamers with preserving the bony end plates. By placing gradually bigger dilators into the collapsed disc, disc space was restored to enough height. The proper cage size for target disc was determined according to normal disc height of the adjacent segments. Ogival interbody cages (OIC: Stryker Howmedica Osteonics, Mahwah NJ, USA) were filled with morselized bone chips from the removed lamina and facets. Bio-BMPs is made of pre-filled type. It was applied to the top and bottom surfaces of the cage with 0.05mg per each level (Figure 1). Two cages of the same type were inserted bilaterally in the target disc. Their position was assessed intraoperatively with C-arm fluoroscopy, then the remaining bone chips were placed outside of the cage. Finally, transpedicular screws fixation was carried out by using ZENIUS™system (Medyssey, Korea).
OLIF procedure was carried out in the following steps. Under C-arm fluoroscopic guidance, a skin incision was made in 6-8 cm in front of the center of the target disc. After the serial dissection of three layers of abdominal muscles, the retroperitoneal space was identified. The window between the inferior vena cava or left common iliac vein and anterior border of the psoas muscle was exposed. After confirming the annulus of the targeted disc, a guide pin was placed into the intervertebral disc space. A tubular retractor was docked after applying sequential serial dilators. The disc removal and endplate preparation were carried out by using shavers, curettes, and forceps. Lastly, a cage (PEEK Clydesdale®, Medtronic, Memphis, TN, USA) with the proper size was filled with DBM (AlloMatrix Injectable Putty, Wright Medical Technology, Inc, Arlington, Tenn). After applying rh-BMP2 to the top and bottom surfaces of the cage as same dose with PLIF, a cage was placed to the target disc. All procedures were performed by an orthogonal maneuver under C-arm fluoroscopic guidance. After change patient’s position to prone, the transpedicular screws fixation with or without laminectomy was conducted.
The back and leg pain outcome was assessed using visual analogue scale(VAS) score measured on a 10-point numeric rating scale. The functional outcome was evaluated using Oswestry disability index (ODI). Patient assessments were completed preoperatively and at 12 months after operations.
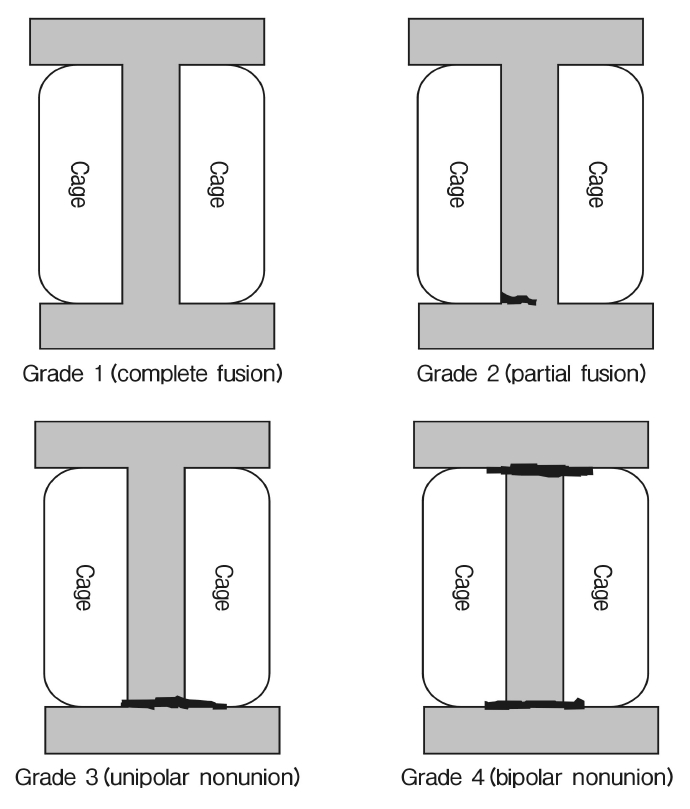
To evaluate fusion status, standing lateral and flexion-extension lateral radiographic and thin-cut 1-mm CT scans were obtained postoperatively at 12 months. In plain dynamic X-ray, fusion success was defined as continuous bone growth between the vertebral bodies and minimal translation (less than 2 mm) and minimal angulation (less than 5 degrees). Finding of the CT scan at the operated segment was classified from grade 1 to 4 (grade 1; complete fusion, grade 2; partial fusion, grade 3; unipolar nonunion, grade 4; bipolar nonunion) (Figure 2) [22]. Grade 1 or 2 was considered as fusion success. Comparing fusion success rate between the subgroups was done using t-test.
The postoperative complications related to surgical procedure were assessed. The occurrence of complications related to the use of rh-BMP2 including ectopic bone formation, postoperative radiculitis, and endplate osteolysis was observed from clinical records and imaging studies. Ectopic bone formation was defined as exhibition of new bone formation extending outside the disc space on follow up CT scans. Postoperative radiculitis was defined by worsening leg pain postoperatively in a dermatomal distribution without any compressive lesion on imaging findings. Endplate osteolysis was defined as manifestation of endplate erosions with implant subsidence.
All radiographic findings were observed on digital radiograph images displayed on a PACS (Picture Achieve and Communication System) terminal (Marosis 2003, Marotech, Seoul). The radiological assessments were performed twice by 2 independent observers. Inter- and intraobserver reliabilities of all radiological data were greater than a correlation of 0.80.
The correlation with the clinical parameters and fusion status was assessed using Chi-square test. A p-value at 0.05 was set as statistical significance. Numerical results were averaged. All numerical findings were expressed as means ±SDs. Statistical verification was determined using PASW Statistics 18 (version 18.0.0; SPSS Inc., USA). A p-value at 0.05 was set as statistical significance.
RESULTS
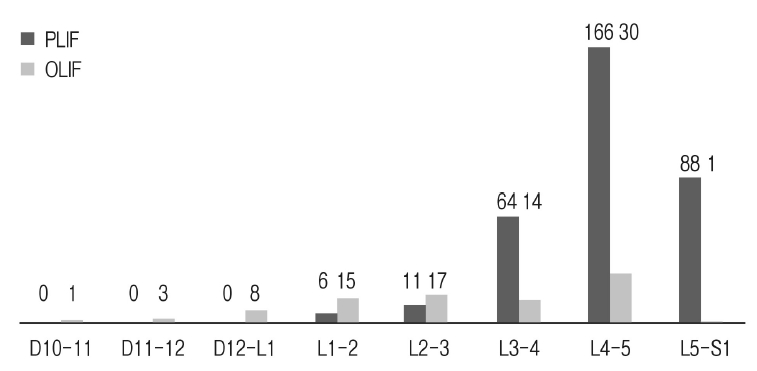
The demographics of the patients was figured out on Table 2. They are 61 men and 138 women of ages ranging from 38 to 91 years (mean age: 66.9±12.4). Total surgical levels were 424 levels. The distribution of level operated was shown in Figure 2. The number of surgical levels was listed on Table 3. Fusion methods were distributed as 164 cases of PLIF, 17 of OLIF, and 18 of combined. According to the surgical method, 335 segments were operated with the PLIF and 89 segments with the OLIF. Mean follow-up duration was 14.1±2.5 months. Mean back and leg VAS scores were significantly decreased from 7.12±2.23 to 1.45±1.63, and from 7.54±2.11 to 1.27±1.56, respectively (p<0.05). ODI scores were also decreased from 38.12±15.33 to 18.93±13.67 (p<0.05).
In plain dynamic X-rays, 406 (95.8%) of surgical levels were shown continuous bony bridge in the cages and no segmental motion at last follow up. On the last follow up CT scan, fusion grade was distributed as 330 levels of grade 1 (77.8%), 66 of grade 2 (15.6%), 22 of grade 3 (5.2%), and 6 of grade 4 (1.4%). Overall fusion success rate was found to be 93.4%. According to fusion method, in PLIF group, it was distributed as 267 levels of grade 1 (79.7%), 45 of grade 2 (13.4%), 18 of grade 3 (5.4%), and 5 of grade 4 (1.5%), and in OLIF group, 63 levels of grade 1 (70.8%), 21 of grade 2 (23.6%), 4 of grade 3 (4.5%), and 1 of grade 4 (1.1%). Fusion status of each surgical level in regard to surgical methods was shown on Table 4. L5-S1 level showed the lowest fusion success rate. Fusion success rate with regard to fusion method was appeared as 93.1% in PLIF and 94.4% in OLIF.
The statistical verification between clinical variables of the present study and the fusion status was listed on Table 5. The lower T-score, smoker, and lower level especially in L5-S1 were significantly related to the fusion failure.
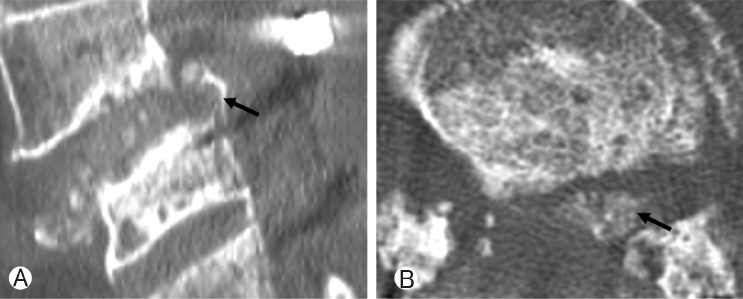
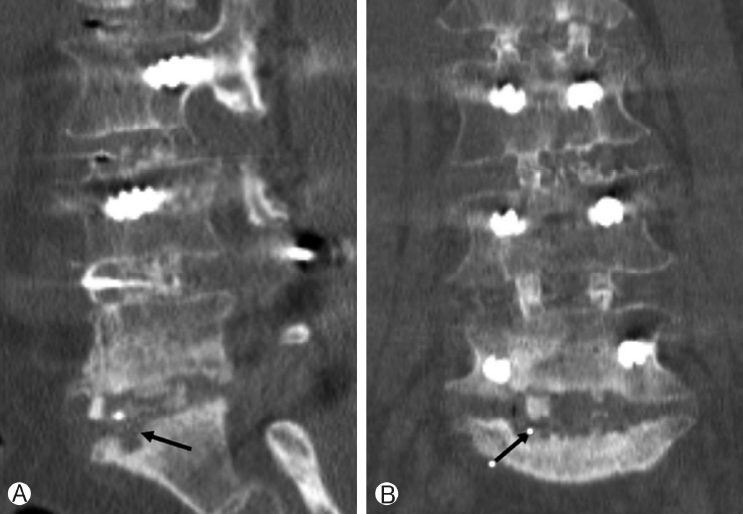
The observed postoperative complication related to surgical procedure and the use of rh-BMP2 were listed on Table 6. Fortythree patients presented newly developed leg symptoms postoperatively. However, 27 patients showed temporary symptoms and disappeared within 7 days after surgery. The remaining 16 cases were caused by a misplaced screw or a cage migration, and the symptoms were alleviated after revision surgery. No patient was suspected of having postoperative radiculitis related to the use of rh-BMP2. Two case showed ectopic bone formation behind the inserted cage, and it located into the spinal canal (Figure 4). However, there was no clinical symptom correlated with. There were 2 cases of endplate osteolysis. Those findings were observed at L5-S1 level in the cases of multiple level operations (Figure 5). One case without clinical symptom has been still observed, and the other one was required revision surgery due to continuous back pain.
DISCUSSION
The most important current issue with rh-BMP2 might be potential adverse events caused by this biologically active protein. Many previous clinical papers have reported the complications after PLIF or TLIF surgery using rh-BMP2. Carragee et al. [3] did comparative review of Food and Drug Administration(FDA) documents and subsequent publications revealed originally unpublished adverse events and internal inconsistencies. They suggested an estimate of adverse events associated with rhBMP-2 use in spine fusion ranging from 10% to 50%. Especially in PLIF, use of rh-BMP2 was strongly associated with radiculitis, ectopic bone formation, osteolysis, and poorer global outcomes. Representatively, Sethi et al. [20] analyzed radiographic and CT changes after the use of rhBMP-2 in spinal fusion surgery. They found out that the endplate resorption was observed in 82% of the lumbar levels and subsidence of the cage resulting in narrowing of the disk space in 50%. Vaidya et al. [23], also noted that 8 of the 26 patients of TLIF and PLIF required revision surgery during the follow-up period due to cage migration or disc space subsidence by endplate resorption. Wong et al. [27] reported 5 cases of ectopic bone in the spinal canal with potential neurologic compromise after PLIF/TLIF use of rh-BMP2. Rihn et al. [19] noted that postoperative radiculitis occurred in 14% of patients undergoing TLIF with rhBMP-2, but only 3% of patients with other bone graft materials. Although this postoperative radiculitis with rh-BMP2 is not clearly defined yet, the possible causes have been suggested, which includes ectopic bone [27], postoperative epidural cysts [15], seroma [17,26], inflammation of the nerve root [14]. Various techniques have been advocated for preventing adverse events following the use of rh-BMP2 in the lumbar interbody fusion surgery using cages. A physical barrier such as fibrin glue between the disc space and the spinal canal [4,16,24], placement of interbody devices with less than 3 mm of confinement within the disc space [10], or lowering the concentration and volume of rhBMP [24].
The present study showed that 2 cases of ectopic bone formation(1%, 2/199) without clinical symptoms and 2 cases of endplate osteolysis observed at L5-S1 requiring revision surgery (1%, 2/199). No patient was suspected of having postoperative radiculitis. This occurrence rate is remarkably lower than the results of previous reports. During the operation, the authors did not use the any specific techniques such as use of physical barrier or management of cage location to prevent complications related to use of rh-BMP2. Only difference from other clinical studies was that the authors had used different type of rh-BMP2, which is domestically produced rh-BMP2 product (Bio-BMP2). This product has a prominently small dose of BMP(0.05 mg/mL) compared to other products such as INFUSE (Medtronic, Memphis, TN) (1.5 mg/mL).
There has been a speculation of that the use of a higher dose of rh-BMP2 may increase the fusion success rate, but also can induce more complications. Crandall et al. [6] did a retrospective review of 509 consecutive patients undergoing TLIF with rhBMP2. They incrementally decreased the BMP dose over time from 12 to 2 mg. According to their results, there were no BMP-related complications occurring at a dose of below 4 mg per disc, and all cases showed successful arthrodesis. Mannion et al. [13] conducted a prospective observational study of 30 patients who underwent TLIF/PLIF with a low-dose rhBMP-2 (1.4 mg). They reported 97% of fusion success and observed 2 cases of asymptomatic heterotopic ossification (6%), and two cases of perineural cyst formation (6%). Moreover, although the present study did not deal with, it is known that there is cancer risk with rh-BMP2. According to systemic review attempts to summarize the cancer risk from using rh-BMP2 in spine surgery from the published peer-reviewed literature and available FDA summary, the risk of cancer with rh-BMP2 is highly dose dependent [7]. The present study using only 0.05 mg of rh-BMP2 per disc, showed remarkably low incidence of complications related to. The authors strongly conjecture that this very low-dose of rh-BMP2 could reduce the incidence of complications.
A potential concern when using lower-dose of rh-BMPs2 is whether the fusion success rate is decreased. However, according to above mentioned reports, the fusion was successful when they used a small dose of rh-BMP2. And even in the present study with much lower dose, the authors also obtained 93.4% of fusion success rate. It indicates that establishment of a dose of rh-BMP2 to help the fusion effectively and reduce the incidence of complications to a minimum may be mandatory.
There is a difference between PLIF and OLIF in regard of graft materials. Unlike PLIF, which could get autologous bones from the removed lamina and facets, OLIF usually uses synthetic graft materials due to difficulty in harvesting autologous bone. Thus, there has been concern of that this might be the reason for lowering the fusion success rate. In the present study, the authors had used DBM as graft material in OLIF surgery. Nevertheless, the result of fusion degree was not inferior to PLIF procedures. These results indicate that rh-BMP2 plays a major role in fusion success regardless of the type of graft material. It is well known that lumbosacral junction is the most heavily loaded segment and high mechanical stress is concentrated as fusion end in multilevel operation [1,9,28]. Non-union cases in the present study were mainly found out at L5-S1 level especially in multilevel operations.
There have been clear evidences of that rh-BMP2 has potent osteoinductive capabilities and enhances fusion success rate in spinal fusion surgeries [2,18]. Among several fusion methods, in the present study, the authors performed PLIF and OLIF procedures, which put a cage filled with autologous bone chips or DBM and applied with rh-BMP2. And the author has achieved an overall 93.4% of fusion success rate in minimal 12 months follow up, which is a high enough and can be compared with previous many reports.
CONCLUSION
The known complications related to using rh-BMP2 in spinal surgery is not common in the present study. Further long term observations are needed to clarify these issues of such complications. The known complications is not common in the present study, which may be caused by using low-dose rhBMP-2. Further long term observations are needed to clarify these issues of such complications.